1. Background
Menopause is a physiological transition in middle age. It is important in terms of reproductive health and personal, social, and cultural life (1). The physiological changes of this period (especially age-related physical changes, such as weight gain, menstrual cessation due to reduced ovarian activity, decreased muscle mass, reduced elasticity of the skin, redistribution of fat mass in the abdomen, and progression of obesity following the reduction of estrogen) may lead to negative experiences in body image among postmenopausal women (2, 3).
These physiological changes can exacerbate other symptoms (especially mental changes) with varying severity and weakness, including self-hatred, feelings of ugliness, loss of sexual attractiveness, exhaustion due to aging, and changes in body image (4-6). Body image is a complex phenomenon encompassing physiological, psychological, and sociological components. When a person does not have a positive body image and finds his or her appearance lower than the desirable and ideal criterion for society, he or she may face inappropriate emotions and attitudes toward oneself, such as low self-esteem and depression (2). Women are very sensitive to their body image (7); therefore, impaired body image has a large impact on social and marital relationships, daily functions, interpersonal and family relationships, and quality of life (8). Besides several interventions (such as exercise, relaxation, and group therapy) suggested for the improvement of negative body image, cognitive behavioral therapy (CBT) is widely considered to be an effective intervention (8-10). Cognitive behavioral therapy is a psychosocial intervention that focuses on challenging and changing feelings, thoughts, and behaviors to improve mental health (11) and provide an opportunity for assessment and intervention (12).
Thomas Cash identified 8 steps in CBT and conducted studies to investigate the impact of this kind of therapy on negative body image. This method is rooted in scientific psychology and reflects an active and cognitive behavioral approach to treatment (13). Controlled studies have shown that CBT can make significant changes in how a person feels about his or her body (14, 15). Moreover, positive changes that a person obtains with his or her body image can improve self-esteem and generally improve his or her psychological status (16). The majority of body image studies have focused on adolescents, and few studies have been conducted on adults and older women (17). Body dissatisfaction is more common and complex in middle-aged women than in young women (3). Erbil reported that women with an optimistic attitude toward menopause tend to have a more positive body image and lower levels of depression (18). Thomas et al showed that attractiveness is important for sexual satisfaction in middle-aged women, and supporting positive body image may help women in their midlife maintain sexual satisfaction with aging (19). Nazarpour et al showed that the body image of postmenopausal women was associated with the severity of menopausal symptoms (20).
2. Objectives
This study aimed to evaluate the effectiveness of cognitive behavioral group therapy on the negative body image of postmenopausal women.
3. Methods
A clinical trial with a pretest and posttest control group design was used in this study. Twenty-two eligible postmenopausal women aged 45 - 60 years attending a health center in Ahvaz, Iran, in 2018 were included in this study. Inclusion criteria were having a negative body image according to the body image concern inventory (BICI) (with scores higher than 57), body mass index (BMI) of 18.5 - 30 kg/m2, a minimum of 2 years having passed since menopause, having the ability to read and write, and willingness to participate in the study. The exclusion criterion was having a history of severe psychological problems before the study, identified in interview sessions held before the start of the research project.
This study was approved by the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (code: IR.AJUMS.REC.1395.453), and the study protocol was registered on the Iranian Registry of Clinical Trials website (code: IRCT2017041029964N1). The objectives of the study were explained to the participants, and written consent was obtained from all participants. Then, the BICI questionnaire was completed by the postmenopausal women who met the inclusion criteria and were willing to participate in the study. Studies have supported the efficacy of CBT on body image, with the effect size ranging from low (d+ = 0.23) to high (d+ = 1.00) (8). The sample size was determined based on the literature (21) and taking into account the total score of the body image. In this study, a significant level of 0.05, power of 90%, and attrition rate of 20% were considered acceptable. The sample size in each group was 11, and accordingly, 22 subjects were invited to the study. Training and counseling sessions were held at a health care center. Participants were randomly assigned to the intervention and control groups (n = 11 per group) using a random block method with a 1 to 1 ratio using a randomized computer-generated list. Random allocation concealment was performed, and all procedures were conducted in accordance with the Declaration of Helsinki principles. Cognitive behavioral therapy sessions were also held at a health care center. The 2 groups were evaluated by the Multidimensional Body-Self Relations Questionnaire (MBSRQ). Then, the intervention group received cognitive behavioral group therapy based on the Cash 8-step model every week.
The CBT based on the Persian translation of the Thomas Cash book (22) was designed in 8 sessions of 90 minutes. The sessions were conducted over a period of 2 months (June and July 2018) by a trained researcher (Marziyeh Hosseini) under the supervision of a psychologist.
The sessions were as follows:
Session 1: Discovering personal body image
Session 2: Understanding the origin of the body image concept
Session 3: Mindfully accepting body image experiences and implementing the mirror reflection technique
Session 4: Seeing beneath the surface of private body talk and implementing the mirror reflection technique
Session 5: Mindfully modifying mental mistakes
Session 6: Facing body image avoidance
Session 7: Erasing body image rituals
Session 8: Treating the body well
All sessions, except the eighth session, ended with a review of homework assignments and practices, as well as setting goals for the next week. No intervention was performed in the control group. After the end of the eighth session and 1 month after the therapy, both groups completed MBSRQ and BICI. To comply with ethical principles, a copy of the book was given to participants in the control group.
To collect the data, 2 questionnaires were used as the instruments of the study. These instruments are discussed in detail in the following sections.
Multidimensional Body-Self Relations Questionnaire was designed by Cash as a convenient self-reported method to evaluate body image and attitudes. This questionnaire had 46 items. In analyzing the survey data, the rating took the form of the Likert scale. Rating scales were numerically coded as (1) definitely disagree; (2) mostly disagree; (3) neither agree nor disagree; (4) mostly agree; and (5) definitely agree. The subscales included (1) appearance orientation (AO) (which is defined as the extent of investment in one's appearance and has 12 items scoring from 12 to 60); (2) appearance evaluation (AE) (which is defined as satisfaction or dissatisfaction with one's looks and has 7 items scoring from 7 to 35); (3) fitness evaluation (FE) (which is defined as feelings of being physically fit or unfit and has 3 items scoring from 3 to 15); (4) fitness orientation (FO) (which is defined as the extent of investment in being physically fit or athletically competent and has 13 items scoring from 13 to 65); (5) subjective weight (SW) (which is defined as obesity anxiety (ie, care and maintenance about weight, diet, and limited feed) and has 2 items scoring from 2 to 10); and (6) body areas satisfaction (BAS) (which is defined as satisfaction with specific areas of the body and features such as the face, weight, and muscle status; it has 9 items scoring from 9 to 45). The higher the score on MBSRQ is, the more satisfaction with the body image is indicated (23). Multidimensional Body-Self Relations Questionnaire is a well-validated measure (24) and has been used in many studies in Iran (9, 25). The psychometric properties of this questionnaire were calculated and approved in Iran by Rahati (26). They report that the Cronbach α value was 0.85 for the total of the questionnaire among 217 female subjects and was higher than 0.60 for all of the 6 subscales. They also calculated the correlation coefficient in a test-retest study with a 2-week interval on a sample of 67 individuals, indicating appropriate reliability of the scale (26).
The other tool, BICI, was developed by Littleton et al. It consists of 19 questions, and each question has 5 options. It is numerically coded from 1 (never) to 5 (always). The total points obtained from the whole 19 questions show a minimum score of 19 and a maximum of 95. Higher scores represent higher levels of body image concern (27). A score between 38 and 57 indicates the average degree of concern, and scores higher than 57 indicate a high degree of concern. The validity and reliability of the questionnaire were investigated and approved in different studies in Iran (28, 29). This questionnaire has good reliability and validity indices. Its reliability was examined by the internal consistency method, and the Cronbach α coefficient was 0.93. In Iran, Mohammadi and Sajadinejad investigated the validity of the questionnaire among 209 high school students in Shiraz by split-half and internal consistency methods, and the coefficients were 0.66 and 0.80, respectively (30).
In this study, the normality of the data was tested by the Kolmogorov-Smirnov test. The quantitative variables were described by the mean ± SD. The independent t-test, chi-square test, and Mann-Whitney U test were used to compare the groups. The Mauchly test of sphericity indicated that the assumption of sphericity was not violated (P > 0.05). Repeated measures analysis of variance was used to assess changes in each parameter during the study. P values less than 0.05 were considered statistically significant.
4. Results
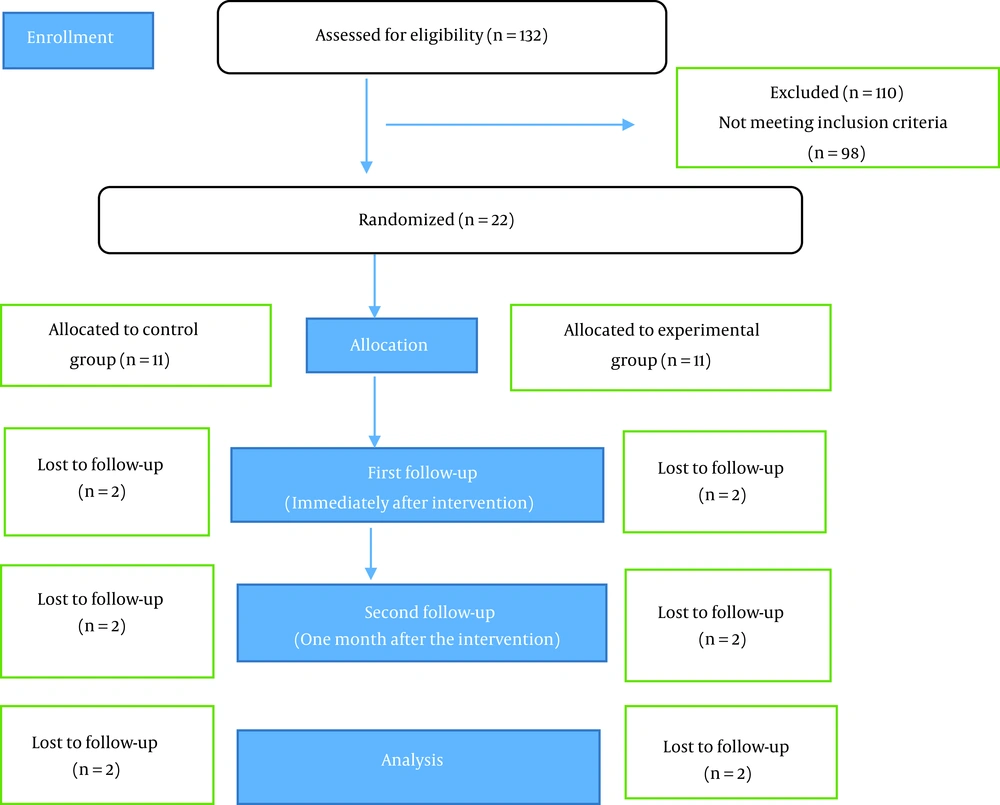
In the present study, 132 postmenopausal women attending a health center were assessed for eligibility criteria, and 22 women who met the criteria were selected and assigned to the intervention and control groups. After the loss of 2 subjects in the intervention group (due to the absence of more than 2 sessions), 2 other subjects were excluded from the control group due to the lack of cooperation. Finally, 18 patients (n = 9 per group) were regarded as the effective subjects (Figure 1). Demographic information is presented in Table 1. Both groups showed no statistically significant difference in terms of age, number of children, age of menopause, BMI, education, and economic level. The scores of MBSRQ and BICI for the pretest, posttest, and follow-up stages are presented in Table 2. Before the study, the control and intervention groups were consistent in all dimensions of MBSRQ, except for the FO subscale (P = 0.02). The results of the repeated test showed that there was a significant difference between the scales for AE, AO, and BAS in the intervention group after cognitive behavioral group therapy (P < 0.05). This effect has also been significant for a follow-up assessment after 1 month.
| Demographic Characteristics | Intervention (n = 9) | Control (n = 9) | P Value |
|---|---|---|---|
| BMI (kg/m2) | 24.6 ± 1.4 | 24.3 ± 1.2 | 0.7 b |
| Age (y) | 52.7 ± 2.3 | 51.6 ± 2.4 | 0.5 b |
| Number of children | 5.2 ± 1.01 | 4.1 ± 1.01 | 0.3 c |
| Age of menopause (y) | 48.2 ± 2.2 | 47.1 ± 2.1 | 0.21 b |
| Education | 0.1 d | ||
| Elementary | 3 (33) | 4 (44) | |
| Middle school | 2 (22) | 2 (22) | |
| High school | 3 (33) | 2 (22 | |
| University | 1 (11) | 1 (11) | |
| Family income | 0.12 d | ||
| Good | 3 (33) | 4 (44) | |
| Fair | 5 (55) | 3 (33) | |
| Poor | 1 (11) | 2 (22) |
Abbreviation: BMI, body mass index.
a Values are expressed as mean ± SD or No. (%).
b Independent t-test.
c Mann-Whitney U test.
d Chi-squared test.
| Variables and Time | Intervention Group (n = 9) a | Control Group (n = 9) a | P Value b | Effect Size |
|---|---|---|---|---|
| AE | 0.49 | |||
| Pretest | 15.5 ± 5.4 | 17.1 ± 4.05 | 0.20 | |
| Posttest | 25.02 | 17.3 ± 3.02 | 0.001 | |
| Follow-up | 27 ± 3.04 | 16.4 ± 3.1 | 0.001 | |
| P value c | 0.001 | 0.9 | ||
| AO | 0.56 | |||
| Pretest | 41.01 ± 4.05 | 42.02 ± 4.1 | 0.75 | |
| Posttest | 47.01 ± 5.02 | 43.2 ± 5.3 | 0.001 | |
| Follow-up | 49.05 ± 4.23 | 42.3 ± 5.01 | 0.001 | |
| P value c | 0.001 | 1 | ||
| FE | 0.20 | |||
| Pretest | 7.1 ± 1.02 | 7.2 ± 1 | 0.32 | |
| Posttest | 7.3 ± 1 | 6.3 ± 1.05 | 0.09 | |
| Follow-up | 7.6 ± 1.02 | 7.4 ± 1.02 | 0.09 | |
| P value c | 0.22 | 0.065 | ||
| FO | 0.29 | |||
| Pretest | 39.3 ± 5.01 | 34.5 ± 5.06 | 0.02 | |
| Posttest | 38.01 ± 5.02 | 33.4 ± 3.08 | 0.063 | |
| Follow-up | 39 ± 4.08 | 34 ± 4.1 | 0.063 | |
| P value c | 0.81 | 0.11 | ||
| SW | 0.01 | |||
| Pretest | 6.3 ± 1 | 7.3 ± 2 | 0.68 | |
| Posttest | 6.2 ± 1.1 | 7.4 ± 2 | 0.48 | |
| Follow-up | 6.3 ± 1.05 | 7.2 ± 1 | 0.48 | |
| P value c | 0.8 | 0.93 | ||
| BAS | 0.72 | |||
| Pretest | 21.01 ± 3.1 | 19.2 ± 3.01 | 0.80 | |
| Posttest | 29.01 ± 1.1 | 19.2 ± 2.02 | 0.001 | |
| Follow-up | 29.3 ± 1 | 18.01 ± 2.03 | 0.001 | |
| P value c | 0.001 | 0.62 | ||
| Total body image score | 0.63 | |||
| Pretest | 131.56 ± 9.15 | 127.8 ± 5.5 | 0.55 | |
| Posttest | 145.44 ± 7.01 | 127.4 ± 1.05 | 0.035 | |
| Follow-up | 149 ± 6.39 | 125.33 ± 6.39 | 0.035 | |
| P value c | 0.001 | 0.65 | ||
| BICI | 0.50 | |||
| Pretest | 66.3 ± 19.1 | 67.5 ± 8.2 | 0.70 | |
| Posttest | 48.2 ± 4.01 | 66.5 ± 8.3 | 0.001 | |
| Follow-up | 50.4 ± 5.02 | 67.3 ± 7.02 | 0.001 | |
| P value c | 0.002 | 0.09 |
Abbreviations: AE, appearance evaluation; AO, appearance orientation; FE, fitness evaluation; FO, fitness orientation; SW, subjective weight; BAS, body areas satisfaction; BICI, Body Image Concern Inventory.
a Values are expressed as mean ± SD.
b Independent t-test.
c Repeated measures test.
Also, analysis of the results of body image concern showed that there was a significant difference in the intervention group (P < 0.05) after the CBT sessions, which continued until follow-up.
5. Discussion
It is well-documented that body image consists of attitudinal, behavioral, and perceptual components. Cognitive behavioral therapy does not address any of these aspects in a particular way and, instead, considers the body image as a general construct and improves dysfunctional cognition (attitudinal component), reduces body avoidance and checking (the behavioral component), and reduces size overestimate (perceptual component) (31). The results of the present study indicated that CBT based on the Cash 8-step model in postmenopausal women can promote satisfaction with their body image. These results are consistent with the findings obtained in previous studies focusing on the effect of CBT on body image in different groups, such as primiparous women during the postpartum period (9), infertile women (22), women with mastectomy (32), and those with binge eating disorders (33). This method could improve AE, AO, and BAS in postmenopausal women by dealing with the dimensions of body image and enhancing them by examining the cognitive distortions and assumptions of the subject about appearance.
Improvement in the BAS subscale might be due to the teaching skills, such as regular mirroring de-sensitization, positive self-talk, and cognitive restructuring. Enhancing AO may refer to issues used in step 7, such as encouraging subjects to use positive physical activity or factors (such as wearing make-up) that give rise to more positive feelings about appearance.
Despite the significant difference in the FO subscale in the pretest, in the present study, SW, FE, and FO did not show a significant change. Failure to obtain a positive result on FE and FO subscales can be due to intensive sessions and focusing more on body details since the subjects did not have the opportunity to review and create a consistent overall picture of their own body.
Another measure that did not show a positive change was SW. This result may be due to the fact that the study did not pay particular attention to the problem of weight, as the subjects neither reported a weight problem nor experienced adverse weight conditions.
Applying the Cash model and MBSRQ has had different findings in various studies conducted on different social groups. A study conducted on primiparous mothers during the postpartum period showed that CBT could promote AE and BAS subscales, and there was no improvement in other dimensions (9); in addition, in a group of infertile women, CBT improved all dimensions except for FO and SW (22).
Another tool used in this study was BICI. It provides the body image as a general construct in 2 factors. The first factor is the person's dissatisfaction and embarrassment of his appearance and examining and concealing perceived defects. The second factor indicates the degree of interference of concern with the appearance in the social function of an individual (24). Group therapy, as well as focusing on steps 6 and 7, helped to improve the body image concern.
Considering the physical and emotional changes during menopause, it seems necessary for postmenopausal women to pay attention to their body image, and the Cash model can improve it. In this model, the focus is on perceptions, thoughts, and feelings about the body image with the aim of finding out how this image has been shaped (26).
This model emphasizes the possibility of satisfying the body, and the subjects are taught how to create opportunities to enjoy their appearance. In the process of group CBT, the main goal is to help group members identify their negative feelings and understand how their beliefs and assumptions affect their feelings and behaviors, as well as to provide other alternatives (22).
Menopausal women have significantly less positive attitudes toward their appearance and body image, which may cause low self-esteem and depression (23). Therefore, using the present method, which resulted in the improvement of body image, it is possible to prevent the occurrence of subsequent psychological problems in postmenopausal women and help them accept age-related appearance changes.
To our knowledge, the present study is the first randomized study examining the efficacy of CBT on the body image of postmenopausal women; however, it has some limitations. The sample size used in the study was small, and therefore, generalization could not be made with certainty. Another limitation was related to the use of a self-report questionnaire without taking into account the hidden private thoughts of the participants, which should be considered due to the generalization of the findings.
5.1. Conclusions
Cognitive behavioral group therapy based on the Cash 8-step model can be effective in improving the negative body image of postmenopausal women. Further studies are needed with more therapy sessions or breaking down the steps into several steps for complete and profound changes.