1. Background
Although hospital services and the system for caring for traumatic brain diseases have improved, the impact of TBI-related behavioral dysregulation, such as bullying behavior and aggression, on the occurrence of crimes remains significant. Traumatic brain injury (TBI) is a condition that results in disability and loss of years of life (1-5). While several potential mediators have been identified in previous studies (6), the role of cognitive emotion regulation as a mediator in the relationship between difficulties in emotion regulation (DERS) and current symptoms of bullying behavior and aggression is still relatively unexplored. Previous studies have examined each of these emotion regulation components independently as potential contributors to emotion regulation problems. However, the correlation between DERS and aggressive behavior has not been thoroughly investigated more generally (7). In recent years, research efforts have shifted towards identifying the elements that contribute to emotional tone. Research results have shown that individuals who use positive emotional strategies are less likely to experience depression and exhibit better adaptability. On the other hand, when individuals employ avoidance strategies, they tend to feel depressed and exhibit poor adaptability (8). Improved adaptability is associated with emotional expression. However, when emotions are not expressed, they remain unresolved, which can impact the patient's health and increase sympathetic nervous system activity (9). Given that TBI patients experience significant levels of stress and negative emotions in addition to the challenges they face, it is crucial to understand the emotional components of these patients' experiences and the strategies they employ to regulate their emotions (10). Therefore, uncovering these associations could assist in the management of the large numbers of patients with these disorders presenting to health services.
2. Objectives
Due to the limited number of studies that have examined the possible mediating variables, the current study aimed to explore the relationship between DERS, aggregation, and bullying behavior in TBI patients.
3. Methods
3.1. Participants and Procedures
This research is a retrospective cohort study using community-based samples. Information on motorcyclists who survived a full year from their first TBI was collected to allow adequate time for an outcome to occur. They were advised to visit a mental clinic at the Shahid Mostafa Khomeini Hospital in Ilam, Iran, after being contacted. A psychiatrist conducted clinical interviews with the patients. They were instructed to bring the 5 questionnaires they had been given to their next appointment. Informed consent, demographic information, and neurological information of the patients were recorded in the questionnaires. Over the 23-month period from January 2017 to March 2019, 120 motorcyclists with mild TBI participated in the current research. The inclusion criteria for this study included brain trauma patients with a GCS score between 13 and 15 years, ages 18 to 50 years, willingness to participate in the study, no history of mental illness (such as bipolar disorder, personality disorder, severe psychosis), and no mental retardation, smoking, drug use, or alcohol consumption.
The exclusion criteria included non-cooperation in completing the questionnaire, moderate and severe traumatic injuries, and a previous history of head injury. The questionnaires were coded without including first and last names and were only marked with acronyms (A, B, C) to protect the participants' privacy and prevent the disclosure of their names.
3.2. Questionnaires
3.2.1. The Cognitive Emotion Regulation Questionnaire (CERQ)
The CERQ is a 36-item scale with 9 subscales. For our analysis, we summed the CERQ-M and CERQ-A strategies (11).
3.2.2. Bullying Behavior
The initial Olweus questionnaire is an abbreviated questionnaire comprising 28 items. Its validity and reliability have been confirmed in several studies, with a test-retest reliability estimated using Cronbach's alpha coefficient as 0.83 (12).
3.2.3. Impulsive and Premeditated Aggression Scale
The Impulsive and Premeditated Aggression Scale (IPAS) (13) consists of 30 items for reporting aggressive acts over the past years. It has been used in various populations, including community adult samples (14, 15).
3.2.4. Difficulties in Emotion Regulation Scale
This questionnaire was developed by Gratz and Roemer (2004) and comprises 36 items rated on a 5-point Likert scale. In a study conducted by Shafiei et al. (2016), the tool's reliability was confirmed as 0.89 using Cronbach's alpha (16).
3.3. Data Analysis
Descriptive statistics were reported as mean ± standard deviation (SD). Correlation coefficients were used for normally and non-normally distributed variables, respectively. The mediating variables were CERQ-A and CERQ-M sub-scores from the CERQ.
After completing the questionnaires, the data were analyzed using SPSS AMOS software. Structural equation modeling based on the maximum likelihood method was applied to study the components of emotion regulation in patients with mTBI.
The most common statistical indices for evaluating the fit of the structural model, including the absolute fit (chi-square, CMIN), fit indices (root mean square error of approximation (RMSEA), normalized fit index (NFI), comparative fit index (CFI), and Bentler-Bonett normed fit index (NFI)), and the Tucker-Lewis index (TLI), were all calculated. If the chi-square is not statistically significant, it indicates an appropriate fit for the model. However, this indicator tends to be significant in larger samples and is not considered an appropriate index for model fit. Values close to 1 for the TLI, NFI, and CFI indices, values greater than 0.5 for the normalized fit index, and values less than or equal to 0.05 for the RMSEA index all indicate a good fit.
4. Results
4.1. Demographics and Psychiatric Symptoms
In the present study, 120 participants were included, with an average age of 34.00 ± 11.56 years. Of the participants, 61.6% were married, 35.5% were single, and 3.3% were divorced (Table 1).
| Variables | No. (%) |
|---|---|
| Marital status | |
| Married | 74 (61.6) |
| Single | 42 (35) |
| Divorced | 4 (3.3) |
| Education level | |
| Illiterate | 10 (8.3) |
| High school | 55 (45.83) |
| High school diploma | 30 (25) |
| Bachelor's degree | 20 (16.66) |
| Master's degree | 3 (2.5) |
| PhD | 2 (1.6) |
a Values are expressed as No. (%).
Table 2 summarizes all the information, including means, SDs, and ranges. The overall mean score for bullying behavior was 13.3 ± 0.63. In this sample, 32.4% of participants met the cut-off for mild bullying, 41.8% for moderate bullying, and 25.8% for severe bullying behavior. The mean scores for CERQ-M and CERQ-A were 53.48 ± 11.0 and 70.1 ± 13.31, respectively. The overall mean score for aggression was 7.24 ± 5.87. In this sample, 23.8% of participants met the cut-off for mild aggression, 39.7% for moderate aggression, and 36.5% for severe aggression.
| Characteristics | Mean (SD, Range) % |
|---|---|
| Bullying behavior | 13.3 (0.63, 3.66) |
| Maladaptive cognitive emotion regulation strategies (CERQ-M) | 53.48 (11, 57) |
| Adaptive cognitive emotion regulation strategies (CERQ-A) | 70.1 (13.31, 67) |
| Difficulties in Emotion Regulation Scale (DERS) | 112.6 (21.8, 56.2) |
| Aggregation | 7.24 (5.87, 19) |
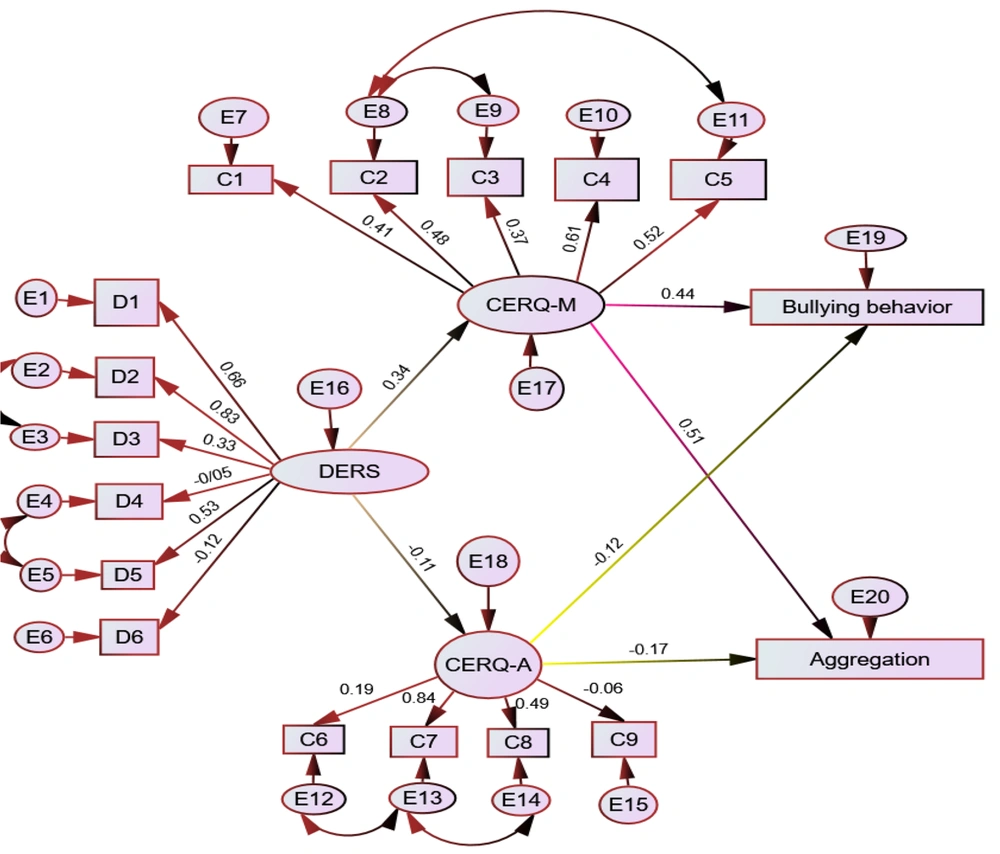
By fitting the structural equation model and the final model, the fit indices for chi-square (CMIN = 10.762, df = 15, P = 0.096 > 0.05), Tucker-Lewis index (TLI = 0.857), comparative fit index (CFI = 0.943), and Bentler-Bonett normed fit index (NFI = 0.932) were obtained. Additionally, the value of the normalized fit index (PNFI) was 0.725, and the RMSEA was 0.031. These values indicate that the model fits the data well. Table 3 displays the regression coefficients for the obtained model.
| Paths | Non-standard Coefficients | Standard Coefficients | Standard Deviation | Critical Region | P-Value |
|---|---|---|---|---|---|
| CERQ-A → DERS | -1.151 | -0.110 | 0.104 | 0.178 | 0.000 |
| DERS → CERQ-M | 1.054 | 0.340 | 0.215 | 0.103 | 0.000 |
| CERQ-M → C1 | 1.238 | 0.410 | 0.416 | 0.370 | 0.000 |
| CERQ-M → C2 | 1.255 | 0.462 | 0.229 | 0.263 | 0.000 |
| CERQ-M → C3 | 0.912 | 0.374 | 0.416 | 0.350 | 0.037 |
| CERQ-M → C4 | 1.311 | 0.611 | 0.514 | 0.629 | 0.002 |
| CERQ-M → C5 | 0.983 | 0.522 | 0.281 | 0.415 | 0.000 |
| CERQ-A → C6 | 0.541 | 0.193 | 0.168 | 0.167 | 0.031 |
| CERQ-A → C7 | 7.512 | 0.842 | 0.401 | 0.113 | 0.000 |
| CERQ-A → C8 | 1.863 | 0.494 | 0.112 | 0.329 | 0.000 |
| CERQ-A → C9 | -0.712 | -0.063 | 0.341 | -0.563 | 0.110 |
| DERS → D1 | 1.210 | 0.663 | 0.514 | 0.510 | 0.000 |
| DERS → D2 | 1.110 | 0.843 | 0.203 | 0.563 | 0.000 |
| DERS → D3 | 1.168 | 0.331 | 0.517 | 0.143 | 0.000 |
| DERS → D4 | -0.074 | -0.054 | 0.342 | -0.329 | 0.231 |
| DERS → D5 | 1.103 | 0.538 | 0.161 | 0.313 | 0.000 |
| DERS → D6 | -0.181 | -0.121 | 0.109 | -0.370 | 0.013 |
| CERQ-M → Bullying behavior | 1.311 | 0.441 | 0.154 | 0.629 | 0.002 |
| CERQ-M → Aggregation | 0.983 | 0.512 | 0.281 | 0.415 | 0.000 |
| CERQ-A → Bullying behavior | -0.541 | -0.123 | 0.168 | 0.617 | 0.031 |
| CERQ-A → Aggregation | -7.512 | -0.172 | 0.401 | 0.311 | 0.000 |
Based on the results presented in Table 3, all the factors related to emotion regulation, cognitive adjustment, and emotional adjustment were significant at a 5% error level (P < 0.05). Furthermore, there was a significant correlation between the components of cognitive and emotional regulation and maladaptation at the 1% error level, with a correlation coefficient of 30% (P < 0.01).
Figure 1 illustrates the final structural model for measuring the emotional adjustment variable. In this model, the emotional adjustment variables, along with the components of cognitive emotion regulation that are compatible and incompatible with Bayesian symbols and the dimensions of their measurement with rectangular symbols, are displayed.
5. Discussion
Traumatic brain injury is defined as an injury that disrupts the brain's normal functioning, often caused by shaking, impact, or head contact. Due to the intricate interplay between acute (short-term) and long-term changes in quality of life following a brain injury, complications arising from traumatic brain injuries and their effects have garnered significant attention. Recently, there has been an increased focus on the prevalence of psychiatric illnesses as outcomes following traumatic brain injuries (17). This study investigates the mediating role of maladaptive and adaptive emotional regulation in the relationship between DERS, bullying behavior, and aggression among TBI patients.
The study demonstrates a significant correlation between DERS, aggression, and bullying behavior with cognitive mediation. Additionally, structural equation modeling analysis reveals that patients with maladaptive cognitive processes have difficulty in regulating their emotions, contributing to increased emotional turmoil. In general, both maladaptive and adaptive cognitive processes can predict difficulties in emotional control, aligning with previous research findings (18, 19). It appears that in the absence of adaptive regulation, patients may resort to impulsive and maladaptive regulation methods.
Furthermore, the findings indicate an indirect correlation between DERS and adaptive cognitive processes. Patients who do not struggle with adaptive cognitive regulation experience more positive emotions, higher self-esteem, and better psychological adaptation. Positive emotions serve as essential psychological resources, enabling individuals to employ coping strategies against psychological stress, maintain physical health, and confront stressful life events (20).
The role and impact of emotional regulation on various mental disorders have been explored in previous studies (21, 22). These studies have shown a connection between emotional regulation and anger. Individuals with stable emotional regulation tend to experience fewer negative emotions, such as anger and irritability. They manage their emotions before becoming overwhelmed and avoid situations that may trigger negative emotions.
It has been revealed that people may face challenges in controlling their emotions for various reasons. This research suggests that the inability to control emotions can be linked to both compatible and incompatible cognitive-emotional adjustment components (23, 24). Consequently, enhancing emotional control in patients with brain injuries can involve identifying, modifying, and replacing components of emotional regulation. Furthermore, addressing the emotional aspects of traumatic brain injuries through psychological therapy can help patients overcome the challenges posed by this condition. This study is the first to examine the elements of both adaptive and incompatible cognitive-emotional regulation in traumatic brain injuries.
A primary limitation of our study was the limited sample size and the lack of similar studies that comprehensively addressed the generalizability of the results. Therefore, to strengthen the findings of this study, further research within the field is strongly encouraged.
Based on the study's results, it is recommended that psychological interventions be developed to teach emotion regulation strategies as part of the therapeutic protocol for TBI patients. This could help prevent the recurrence of traumatic events. Additionally, research should be designed and conducted to assess the effectiveness of these interventions in TBI patients, aiming to determine the precise role of these components.