1. Background
Phenylketonuria (PKU) is a congenital metabolic disorder caused by a deficiency or dysfunction of the enzyme phenylalanine hydroxylase (PAH), which disrupts the conversion of phenylalanine (Phe) to tyrosine. If the disease is not diagnosed at birth and treatment is not started according to the child’s needs, high levels of Phe in the patient’s blood plasma lead to nerve injury, brain abnormalities, mental retardation, epilepsy, and behavioral problems (1). Treatment includes strict adherence to a controlled and restricted diet with low protein to maintain blood Phe levels within the specified range to prevent neurological problems caused by the disease (2).
1.1. Parents with PKU Children
Carpenter et al., in examining the specific parenting experiences of parents of children with PKU, identified three following trends:
(1) From the moment the disease is diagnosed, the parents should continuously monitor the amount of Phe in the child’s blood, and regardless of emotional reactions, the parents will learn that the child’s growth depends on the proper management of the disease by them.
(2) Social situations related to food, including parties, increase the anxiety and stress of parents and require constant attention and care to ensure that children do not consume forbidden food.
(3) Despite the concerns related to these problems, some parents adapt to these conditions and adjust their lives according to the requirements of treatment and care of a child with PKU, and after successfully achieving and controlling the disease, they witness the child’s normal development. These parents accept PKU as a part of their and their children’s normal lives. However, some parents do not accept the diagnosis of PKU and are not able to bear the pressure caused by the feeling of shame and social labeling and experience more negative emotions related to the feeling of mourning (stigma), especially denial, anger, and depression before acceptance. These parents consider PKU disease as a threat to their child, and this problem can disrupt the natural process of adaptation to the diagnosis of the disease (3).
In general, the limited diet and the possible risk of mental retardation impose a heavy burden on the family and affect their mental well-being. This is one of the reasons that parents suffer from a high level of anxiety and stress. Moreover, in addition to severe dietary restrictions, possible factors affecting parents’ stress, including limitations in daily activities, cognitive disabilities, learning and behavioral problems of the patient, numerous visits to the doctor, and repeated sampling of Phe level, were mentioned. The difficulty in having access to and preparing Phe-free products due to the low economic status of the family can be one of the most important factors related to parental stress. Managing a patient with PKU is very time-consuming and costly for the family, even in countries where the economic situation is stable (4). Because in Iranian culture, individuals are highly emotionally dependent on their families, parents of children with PKU are more likely to suffer from social, economic, and emotional problems that are often limiting, destructive, and comprehensive essentially (2).
1.2. Perceived Social Support and Self-compassion for Parents of PKU Children
The perception of social support and individuals’ attitude toward the support received is more important than the amount of support provided, which is called perceived social support and plays a significant role in dealing with stressful events. The members of the network providing the perceived support, who are often the family and close friends of the person, are effective in reducing the isolation and increasing the coping capacity of the person (5).
There are two hypotheses about the major effect of social support as an effective factor in coping with stressful events and health-promoting behaviors. Firstly, the experience or perception of receiving social support as a rewarding experience creates a positive feeling of being cared for and loved. It causes mental health and, consequently, physical health. Secondly, social support acts as a stress buffer and indirectly reduces the negative effects of stressful events and reduces the consequences and impacts of stressful events. In other words, perceived social support can be effective in individuals’ adaptation and coping with major health stresses by improving the functioning of the immune system and reducing stress (6).
Studies have shown that, along with social support, individuals receive high compassion from others, and this becomes a protection against stress. Compassion not only from others in the form of social support but also from the person himself/herself in the form of self-kindness has an extensive background in reducing the negative effects of stressful events. Therefore, increasing social support might provide the guidance and security needed to develop self-regulatory skills, such as self-compassion (7, 8). The compassion, safety, reciprocity, and a sense of common humanity that comes from positive relationships and social support increase adaptive strategies for emotional regulation and effective coping and make it possible to improve mental well-being (9).
1.3. Link Between Self-compassion and Distress Tolerance
One of the variables influencing distress tolerance is emotion regulation (10). Emotion regulation means processes or methods that individuals use to adjust their emotions when facing a negative situation (11). Self-compassion, as an emotion regulation mechanism, is responsible for the role of shock absorber and support against symptoms of anxiety, depression, and rumination (12, 13). Neff first conceptualized the construct of self-compassion. Self-compassion includes 3 main components, namely self-kindness versus self-blame, human commonality versus isolation, and mindfulness versus extreme assimilation or avoidance (13). From the point of view of Gilbert, the founder of compassion-focused therapy, compassion itself is a motivational system designed to regulate negative emotions and has a special psychological activation pattern. Self-compassion is a healthy introspective attitude in times of personal distress and suffering that facilitates more adaptive emotion regulation through self-soothing (14). Self-compassion is a multidimensional construct that includes components for identifying and acknowledging suffering, having a non-judgmental attitude, and creating motivation to alleviate suffering (15). Individuals with high self-compassion perform better in activating the soothing system and deactivating the threat-defense system (14) and by keeping difficult emotions in awareness and accepting them unconditionally from avoiding or exaggerating the experience (16).
The results of previous studies showed that high levels of self-compassion and mindfulness predict lower levels of parental distress. The sense of self-acceptance, along with compassion, has led to a reduction of self-criticism and self-condemnation in mothers, and the ability to consider their experiences in the framework of common human experience can become a sense of connection with others and avoid exaggerating problems. This not only leads to the relief of negative emotions by creating coping skills but is also useful in the mental well-being of mothers. Additionally, mothers can be emotionally available and responsive to their child’s needs (17). Self-compassion has a significant positive relationship with life satisfaction, hope, and goal readjustment, and it was inversely related to depression and parenting stress (18).
Distress tolerance is the term used in clinical psychology research to encapsulate the concept of how an individual stands for aversive internal psychological states (19). Distress tolerance often refers to an individual’s perceived ability to withstand negative or unpleasant emotional states (e.g., physical discomfort) and the behavioral ability to persist in the face of internal states of distress provoked by certain stressful situations (20). Theoretically, distress tolerance might affect or be influenced by some self-regulatory processes, including attention and cognitive appraisals of distressing emotional or physical states; for example, individual differences in the experience of emotions, both their intensity and frequency, might influence the nature of distress tolerance (19). Individuals with lower levels of distress tolerance might be prone to maladaptive responses to distress and threatening situations. As a result, these individuals might try to avoid related negative emotions/annoying states. Conversely, individuals with higher levels of distress tolerance might be more able to respond adaptively to distress and perform behavioral reactions caused by resilience and tolerance against various types of stressors (21).
Baker and Hoerger consider parental distress to be one of the things that affect the relationship between parents and children. Reducing the level of distress tolerance is one of the important psychological symptoms in families with sick children, which is manifested in the ability to analyze psychological situations. The disturbance might be the result of physical and cognitive processes; however, its representation is in the form of negative emotional states, which are often manifested by the desire reaction to get rid of the negative emotional experience. Individuals with low mental distress tolerance evaluate the experience of emotional disturbance as exhausting and unacceptable; as a result, they try to relieve this negative emotional state. Nevertheless, most of the time, they are not able to focus their attention on anything other than their distress (22). Decreased levels of distress tolerance might be associated with maladaptive responses to stress, including avoidance of negative affect. Those with low distress tolerance tend to show more impulsivity and leave difficult tasks faster. As parents, low distress tolerance might jeopardize daily interactions and have long-term effects on the child’s development (23, 24).
Gilbert defines distress tolerance as “the ability to control, stay with, and tolerate complex and high levels of emotion rather than avoiding, deflecting, shutting down, contradicting, invalidating, or denying them with fear” (25). Low levels of distress tolerance combined with avoidance and a need to escape run counter to what we all seek in our lives and desire to share with others. Self-compassion, acceptance, and understanding of inner suffering might be the key to freeing parents to truly and fully participate in the moment-to-moment experience of emotions for the best performance and the best quality of inner life experience (26).
It seems that perceived social support can have a protective effect as a source of support in facing a stressful event. The role of psychological self-care, that is, self-compassion along with perceived social support, will be important in facing the impact of the event (26, 27).
2. Objectives
The current study, different from the recent research, has examined two internal support sources of self-compassion and the external support source of perceived social support simultaneously. More specifically, the present study sought to examine the following research hypnosis:
(1) Perceived social support has a direct pathway to self-compassion.
(2) Self-compassion has a direct path to distress tolerance.
(3) Perceived social support through self-compassion has an indirect pathway to parenting distress tolerance of parents with a PKU child.
3. Methods
3.1. Study Design
This study is among descriptive designs of correlation type using the structural equation modeling (SEM) method. Considering that PKU is a rare metabolic disease (prevalence of 1 in 10,000 births in the world/1 in 5,000 births in Iran) and has a different distribution in the provinces of Iran (1), the statistical population of this study included 195 parents who had the child with PKU (based on the medical diagnosis file), received dietary products (without Phe), and was covered by the support center for metabolic patients in Zanjan province, in 2021. Due to the rarity of PKU disease and the small number of diagnosed cases, the number of samples was chosen according to this statistical population.
3.2. Participants
A total of 157 parents of children with PKU and covered by the Association for the Support of Metabolic Patients of Zanjan Province were selected as the research sample by the targeted sampling method. The criteria for entering the research included the necessity of being the biological parents of the child with PKU, receiving food products without Phe from the Association for the Support of Metabolic Patients of Zanjan Province, and having at least one child within 2 - 18 years with PKU disease, at least a high school education, and no serious psychiatric illness in the parent of the participant in the research. The exclusion criteria were the completion of the questionnaires by someone other than the parents and the lack of willingness and cooperation of the parents to participate in the study.
3.3. Procedure
At first, by obtaining the necessary permits and coordinating with the management of the Zanjan Metabolic Patient Support Charity, referrals to this Institute and the medical files of patients with PKU were evaluated. Parents who had a child with PKU were asked to participate in the study by completing the questionnaire electronically. The electronic packages containing the questionnaires of the current study were sent to the participants through social networks and email with informed consent. After completing the forms, they were sent to the researchers individually by each of the parents. To comply with ethics in the study, parental consent was obtained to participate in the study. Additionally, the research objectives were explained, and they were assured that their information would remain confidential and there was no need to include names. This study was approved by the Institutional Review Board of Behavioral Research and Surveys of the University of Mohaghegh Ardabili, Ardabil, Iran.
3.4. Instruments
3.4.1. Self-compassion Scale
The Self-compassion Scale (SCS) was compiled based on Neff’s conceptualization of the construct of self-compassion. It consists of 26 items and measures three bipolar components in the form of six subscales of self-kindness (5 items) versus self-judgment (5 items), common humanity (4 items) versus isolation (4 items), and mindfulness (4 items) versus over-identification (4 items). Answers are placed on a five-point Likert scale from almost never (1) to almost always (5) (28). The internal consistency of the scale with the Cronbach’s alpha method was reported from 0.89 (mindfulness) to 0.91 (over-identification). Re-test reliability was also reported as 0.92 after 2 weeks (29). In a study by Mohammadali et al., the reliability coefficient of the scale was reported as 0.77 and 0.75 by Cronbach’s alpha and re-test methods, respectively. The construct validity of the scale has been confirmed by exploratory and confirmatory factor analyses (30).
3.4.2. The Multidimensional Scale of Perceived Social Support
This 12-item scale was designed in 1988 by Zimmet, Dahlem, Zimmet, and Farley to assess perceived social support from three sources: family, significant others, and friends on a seven-point scale from 1 (very strongly disagree) to 7 (very strongly agree) (31). The range of scores on this scale is 12 to 84, and in each of the family, significant other, and friend support subscales, 4 to 28. A higher score indicates perceived social support. In examining the psychometric properties of this scale, Cronbach’s alpha coefficient was reported as 0.88 for the scale and 0.86 to 0.90 for the three subscales (32). In Basharat’s study, the reliability coefficient of the scale (0.91) and three subscales of social support of family, significant others, and friends were obtained as 0.87, 0.83, and 0.89 by the Cronbach’s alpha method. The internal consistency coefficients of this scale were confirmed. Additionally, the results of exploratory and confirmatory factor analyses confirmed the validity of the Multidimensional Scale of Perceived Social Support (MSPSS) by determining three factors of social support from family, significant others, and friends (33).
3.4.3. The Distress Tolerance Scale
The Distress Tolerance Scale (DTS) is a self-report index of emotional distress tolerance that was created by Simons and Gaher (2005). This scale includes 15 items and four subscales of emotional distress tolerance (Tolerance), absorption by negative emotions (Absorb), mental assessment of distress (Evaluate), and regulation of efforts to relieve distress (Regulate). Each item is rated on a five-point Likert scale. A score of ‘1’ means “strongly agree”, and a score of ‘5’ means “strongly disagree” with the desired option. The minimum and maximum scores of a subject on this scale are 15 and 75, respectively, indicating greater tolerance. The alpha coefficients for the dimensions of tolerance, absorb, evaluate, and regulate were reported as 0.72, 0.82, 0.78, and 0.70, respectively, and for the whole scale, it was reported as 0.82. In addition, it was observed that this scale has criterion validity and good initial convergence with the coping styles scale (20). Azizi et al. reported Cronbach’s alpha for this questionnaire as 0.67 and the retest validity of this scale as 0.79 (34).
3.5. Statistical Analysis
Data analysis was performed using SPSS software (version 25) and SmartPLS software (version 3.3). SmartPLS enables measurement model evaluation and testing of proposed relationships between constructs. The choice of SmartPLS in this study is based on the following reasons:
(1) The sample size (157 participants), and according to Reinartz et al., “SmartPLS should be the method of choice for all situations where the number of observations is less than 250”.
(2) SmartPLS is the best option if the researcher needs to use the scores of latent variables in subsequent analyses to predict correlation. Structural equation modeling was used to fit the model, and bootstrap was used to test the direct, indirect path, and total effects and their statistical significance, in which 1000 random samples were obtained with a 95% corrected confidence interval (35).
4. Results
Table 1 shows the participants’ demographic characteristics, including gender, parent age, child age, education level, time of diagnosis, and treatment.
| Characteristics | No. (%) |
|---|---|
| Gender | |
| Female | 113 (72) |
| Male | 44 (28) |
| Parent age (y) | |
| 20 - 29 | 37 (23.6) |
| 30 - 39 | 77 (49) |
| 40 - 49 | 31 (19.7) |
| 50 - 59 | 12 (7.6) |
| Education level | |
| Below diploma | 53 (33.8) |
| Diploma | 70 (44.6) |
| B.S. | 31 (19.7) |
| M.A. | 3 (1.9) |
| Child age (y) | |
| 0 - 2 | 30 (19.1) |
| 3 - 6 | 56 (35.7) |
| 7 - 11 | 30 (19.1) |
| 12 - 18 | 27 (17.2) |
| > 19 | 14 (8.9) |
| Time of diagnosis and treatment (having a diet without phenylalanine) | |
| Early (from birth to 15 months) | 95 (60.5) |
| Late | 62 (39.5) |
According to the results of Table 1, most of the studied parents were women (72%) within the age range of 30 - 39 years (49%), with a diploma (44.6%). Most of the studied children were within the age range of 3 - 6 years (35.7%), and most of them (60.5%) received early treatment.
Table 2 shows the zero-order correlations, means, and standard deviations (SDs) for the variables of the current study.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Perceived social support | |||||||||||||||
| 1. Significant others | 1 | 0.53 a | 0.63 a | 0.24 a | 0.19 b | 0.27 a | 0.34 a | 0.26 a | 0.28 a | 0.37 a | 0.26 a | 0.28 a | 0.19 b | -0.11 | 0.23 a |
| 2. Friends | 1 | 0.49 a | 0.21 a | 0.12 | 0.18 b | 0.24 a | 0.25 a | 0.15 | 0.27 a | 0.20 b | 0.17 b | 0.17 b | 0.21 a | 0.15 | |
| 3. Family | 1 | 0.12 | 0.08 | 0.13 | 0.16 b | 0.16 b | 0.10 | 0.18 b | 0.17 b | 0.22 a | 0.05 | -0.11 | 0.12 | ||
| Self-compassion | |||||||||||||||
| 4. Self-kindness | 1 | 0.35 a | 0.47 a | 0.30 a | 0.55 a | 0.30 a | 0.69 a | 0.32 a | 0.35 a | 0.32 a | -0.16 b | 0.32 a | |||
| 5. Self-judgment | 1 | 0.25 a | 0.58 a | 0.30 a | 0.61 a | 0.75 a | 0.39 a | 0.50 a | 0.58 a | 0.02 | 0.57 a | ||||
| 6. Common humanity | 1 | 0.25 a | 0.37 a | 0.22 a | 0.57 a | 0.22 a | 0.31 a | 0.28 a | 0.22 a | 0.26 a | |||||
| 7. Isolation | 1 | 0.30 a | 0.59 a | 0.73 a | 0.37 a | 0.46 a | 0.46 a | -0.06 | 0.47 a | ||||||
| 8. Mindfulness | 1 | 0.38 a | 0.69 a | 0.41 a | 0.48 a | 0.37 a | 0.27 a | 0.40 a | |||||||
| 9. Over-identification | 1 | 0.75 a | 0.46 a | 0.49 a | 0.55 a | -0.03 | 0.56 a | ||||||||
| 10. Total self-compassion | 1 | 0.52 a | 0.62 a | 0.62 a | -0.16 b | 0.62 a | |||||||||
| Distress tolerance | |||||||||||||||
| 11. Tolerance | 1 | 0.64 a | 0.59 a | -0.07 | 0.77 a | ||||||||||
| 12. Absorption | 1 | 0.64 a | -0.11 | 0.81 a | |||||||||||
| 13. Appraisal | 1 | 0.09 | 0.90 a | ||||||||||||
| 14. Regulation | 1 | 0.23 a | |||||||||||||
| 15. Total distress tolerance | 1 | ||||||||||||||
| M | 14.26 | 11.12 | 14.08 | 6.15 | 6.56 | 6.38 | 6.15 | 6.45 | 6.82 | 38.54 | 7.56 | 8.70 | 17.84 | 6.76 | 40.8 |
| SD | 3.83 | 4.37 | 3.94 | 1.72 | 2.05 | 1.55 | 1.98 | 2.05 | 1.88 | 7.95 | 2.67 | 3.21 | 4.95 | 2.36 | 9.71 |
Abbreviations: M, mean; SD, standard deviation.
a P < 0.01
b P < 0.05
According to Table 2, a positive correlation was observed between the three dimensions of perceived social support with self-compassion and its dimensions. Additionally, there was a positive correlation between perceived support from significant others with the overall score of distress tolerance and the dimensions of tolerance, absorption, and appraisal. There was a positive correlation between friend support and tolerance, absorption, and appraisal. There was a positive correlation between family support with tolerance and absorption. There was a positive correlation between the total score of self-compassion and the dimensions of common humanity and mindfulness with distress tolerance and its dimensions. There was a positive correlation between self-kindness with tolerance, absorption, and appraisal and a negative correlation with regulation. There was a positive correlation between self-judgment, isolation, and over-identification with tolerance, absorption, and appraisal.
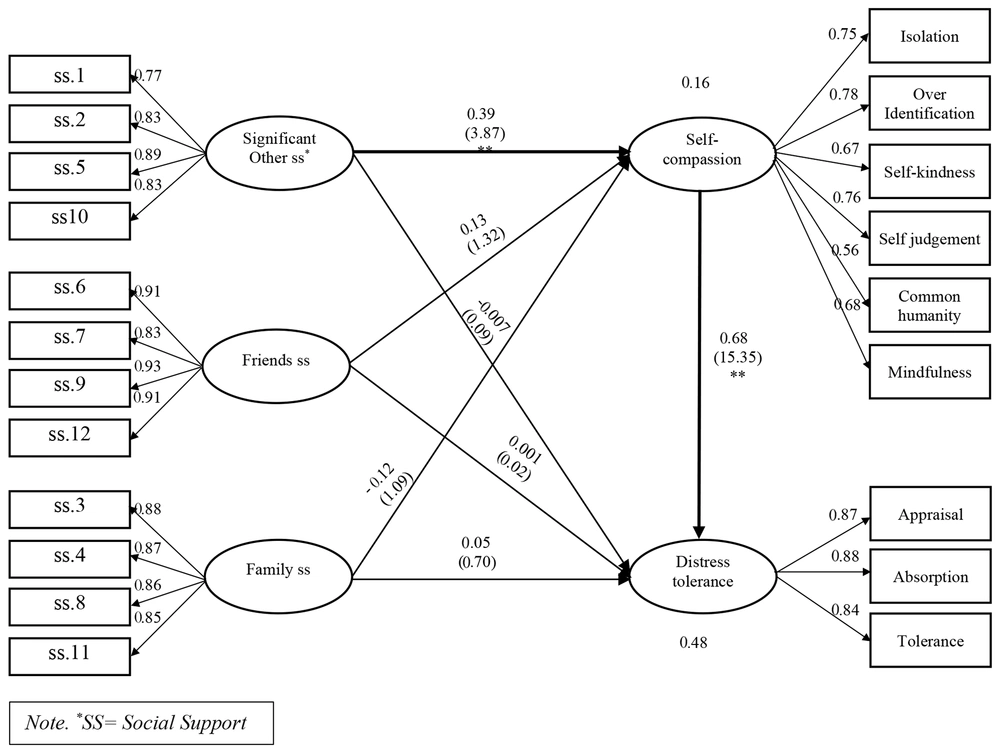
The results of the indices showed the good fit of the model, which favors the role of self-compassion in the relationship between perceived social support and distress tolerance (SRMR = 0.07, NFI = 0.77, GOF = 0.26, Q2 [self-compassion] = 0.08, Q2 [distress tolerance] = 0.33, R2 [self-compassion] = 0.15, R2 [distress tolerance] = 0.49). According to Chin and Marcoulides, the findings suggest that the R2 values obtained in the study can be categorized as follows:
0.19 < R2 < 0.33 is considered weak, and 0.33 < R2 < 0.67 is categorized as moderate (36).
The bootstrapped results of the direct, indirect, and total estimates and the bias-corrected (BC) percentile intervals with 95% confidence are shown in Table 3.
| Path | Β | T | P | BC Interval a |
|---|---|---|---|---|
| Direct effects | ||||
| Significant other SS -> distress tolerance | -0.007 | 0.08 | 0.93 | (-0.15; 0.15) |
| Significant other SS -> self-compassion | 0.39 | 3.87 | 0.0001 | (0.18; 0.56) |
| Friends SS -> distress tolerance | 0.001 | 0.024 | 0.98 | (-0.11; 0.12) |
| Friends SS -> self-compassion | 0.12 | 1.31 | 0.18 | (-0.04; 0.32) |
| Family SS -> distress tolerance | 0.05 | 0.69 | 0.48 | (-0.12; 0.18) |
| Family SS -> self-compassion | -0.11 | 1.09 | 0.27 | (-0.33; 0.10) |
| Self-compassion -> distress tolerance | 0.68 | 15.35 | 0.0001 | (0.58; 0.75) |
| Indirect effects | ||||
| Significant other SS -> self-compassion -> distress tolerance | 0.26 | 3.86 | 0.0001 | (0.13; 0.40) |
| Friends SS -> self-compassion -> distress tolerance | 0.08 | 1.27 | 0.20 | (-0.04; 0.22) |
| Family SS -> self-compassion -> distress tolerance | -0.08 | 1.09 | 0.27 | (-0.22; 0.07) |
| Total effects | ||||
| Self-compassion -> distress tolerance | 0.68 | 15.35 | 0.0001 | (0.58; 0.75) |
| Significant other SS -> distress tolerance | 0.25 | 2.58 | 0.010 | (0.05; 0.45) |
| Friends SS -> distress tolerance | 0.08 | 1.02 | 0.30 | (-0.07; 0.26) |
| Friends SS -> self-compassion | 0.12 | 1.31 | 0.18 | (-0.04; 0.32) |
| Family SS -> distress tolerance | -0.02 | 0.26 | 0.79 | (-0.25; 0.14) |
| Family SS -> self-compassion | -0.11 | 1.09 | 0.27 | (-0.33; 0.10) |
| Significant other SS -> self-compassion | 0.39 | 3.87 | 0.0001 | (0.18; 0.56) |
Abbreviation: SS, social support.
a Reported BC intervals are the bias-corrected 95% confidence interval of the estimates resulting from the bootstrap analysis.
According to the bootstrapped results, the direct effects of perceived support from significant others on distress tolerance (β = 0.39, P = 0.0001) and self-compassion on distress tolerance (β = 0.68, P = 0.0001) were significant and positive (Figure 1).
The indirect effects of perceived support from significant others (β = 0.26, P = 0.0001) via self-compassion on distress tolerance were significant and positive; that is, the relationship between perceived support from significant others toward distress tolerance was mediated through self-compassion.
Perceived support from significant others (β = 0.25, P = 0.010) and self-compassion (β = 0.68, P = 0.0001) had total effects on self-compassion. The total effect of perceived support from significant others on self-compassion (β = 0.39, P = 0.0001) was significant and positive.
5. Discussion
This study tested the direct and indirect effects of perceived social support, self-compassion, and distress tolerance in a sample of parents of PKU children. This study yielded some significant findings.
Firstly, the results of this study indicated that the direct effect of the perceived support of others on self-compassion was significant and positive. The previous studies showed a link between the total score of perceived social support and self-compassion (27, 37-40). In the present study, the effect of perceived social support from (family and friends) on self-compassion was not significant. It seems that parents of PKU children usually feel lonely, sad, and guilty and get stigmatized due to the transfer of a defective gene by their family and friends and consequently do not like to share their problems with those close to them. On the other side, these parents receive dietary products and mental support services from NGOs, which consist of socially active and charitable individuals and health workers, in addition to other parents with PKU children whom they get to know and can address their concerns and issues. In line with this study, Fidika et al. pointed out that social support is a protective factor against perceived stress caused by controlling the child’s therapeutic diet. They indicated that parent support groups are the most useful place to hear the experiences of other families with PKU children, gather more information about the disease and the care needed, and acquire effective strategies for facing the disease at different developmental stages (41).
Secondly, consistent with the results of previous studies (42-44), the direct effect of self-compassion on distress tolerance was significantly positive. Parents of children with PKU are vulnerable because they think that they are responsible for the conditions created for their child or that they are not able to properly care for their child. Parents of PKU children might feel guilty and blame themselves for passing on a defective gene to their child (45). Self-compassion is an effective coping strategy that facilitates a kind of adaptive communication with oneself and awareness, along with acceptance of negative thoughts and feelings, kindness toward oneself when suffering, and the capacity to look at life’s challenges as part of common humanity (18). On the other hand, the lack of this self-compassion might react to their difficult experiences by avoiding the experience of suffering, over-identification, blaming, and self-judgment (13).
Being a member of PKU support groups and being supported by other individuals, in addition to sharing experiences with other parents of children with PKU, makes these individuals feel more effective, less limited, and isolated in their role as parents. Self-compassion allows a person to see more clearly and acknowledge difficulties without taking them more personally (18). By addressing the challenges of raising a PKU child and remembering that suffering is a universal and common human experience, parents of children with PKU will feel less cut off from others. Therefore, self-compassion is a powerful buffer against the personal distress that can arise when caring for a child with PKU.
Thirdly, consistent with the results of previous studies (27, 40, 46, 47), the relationship between perceived support from significant others and distress tolerance was mediated through self-compassion. The person’s perceptions can strengthen his/her coping resources in facing stressful events. The awareness of the existence of support resources makes the parents confident that they will get the help of others to face difficult situations and suffering caused by the child’s illness. In other words, in the beginning, the event is perceived as negative and stressful; however, the support resources available to face the stress factor help the person to endure that stressful event. A person’s perception of access to supportive resources is effective in weakening the negative effect of a stressful event, and finally, the parents can evaluate the event as controllable (48).
Furthermore, strengthening awareness and acceptance, along with kindness, in parents makes them give themselves more opportunities to compensate and rebuild communication-based on trust and compassion toward themselves in interpersonal relationships that are criticized or blamed by others. Self-compassion can increase distress tolerance in individuals by providing positive experiences, increasing adaptation to stressful situations, and expressing empathy. Instead of avoiding painful feelings, self-compassionate individuals recognize and face them and show compassion and tolerance toward those feelings. Additionally, being a member and being in a suitable atmosphere of support groups and other parents with a child with PKU, providing and receiving positive feedback, benefiting from the support of others, and creating opportunities to express oneself appropriately and express views, opinions, confusion pain, and anxiety, sharing experiences and offering help to others to think together to reach the best solution can provide the basis for reducing the feeling of guilt and increasing the tolerance of distress.
5.1. Limitations, Implications, and Future Research
The current study’s sample consisted of Iranian parents with PKU children. Therefore, the findings might not be generalizable to other communities and other clinical samples. The same model can be tested in other communities, such as parents with other disabilities in children. Furthermore, the sample size was relatively small because PKU is a rare metabolic disease. The use of self-report tools and limited information from other sources can limit the validity of the findings; therefore, the use of measurement tools and more extensive information sources should be considered in future studies. The unequal number of fathers and mothers participating in this study has limited the possibility of further comparison and more accurate assessment of gender differences; therefore, further studies are needed in this regard. Another limitation was the cross-sectional nature of the study. Longitudinal studies can be conducted to evaluate the psychological status of the same parents at different ages of their children.
Future research should examine the above-mentioned associations in a much larger sample and other clinical populations to learn more about the interconnections between these variables. Qualitative studies can also explore these connections in more personally meaningful ways for the parents to increase our understanding of their experiences and help those suffering.
5.2. Conclusions
The findings of this study help clinicians pay closer attention to their client’s perceived social support from different sources (i.e., significant others, families, and friends), whether they experience self-compassion or not, and the level of their distress tolerance. Furthermore, the findings suggest that mental health professionals need to consider preventive education that can potentially decrease the prevalence of stigma from close friends and family of PKU children of transference of defective genes. The findings indicate the important role of self-compassion in the ability to tolerate distress. Therefore, parenting education focusing on self-compassion can be very important. Improving the ability to be kind to oneself can lead to less self-judgment and a feeling that they are not alone in their suffering and that they feel part of the community of human beings.