1. Background
Mood disorders, including major depressive disorder and type I and II bipolar disorder, are among the most important health problems in society and important causes of disability in the world (1). More than 21% of children live in families where at least one parent has a psychiatric illness (2). Around 30% of these children experience behavioral problems, and 37% of them deal with excessive worries. Mood disorders, failure in school, social isolation, and anxiety can be other problems threatening these children (3, 4). These children may even have to bear the additional burden of caring for their parents and siblings and face family crises, causing them to experience feelings such as embarrassment, shame, guilt, or anger due to stigma (5). The hospitalization of parents may be one of the most anxiety-provoking issues for these children. Periodic hospitalizations, acute periods of illness, unpredictability, and the chronicity of the disease are some other challenges for these children. Thus, maintaining stability in such families requires more effort and struggles (6, 7). These families may fall into financial problems, leading to children’s lack of access to proper education or employment, increasing the risk of domestic violence and deprivation of personal and social support (2).
Nearly 40% of these children state that no one talks to them about their parent’s illness (4), and the fact that the lack of information about the disease confuses them. These children are afraid that they may be at risk of developing the disease in the future and express worries that their parents may never recover. Some children also believe that they are the cause of their parents' illnesses (8, 9).
Talking about parents’ illnesses relieves children’s fears, reduces their confusion, and increases their resilience (10, 11). When a parent with a mental illness is admitted to a mental health center, a brief history should be taken about their children, and supportive interventions should be considered if needed. The most common intervention is psychosocial training for these children and adolescents (12). Different programs aim to create opportunities for adolescents to interact with their peers, increase their adaptability and self-esteem, help them correctly understand mental illnesses, and create a space for adolescents in which they can cease caring for their parents. Therefore, interventions are primarily and mostly supportive and preventive (13).
Peer-group support programs are believed to increase children’s knowledge about mental illnesses, strengthen their relationships with peers from similar families, and nurture their adaptive skills (12). Peer-group support programs provide a safe place for adolescents to express their feelings, share their experiences, learn the coping strategies employed by others, and develop problem-solving skills. This type of support can be beneficial in helping children gain confidence and build self-esteem and resilience (12, 14).
Resilience is the capacity of an individual to overcome the negative effects of a challenging situation. Resilience consists of many factors enhancing one’s power to adapt and thrive despite adversity (15). Studies suggest that psychoeducation can increase resilience in these children (16). Self-esteem is a person’s overall evaluation of his/her worth and value (17). Developing high self-esteem is essential for having mental well-being as it may serve as a buffer against parents’ mental illnesses. Low self-esteem can be a risk factor, and high self-esteem can protect adolescents (16). Many studies have shown that providing timely and age-appropriate information and support by mental health professionals can help adolescents to shape good coping strategies and support mechanisms (18).
2. Objectives
To the best of our knowledge, no studies have yet been conducted in Iran to investigate the effectiveness of peer-group support on the resilience and self-esteem of adolescents whose parents suffer from mood disorders. On the other hand, some former studies have recruited a small sample size without any control group. Therefore, this research was conducted to address this issue.
3. Methods
This was a randomized clinical trial (registration number: IRCT20210804052078N1) conducted in Kashan in 2022. Adolescents were selected from 12-18-year-old children whose parents were suffering from a major depressive disorder or bipolar disorder undergoing outpatient treatment or receiving inpatient services at the Kargarnjad Hospital of Kashan. Inclusion criteria were the diagnosis of mood disorders in parents according to the DSM-5 scale, parents’ consent for their children to participate in the study, adolescents’ being aware of their parents' illnesses, and children’s willingness to participate. Exclusion criteria were the diagnosis of psychiatric illnesses in adolescents and missing more than two sessions of the peer-group support program. Clinical interviews were conducted based on SCID-5 CV with both parents and then their children by psychiatrists working in Kargarnejad Hospital to confirm the inclusion and exclusion criteria.
No parallel RCTs were found, so the sample size was calculated according to the parameters reported in a pre-post study by Foster et al. (19) as α = 0.05 and β = 0.2. Using the formula specific for the before-after study design, the required sample size was obtained as 40. Regarding probable attrition, the final sample size was increased to 50 in each group.
After evaluating candidates for inclusion and exclusion criteria and observing ethical issues, each participant was assigned a unique code using SPSS software, 50 adolescents were allocated to the intervention group, and 50 others were assigned to the control group using the simple randomization method. In each group, 20 adolescents did not answer the study questionnaires, and the data from the remaining 60 adolescents were analyzed.
After explaining the program and its relevance to parents, the informed consent form was signed by parents, and then a demographic information form was completed by the adolescents and parents.
Before starting the project, adolescents in both groups completed two questionnaires: (1) Conner and Davidson’s resilience and (2) Rosenberg’s self-esteem. The participants in the intervention group were divided into groups of 6 to 8 of the same sex, and each group participated in 90-minute sessions held by a psychiatric assistant every week for eight consecutive weeks. Both groups answered the two questionnaires again at the end of the eight weeks.
Rosenberg’s self-esteem scale measures overall self-esteem, satisfaction with life, and a sense of worth. This questionnaire consists of ten items, and the subject is asked to respond on a four-point Likert scale ranging from "strongly agree" to "strongly disagree." The score on this scale ranges from 10 to 40, with higher scores indicating higher self-esteem. In Iran, Rajabi and Nasreen verified the reliability of this tool with Cronbach’s alpha coefficient of 0.84 (20).
Connor and Davidson's Resilience Scale contains 25 statements rated on a Likert scale from 0 (totally false) to 5 (always true). The test score ranges from 0 to 100. A higher score indicates greater resilience. The scale consists of five subscales, including “personal competency, high standards, and tenacity”, “trust in one’s instincts, tolerance against negative emotions, and strengthening effects of stress”, “positive acceptance of change and secure relationships”, “control”, and “spiritual influences”. In Iran the reliability of this scale with Cronbach’s alpha coefficient of 0.95 was approved (21).
3.1. Peer-group Support Program
The intervention sessions were facilitated by a trained psychiatric assistant according to the Kids in Control Program and using the concepts from the books "Supportive Psychotherapy Learning Guide" (22), "Depression: A Family Guide" (23), and "Bipolar Disorder: A Family Guide" (24), as well as the pamphlets available from the COPMI website. The psychiatry assistant also received supervision from a child and adolescent psychiatrist and a fellowship of psychotherapy specialist. The following topics were discussed during eight sessions in order:
(1) Introduction and establishing the feeling of belonging to a group, explaining group rules, confidentiality guidelines, creating a group identity, acquaintance with each other, and identifying the ability to make decisions.
(2) Obtaining an understanding of basic emotions, comprehending the terminology of primary emotions, and learning how to control emotions.
(3) The roles and responsibilities that adolescents should or shouldn’t take, appropriate ways to share feelings, and proper defenses.
(4) Understanding psychiatric diseases, their causes and physiological basis, and expressing the problems caused by the mental illness of parents.
(5) Understanding treatments and drugs, knowing false information about psychiatric illnesses, expressing how stigma affects one’s life, and managing feelings of shame or guilt towards parents.
(6) Understanding the meaning of resilience, discovering personal experiences of resilience, and promoting tools that strengthen it.
(7) Acquiring information about the meaning of self-esteem, discovering personal experiences of self-esteem, and recognizing individuals’ strengths and valuable abilities.
(8) The importance of self-care, ways to obtain approval, valuing oneself, and recognizing one’s and others’ special qualities.
Because each group’s experiences and needs were different and special, the groups did not follow the exact outline, and the content was modified according to the conditions of the meeting and the group. At the end of the program, satisfaction with group participation and perceptions of mood disorders were surveyed in interviews.
Data were presented using descriptive statistical measures (mean, standard deviation, and frequency) and analyzed using the independent samples Mann-Whitney U test, Fisher’s exact test, paired t-test, independent t-test, and Pearson chi-square test. Data were analyzed using SPSS 26. The statistical significance level was determined as P < 0.05 at a 95% confidence interval.
4. Results
In the intervention group, 11 adolescents (36.6%) did not participate in any session due to reasons such as the coincidence of the sixth peak of COVID-19 in Iran, hospitalization of parents, caring for siblings, school programs and exams, and other commitments. Four of the participants were excluded due to their absence from more than two sessions. Five adolescents in the control group did not complete the questionnaires at the end of the eighth week. At the end of the study, the data of 15 adolescents in the intervention group and 25 adolescents in the control group were obtained. According to Tables 1 and 2, the sociodemographic characteristics of participants in the intervention and control groups were homogeneous, with no statistically significant differences except for the gender and occupation of parents.
| Characteristics | Intervention Group, Mean ± SD | Control Group, Mean ± SD | P-Value a |
|---|---|---|---|
| Adolescents’ age | 14.93 ± 1.6 | 15.20 ± 2.0 | 0.676 |
| Parents’ age | 44.60 ± 6.3 | 44.6 ± 4.9 | 0.982 |
| Number of children | 2.2 ± 0.5 | 2 ± 0.52 | 0.154 |
a Independent t-test, P < 0.05
| Characteristics | Intervention Group | Control Group | P-Value |
|---|---|---|---|
| Parents’ gender | 0.018 b | ||
| Male | 10 (66.6) | 6 (24.0) | |
| Female | 5 (33.3) | 19 (76.0) | |
| Illness of both parents | 0.586 b | ||
| No | 13 (86.6) | 23 (92.0) | |
| Yes | 2 (13.3) | 2 (8.0) | |
| Parents’ education | 0.138 c | ||
| High school | 10 (66.6) | 9 (36) | |
| Diploma | 4 (26.6) | 9 (36) | |
| Higher than diploma | 1 (6) | 7 (28) | |
| Parents’ occupation | 0.464 b | ||
| Housewife/Employed | 13 (86.6) | 24 (96) | |
| Unemployed | 1 (6.6) | 1 (4) | |
| Disabled | 1 (6.6) | 0 (0.0) | |
| Parents’ marital status | 1.00 b | ||
| Married | 14 (47.8) | 24 (52.1) | |
| Divorced | 1 (71.4) | 1 (28.6) | |
| Adolescents’ gender | 0.57 c | ||
| Male | 7 (46.6) | 14 (56) | |
| Female | 8 (53.4) | 11 (44) | |
| Adolescents’ education | 0.120 b | ||
| First to 5th grade | 1 (6.6) | 3 (12) | |
| 6th to 9th grade | 10 (66.6) | 8 (32) | |
| 10th to 12th grade | 4 (26.6) | 14 (56) | |
| Adolescents’ occupation | 0.375 b | ||
| Student | 14 (93.3) | 25 (100) | |
| Dropout | 1 (6.7) | 0 (0.0) | |
| Age of children at the time of the onset of parents’ illness, y | 0.073 b | ||
| < 5 | 14 (93.3) | 15 (60) | |
| 5 - 10 | 1 (6.7) | 7 (28) | |
| > 5 | 0 | 3 (12) |
a Values are expressed as No. (%).
b Fisher’s exact test.
c Pearson chi-square test.
Despite the dropout of half of the participants in the intervention group, the analysis continued on the existing data due to the presence of acceptable available data. At first, the distribution of scores was checked for normality and the presence of outliers, and since the data had non-normal distribution, they were transformed; however, the skewness of the data did not resolve, so the non-parametric Mann-Whitney test was used. The results showed a significant difference between the two groups in terms of the resilience score and its subscales.
In the beginning, the mean of the total resilience score was significantly different between the intervention and control groups (P = 0.005). The scores obtained for resilience subscales are shown in Table 3.
| Intervention Group, Mean ± SD | Control Group, Mean ± SD | P-Value a | |
|---|---|---|---|
| Self-esteem | 26.1 ± 2.8 | 28.4 ± 3.9 | 0.057 |
| Personal competency | 14.3 ± 10.0 | 20.3 ± 7.6 | 0.041 |
| Trust in one’s instincts | 10.2 ± 6.4 | 17.1 ± 4.6 | 0.000 |
| Positive acceptance of change | 10.0 ± 4.7 | 14.0 ± 3.2 | 0.004 |
| Control | 5.9 ± 3.8 | 7.6 ± 3.0 | 0.128 |
| Spiritual influences | 4.6 ± 2.7 | 6.1 ± 1.9 | 0.049 |
| Total resilience | 44.5 ± 26.0 | 65.5 ± 16.8 | 0.005 |
a Independent samples Mann-Whitney U test, P < 0.05
Due to differences between the groups in terms of some demographic variables and self-esteem and resilience scores in some sub-scales at the baseline, and also insufficient and non-normally distributed data, it was not possible to use statistical models. Therefore, the paired t-test was used due to its robustness against the violation of the assumption of non-normality of the data and the easier understanding of the findings by paired comparison (Table 4).
| Groups | Average Score (Week 0) | Average Score (Week 8) | 95% Confidence Interval of the Difference | P-Value a |
|---|---|---|---|---|
| Self-esteem | ||||
| Intervention | 26.1 (2.8) | 27.3 (4.7) | -4.0 (-7.4 - 0.7) | 0.212 |
| Control | 29.2 (3.7) | 29.5 (3.9) | -0.3 (-1.2 - 0.5) | 0.473 |
| Personal competency | ||||
| Intervention | 13.9 (9.4) | 14.9 (7.2) | 0.3 (-1.2 - 1.8) | 0.523 |
| Control | 20.3 (7.7) | 20.2 (7.1) | 0.1 (-2.2 - 2.5) | 0.894 |
| Trust in one’s instincts | ||||
| Intervention | 9.8 (6.8) | 13.9 (4.6) | -5.3 (-13.0 - 2.4) | 0.021 |
| Control | 17.2 (4.8) | 16.5 (4.8) | 0.6 (-1.0 - 2.3) | 0.441 |
| Positive acceptance of change | ||||
| Intervention | 9.9 (5.1) | 11.0 (3.4) | -0.6 (-1.9 - 0.7) | 0.345 |
| Control | 13.6 (3.7) | 12.6 (4.7) | 1.0 (-1.5 - 3.5) | 0.403 |
| Control | ||||
| Intervention | 5.4 (3.7) | 5.1 (3.3) | -1.0 (-4.6 - 2.5) | 0.669 |
| Control | 7.6 (3.0) | 7.3 (2.3) | 0.3 (-0.8 - 1.5) | 0.573 |
| Spiritual influences | ||||
| Intervention | 4.6 (2.9) | 5.2 (2.9) | -1.0 (-3.4 - 1.3) | 0.120 |
| Control | 6.1 (1.9) | 5.6 (2.1) | 0.5 (-0.2 - 1.3) | 0.197 |
| Total resilience | ||||
| Intervention | 47.1 (25.9) | 52.4 (21.2) | -0.6 (-1.4 - 0.1) | 0.150 |
| Control | 66.1 (20.9) | 62.8 (18.0) | 3.3 (-7.4 - 14.1) | 0.510 |
a Paired Samples t Test, P < 0.05.
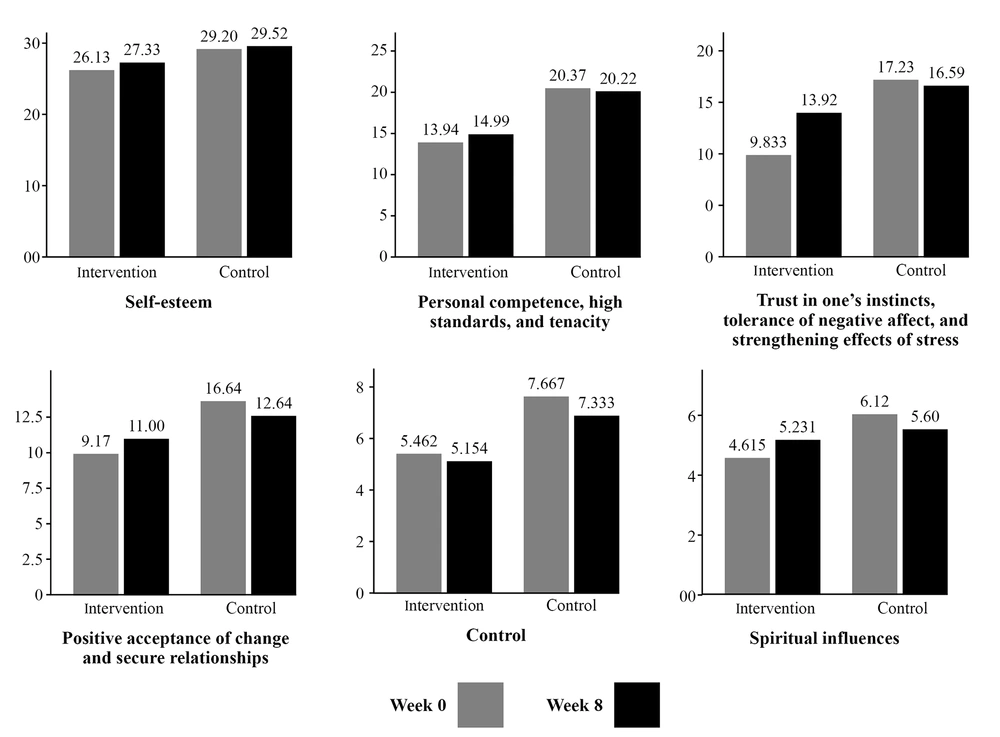
Except for the subscale of trust in one’s instincts, there was no significant difference in the post-intervention scores of other variables and subscales between the two groups at the end of the intervention. However, when looking at the means, most of the adolescents in the intervention group showed an elevation in scores, indicating an improvement in their conditions. According to Figure 1, the average self-esteem score increased in the intervention group after eight weeks. The average scores of the subscales of personal competency, trust in one’s instincts, positive acceptance of change, and spiritual influences, as well as total resilience, increased in the peer-group support group after eight weeks. Peer-group support appeared to have the most strong effect on the subscale of trust in one’s instincts, showing a significant boost.
At the final interview, the participants were asked to state what they gained in the sessions, and they mostly mentioned acquiring knowledge about psychiatric illnesses. The participants also noted that after realizing that there were others with similar problems and finding that they were not alone, they felt that they could talk with their peers dealing with similar situations about their problems, making them feel better at the end of the sessions.
5. Discussion
This randomized controlled study measured resilience and self-esteem in adolescents aged 12 - 18 years who had one or both of their parents suffering from a mood disorder. The pre-intervention self-esteem and resilience scores were significantly lower in the intervention group. We assume that the adolescents who attended all the peer-group support sessions were the ones with lower self-esteem and resilience who sought help the most, so they didn’t drop out, and their scores were attained in the final analysis. After eight weeks of the intervention, the average scores of self-esteem and total resilience (along with its subscales) increased in the intervention group; however, the difference with the control group was only statistically significant in one of the subscales of resilience: trust in one’s instincts. This aspect of resilience appeared to raise the most following peer-group support. One of the reasons for the significant increase in the score of the trust in one’s instincts subscale may be due to the fact that the support sessions brought greater attention to concepts like problem-solving, decision-making, basic emotions, and adaptive skills in response to one’s demands, which are all related to trust in instincts.
The participants reported that they felt relieved after having the opportunity to talk about their problems and share the feelings they could not share with anyone or were embarrassed to express. This means that the peer-group support program achieved one of the most important of its goals and therapeutic effects: cohesion (14, 25). Another goal of group therapy was universalization (25), which seemed to be achieved during these sessions as the participants reported in their interviews that they realized that they were not alone and that there were other adolescents dealing with similar situations.
Similar to the findings of other studies (16), according to our participants’ opinions expressed in the final interviews on the topics discussed in the peer-group sessions, such as mood disorders and their symptoms, treatment options, and the behavioral consequences of the illness, it was concluded that mental health literacy could improve adaptation to life’s events, life satisfaction, and the perception of social support.
Fraser and Pakenham also reported that peer-counseling group sessions had no significant effect on resilience, but most participants in the intervention group reported improvement in their mental health literacy, depression, and life satisfaction (26). In Tapias et al.’s study, significant differences were observed in a number of the subscales of strengths and difficulties, but no significant effect was observed on resilience and self-esteem. Other outcomes included an increase in emotional support of children by parents, improvement in children’s social behaviors, and a reduction in stigma (27).
Pitman and Matthey’s research showed that life satisfaction, self-esteem, and coping skills improved in their participants after peer-group support sessions (28). In Richter’s research, an educational-supportive intervention focusing on resilience was shown to boost self-esteem and awareness of mental illnesses and decrease maladaptive mechanisms (16). In another study by Kucuk, the resilience score significantly increased in the intervention group compared to the control group (29). This discrepancy between our observation and that of these studies may be due to the larger number of participants and fewer dropouts in recent studies. In van Santvoort et al.’s study, children in the intervention group experienced reduced negative cognition, increased social support, and persistent social acceptance (i.e., adequacy) (30). In all these studies, the interventional program was focused on specific indicators of mental health. This is because adolescents may have different needs and, therefore, different group sessions, making it inapplicable to implement the same program and setting in different studies. For this reason, a large sample size is needed to obtain more generalizable findings. Similar to our study, the results of different studies indicate that peer-group support can improve different indicators of mental health.
The strengths of this study include the fact that we designed a program specific to adolescents in need. In addition, this integrative study was conducted by mental health professionals and was one of the first studies in this field in Iran. Addressing our limitations, this study was conducted at a single center and had a small sample size due to a large number of dropouts, which reduced generalizability. In addition, we had short-term group counseling and used only two questionnaires to assess outcomes.
5.1. Conclusions
The current study showed that eight weeks of peer-group support improved self-esteem and resilience in adolescents whose parents suffered from mood disorders. However, the increase in the resilience score was not significant except for the ‘trust in one’s instincts’ subscale. Moreover, adolescents’ awareness about mental disorders was expanded, and the peer-group support sessions could achieve cohesion and universalization as two of the most important goals of group therapy. To further explore the effects of peer-group support, we suggest that future studies employ larger sample sizes and use more tools to determine more outcomes such as life satisfaction, family functioning, adaptive mechanisms, mental illness awareness, and social support.