1. Background
Autism spectrum disorder (ASD) is a neurodevelopmental disorder diagnosed based on DSM-5, characterized by continuous communication and social interaction deficits and repetitive patterns of interests, behavior, and activities (1). The Centers for Disease Control and Prevention (CDC) estimates that 1 in 54 children has been identified with ASD (2). In Iranian children and adolescents, the prevalence of ASD is estimated at 0.1% (10 in 10,000 people) (3). Sensory processing problems are highly prevalent in children with ASD, ranging from 69% to 95% (4-7), and are considered one of the diagnostic criteria for ASD based on DSM-5 (1). Sensory processing patterns in children with ASD differ from those of typically developing children (8, 9), affecting various aspects of their daily lives, including self-care, education, and play (9-11).
Sensory integration therapy (SIT) is the most common method used by occupational therapists for children with ASD (12-15). Despite its widespread popularity, there is limited evidence for the effectiveness of this approach (12, 15). Previous studies have reported inconclusive results regarding the effectiveness of SIT (15-17). Only a few studies have evaluated the direct effects of SIT on sensory processing using standardized assessment tools in children with ASD, most of which support the positive effects of SIT on outcomes such as adaptive behaviors (12). Kashefimehr et al. demonstrated that SIT interventions based on Ayres’ principles could improve the sensory processing abilities and occupational performance of 3-8-year-old children with ASD (18). Randell et al. indicated that although SIT interventions could somehow reduce problematic behaviors of children with ASD, as well as parental stress, no statistically significant difference was observed in sensory processing (19).
Children with autism playing is characterized by its stereotypical or repetitive nature (1). Given the importance of play as the primary occupation of children, occupational therapists often employ play-based assessment and treatment approaches (20, 21). Additionally, the child’s family plays a pivotal role in shaping the child’s growth environment and behavior and can actively participate in play-based interventions (22). Parental engagement in the treatment process is crucial for children with special needs, particularly those with ASD, as they face various challenges that significantly impact the physical, mental, economic, and social performance of family members (8). Many families with ASD children request occupational therapists to assess the sensory factors that affect their children’s participation in daily activities (23). However, there are limited studies investigating the effectiveness of family-oriented interventions in improving sensory processing in children with ASD (10). In a clinical trial conducted by Pashazadeh Azari et al., families of children with ASD were trained using coaching principles to align their daily activities with the sensory needs of their children. The findings revealed that sensory issues were mitigated, and both the child’s participation and parenting efficacy improved (24). Building upon these findings, the current study aimed to evaluate the effectiveness of a sensory integration intervention on the sensory patterns of children with ASD. Additionally, the study sought to investigate whether or not implementing sensory play interventions with parent engagement could enhance the effectiveness of the sensory integration intervention. Due to the engagement of parents in sensory interventions through play activities at home, the combined approach was expected to provide a more comprehensive and holistic intervention to address sensory processing difficulties in children with ASD.
2. Objectives
This study aimed to evaluate the effectiveness of a sensory play activity-based intervention with the participation of parents along with SIT in resolving sensory processing difficulties in children with ASD. Our results were expected to provide insights for augmenting the therapeutic efficacy of these approaches and expanding available therapeutic options for families.
3. Methods
3.1. Design
This study utilized a double-blinded, randomized clinical trial design. The study’s protocol was approved by the Ethics Committee of Tehran University of Medical Sciences (IR.TUMS.FNM.REC.1400.160) and registered at the Iranian Registry for Clinical Trials (IRCT20211114053055N1).
3.2. Participants
The study was conducted on children with mild or moderate ASD with age between 3 and 6 years old. Inclusion criteria for the study were the presence of sensory processing disorder in at least one pattern according to the sensory profile 2 (SP2), no history of seizure or epilepsy, absence of physical problems, and having at least a high school diploma (for parents). The exclusion criterion was the lack of cooperation of children with ASD or their parents at any stage of the study.
3.3. Sample Size
The sample size was calculated as n = 48 based on a similar study (24) and according to Equation 1. Considering a potential dropout rate, 56 samples were finally included in the study.
The elements within the formula and their roles in the process were as follows:
(1) Critical values (Z-scores):
(2) Variance (
(3) Means (
The values used in this study were as follows:
Plugging these values into the formula, a sample size of approximately 48 was achieved. This sample size was thought to be adequate to deliver 80% power to detect the intended effect size if it existed.
Therefore, the above formula was employed to calculate an appropriate sample size using appropriate critical values, variances, and means depending on factors such as the research context, significance level, desired power, and anticipated effect size.
3.4. Study Setting
This study was conducted in Tehran, Iran, at two different centers: (1) the Occupational Therapy unit of the Arman Shayan Comprehensive Rehabilitation Center and (2) the Rangin Kaman Autism Center. These two centers provide separate and suitable rooms for service delivery to children with autism. The Arman Shayan Comprehensive Rehabilitation Center, and its Occupational Therapy Unit in particular, served as one of the primary locations for data collection and intervention implementation. This center is dedicated to providing occupational therapy services to individuals with sensory processing disorders, including children with ASD. The physical space and equipment in rooms were designed to support therapeutic interventions tailored to the needs of children with autism. The Rangin Kaman Autism Center, the second study setting, is a specialized center for providing comprehensive services to children with autism. This center also has suitable rooms designed to accommodate the unique requirements of patients with autism. These rooms were equipped with appropriate sensory materials and tools to facilitate implementing the intervention and support the sensory development of children. Both these places provided controlled and structured environments for data collection and intervention implementation, ensuring that the interventions were conducted in an appropriate and supportive atmosphere, contributing to the effectiveness of implementation and the accuracy of the data collected.
3.5. Procedure
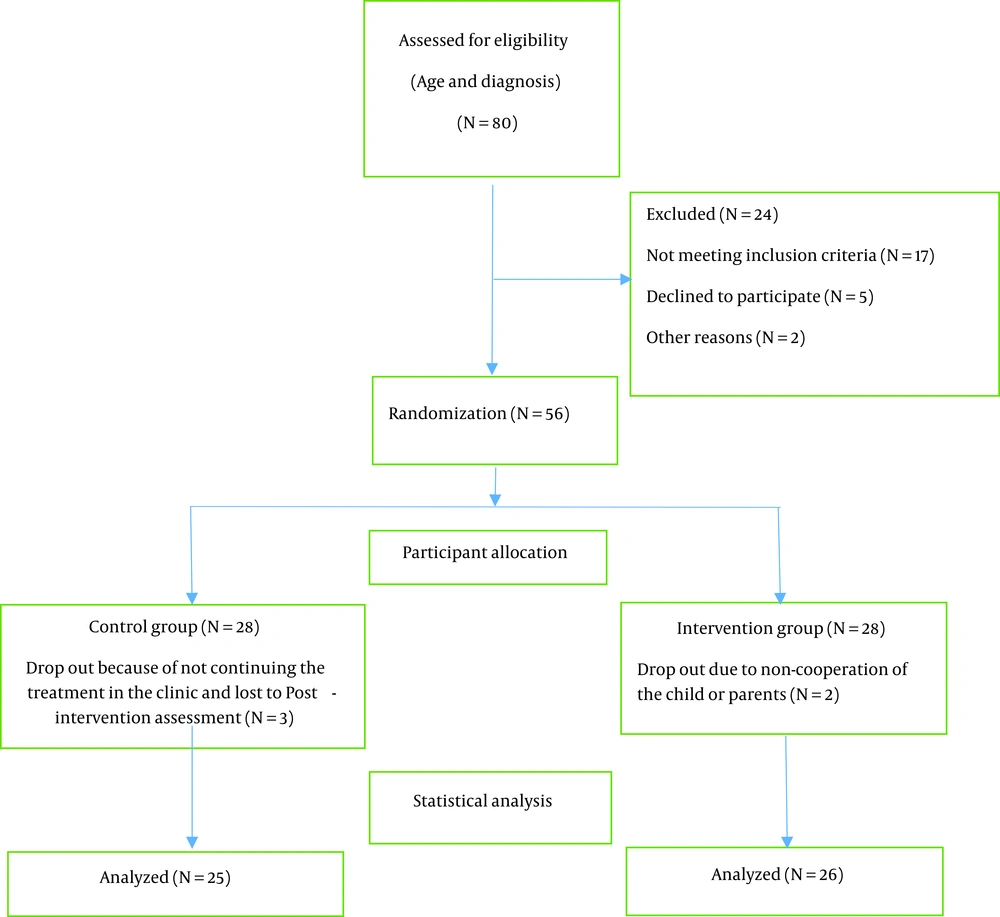
A total of 80 children with ASD aged 3-6 years were selected using convenience sampling and assessed for eligibility based on inclusion criteria, including the completion of the Gilliam Autism Rating Scale-Second Edition (GARS-2) and SP2 by parents. Parents whose ASD children presented at least one sensory processing disorder (SPD) pattern according to SP2 were requested to share information about the research subject, complete a demographic form, and sign the consent form. Participants were then randomly assigned to either the intervention (n = 28) or control (n = 28) group, matched based on gender and the number of disturbed SPD patterns.
3.6. Participant Enrollment
Participants were enrolled by the primary investigator and other research team members who screened potential participants, assessed their eligibility criteria, and obtained informed consent from those who met the inclusion criteria (Figure 1).
3.7. Randomization
The randomization process was carefully conducted to ensure unbiased group assignment. Participants were randomly assigned to either the intervention or control group using a random allocation sequence generated by the “Randomization.com" website. The randomization was performed by an independent researcher who was not involved in the data collection process.
3.8. Blinding
To maintain blinding and conceal the random allocation sequence, containers were prepared in advance by the independent researcher. The containers were opaque and identical in appearance to ensure that group assignments remained concealed until the final intervention assignment. The containers were opened sequentially according to the order of participant enrollment during the intervention assignment process. The random allocation sequence was securely stored and was accessible only to the designated research team members responsible for preparing the containers. Researchers involved in participant recruitment, assessments, and intervention delivery were kept blinded to the random allocation sequence until intervention assignment. This strategy for blinding was employed to minimize potential bias and ensure the integrity of the randomization process.
In this study, the participants were blinded to their group assignment. Also, the data collection process was conducted by trained assessors who were blinded to the participants’ group allocations to ensure objectivity and impartiality during data collection and outcome assessment.
3.9. Participant Assignment to Interventions
An independent researcher who generated the random allocation sequence was in charge of assigning participants to interventions based on the randomized sequence obtained from the “Randomization.com" website. The allocation was performed by matching each participant’s identification number with the corresponding group assignment.
Both groups received common sensory interventions based on SIT principles and the unique sensory needs of each child in two 45-minute sessions per week for 8 weeks. In addition to SIT sessions, the intervention group also received the sensory play intervention once a week (one 30-minute session) for 8 weeks, followed by performing play activities at home three times a week with the participation of parents. Prior to the intervention, a motivational session was held for the parents whose children were in the intervention group to emphasize the importance of the research and provide guidance on how to perform play activities at home. The therapist made 30-minute phone calls or video calls once a week to follow up on the accurate conduction of home play activity sessions and respond to parents’ questions, if any. Sensory processing was evaluated using SP2 before and after the intervention to determine the effect of the interventions.
3.10. Participant Timeline
The recruitment period of the study spanned 3 weeks, during which the files of 80 clients who met the inclusion criteria were reviewed. Informed consent was obtained during this time. Evaluations using GARS and SP2 scales were conducted over a period of 20 days. After completing these tools, a total of 56 eligible individuals were included in the study. After initial evaluations, the members of both the intervention and control groups participated in the interventional phase, which lasted 8 weeks. The members of the experimental group received both a sensory play activity intervention and sensory integration, while those in the control group received sensory integration only. Close follow-ups were conducted during the 8-week period to ensure the proper implementation of the interventions. Within 3 weeks after the completion of the interventions, a post-test was conducted for all participants. Overall, the entire study process, including recruitment, primary evaluation, intervention, and secondary evaluation, lasted 5 months (Table 1).
| Intervention Group | Control Group |
|---|---|
| Pre-assessment | Pre-assessment |
| Common Sensory Integration | |
| 8 weeks, 16 sessions, 45 minutes, at least 2 sessions per week | 8 weeks, 16 sessions, 45minutes, at least 2 sessions per week |
| Sensory Play Intervention | |
| 8 weeks interventions | |
| 8 in-person sessions, 1 session per week: Teaching parents how to perform sensory play activities at home and addressing possible problems and questions | |
| 3 times a week, home sessions, each session for 30 minutes: Performing sensory play activities at home by parents 3 times a week | |
| 8 sessions, 1 session per week: 30-minute phone calls or video calls made by the therapist to follow up on home sessions and answer parents' questions | |
| Post-assessment | Post-assessment |
Study Timeline in Each Study Group
3.11. Common Sensory Integration
The sensory integration intervention was performed in compliance with most principles of Ayres Sensory Integration Therapy (ASIT), including ensuring safety, presenting a range of sensory activity opportunities, arranging the environment to help the child maintain self-regulation and alertness, collaborating with the child on activity choices, tailoring activities to present the “just-right challenge" ensuring that activities are successful, supporting the child’s intrinsic motivations to play, and establishing a therapeutic alliance with the child (12).
3.12. Sensory Play Intervention
Sensory play activities were selected from the Persian version of Early Intervention Games presented by Barbara Sher (25, 26). The games were classified based on the adaptation and matching of activities to a specific sensory modality by the research team. A manual entitled “Sensory Plays", including explanations and written guides for each activity was prepared using the mentioned book and presented to parents. The selection and scope of the games were based on the SP2 score and the degree of their sensory challenges. During in-person sessions, the therapist, in the presence of the child, taught the parents how to perform the play activities at home. Environmental adaptations and strategies were provided to be applied at home based on Dunn’s sensory processing model (27). The performance of parents at home was followed and assessed using a checklist prepared by the research team. According to parents’ reporting, if the child’s participation in the already instructed game at home was 70%, the next novel play activity was provided.
3.13. Data Collection Tools
3.13.1. The Gilliam Autism Rating Scale-2
The Gilliam Autism Rating Scale-2 is a behavioral questionnaire developed for individuals aged 3-22 years to assess the likelihood of ASD. It consists of 42 items and can be completed by parents or professionals familiar with the subject’s behaviors. The scale includes three subscales: Stereotyped behaviors, communication, and social interactions, each comprising 14 items. The participant rates the frequency of behaviors using a four-point scale: “Never," “Rarely," “Sometimes," and “Often," which are scored as 0, 1, 2, and 3, respectively. Scores from each subscale are summed to obtain a single overall score indicating the probability of ASD (28). Raw scores from these subscales are further converted into standardized scores to assess the severity of ASD. The Persian version of GARS-2, which was prepared and validated by Samadi and McConkey, has been noted to have high validity and reliability (29).
3.13.2. Sensory Profile 2
Sensory profile 2 is a standardized measurement tool developed by Dunn in 2014 to evaluate sensory processing abilities of children at home and in the community (27). It has been specifically designed for children aged 3 - 14 years and consists of items rated on a six-point Likert scale, assessing various sensory patterns: Sensory seeking (SK), sensory avoiding (AV), sensory sensitivity (SN), and sensory registration (RG). These patterns are determined based on cut-off values reflecting the individual’s sensory responsiveness compared to his/her peers in the form of “much less than others", “less than others", “similar to others", “more than others", and “much more than others" (27). The Persian version of SP2 was prepared and analyzed for its psychometric properties by Shahbazi et al. and was proved to be valid with highly reliable (30).
In this study, both GARS-2 and SP2 were administered by a trained occupational therapist in the presence of parents and professionals familiar with the participant. The scorers followed the guidelines provided in the respective manuals to ensure accurate completion and scoring of the tools. The Persian versions of GARS-2 and SP2 were utilized, whose validity and reliability were approved for assessing ASD and sensory processing in the target population.
The SP2 scale was used to determine the primary outcome measure used to evaluate the impact of the interventions on the child’s sensory processing abilities. This scale was administered before and after the intervention and analyzed by trained professionals.
3.14. Statistical Analysis
Statistical analysis involved various tests to evaluate the effectiveness of the intervention and seek possible relationships hidden in the collected data. Different statistical methods were utilized for different purposes. Independent samples t-test was employed to compare continuous variables, such as age, between the intervention and control groups. Paired t-test was used to assess changes within each group before and after the intervention. This test allowed for the comparison of dependent variables within the same group. The Mann-Whitney U test, a non-parametric test, was utilized to compare the distribution of values between the intervention and control groups when the assumptions required for the t-test were not met or when the variables under analysis had a non-normal distribution. The Wilcoxon test, also a non-parametric test, was used for paired observations and to evaluate changes within each group before and after the intervention. The chi-square test was applied to analyze categorical variables, such as gender and ASD severity, and determine if their distribution was significantly different between the study groups. All statistical analyses were performed using SPSS version 26. The significance level was set at 0.05, indicating a 95% confidence level.
4. Results
A total of 51 children with ASD were included in the study. There were no significant differences between the intervention and control groups in terms of children’s age, gender, and ASD severity. Most children in both groups were male (N = 39) and diagnosed with moderate ASD (N = 33). The chi-square test (for gender and ASD severity) and independent samples t-test (for age) were employed to assess if there were significant differences between the study groups regarding these baseline characteristics. The results indicated no significant differences between the intervention and control groups in terms of age, gender, and ASD severity (P > 0.05), suggesting that the groups were comparable at the baseline for these variables. Table 2 displays the demographic information of the study participants.
| Demographics | Intervention Group (n = 26) | Control Group (n = 25) |
|---|---|---|
| Gender, No. (%) | ||
| Male | 20 (76.9) | 19 (76) |
| Female | 6 (23.1) | 6 (24) |
| Mean age (mo) | 55.88 | 56.52 |
| ASD severity, No. (%) | ||
| Mild | 10 (38.46) | 8 (32) |
| Moderate | 16 (61.54) | 17 (68) |
Demographic Information of Participants
The effect of the intervention on sensory patterns was assessed by the SP2 scale. Table 3 presents the mean scores of participants with “beyond normal" performance in each of the four sensory patterns based on the Dunn sensory processing model before and after the intervention in each study group.
| Variables | Pre-intervention | Post-intervention | P-Value | |
|---|---|---|---|---|
| Between Groups | Within Groups | |||
| Sensory seeking | 0.43 b | |||
| Intervention (n=12) | 64.66 ± 12.47 | 56.50 ± 9.22 | 0.000 c | |
| Control (n=13) | 67.15 ± 11.56 | 60.15 ± 12.54 | 0.000 c | |
| Sensory avoiding | 0.030 b | |||
| Intervention (n= 13) | 59.38 ± 10.52 | 50.84 ± 7.06 | 0.000 c | |
| Control (n= 12) | 55.41 ± 6.20 | 50.83 ± 4.96 | 0.000 c | |
| Sensory sensitivity | 0.000 d | |||
| Intervention (n= 13) | 55.61 ± 11.22, 52 | 46.30 ± 8.90, 45 | 0.002 e | |
| Control (n= 12) | 58.16 ± 16.54, 49.50 | 56.83 ± 16.49, 48.50 | 0.011 e | |
| Sensory registration | 0.000 b | |||
| Intervention (n= 11) | 58.18 ± 14.04 | 50.18 ± 11.58 | 0.000 c | |
| Control (n= 11) | 57.09 ± 13.70 | 55.81 ± 13.40 | 0.026 c | |
Mean Scores of Sensory Patterns at Pre- and Post-intervention a
It should be noted that there are four possible sensory processing patterns according to the SP2 scale, including SK, AV, SN, and RG. In this study, only the scores related to “beyond normal" patterns were analyzed. This was because normal processing patterns were not affected by the interventions. On the other hand, the number of children with “below normal" range was limited, disallowing to be statistically analyzed. A decrease in scores indicated improvement in sensory processing and approaching the normal pattern.
For all four sensory processing patterns, post-intervention scores significantly decreased compared to pre-intervention in both groups (P < 0.05), indicating that both types of interventions offered in both groups were effective in improving sensory patterns in ASD children (i.e., the within-group effect).
To compare the effectiveness of the two treatments (i.e., sensory play intervention and common sensory intervention) between the two groups, changes in respective scores for all sensory patterns before and after the interventions were compared. For the SK pattern, there was no significant difference in the mean score change between the two groups before and after the intervention (P > 0.05). However, regarding the other three sensory patterns, including AV, SN, and RG, the intervention group (but not the control group) showed significant declines in respective scores after the intervention (P < 0.01), indicating the higher effectiveness of sensory play activities with parent involvement compared to the common sensory intervention.
5. Discussion
The present study aimed to evaluate the effectiveness of SIT and investigate whether the addition of parent engagement through a sensory play activity program in treatment would lead to greater improvement in sensory processing patterns for children with ASD. Previous studies investigating the effects of sensory interventions on sensory processing patterns and performance skills in children with ASD have yielded inconsistent results (15, 31). Some studies (18, 32-37) have reported positive effects of sensory interventions on sensory processing patterns, functional capacities, and adaptive behaviors in children with ASD. However, other studies (19, 38-40) have declared limited to moderate effectiveness for sensory interventions. The findings of the present study were consistent with the studies supporting the effectiveness of sensory interventions.
There are several reasons for the inconsistency observed in the effectiveness of sensory interventions, particularly SIT. These may include the lack of a universal and standard definition for sensory integration interventions, the heterogeneity of participants in terms of ASD severity and the presence of co-morbidities, the use of non-standardized outcome measurement tools, and the lack of individualized sensory programs for each child (12). For instance, studies that used the same predetermined sensory diet for all participants or only utilized therapy ball chairs as a sensory intervention have reported limited effectiveness (39, 40). However, studies that adhered to ASIT principles, an evidence-based approach according to systematic reviews, have shown greater effectiveness and better results (12, 17).
In the present study, factors such as the use of SP2 as a specialized and standardized sensory measurement tool, personalizing SIT based on each participant's needs, and compliance with ASIT principles (i.e., tailoring activities to presenting the “just-right challenge", supporting intrinsic motivations to play, and establishing a therapeutic alliance with the child) seem to contribute to the observed effectiveness of SIT. The results of the present study demonstrated significant improvements in all four sensory patterns in both study groups compared to the pre-intervention. However, between-group comparisons revealed that parental engagement in sensory games at home (i.e., the intervention group) led to a significantly greater improvement in sensory processing patterns, probably by reducing disturbance in auditory, visual, and tactile sensory patterns.
Consistent with previous research, the findings of this study highlighted the importance of parental engagement in ASD children's treatment and child-centered therapeutic approaches that prioritize child-parent cooperation and relevant problem-solving strategies (41-43). The active participation of parents in the treatment of ASD can increase their knowledge about their children's sensory challenges, facilitate the use of coping strategies, and promote the application of environmental adaptations (44-46).
Based on an ecological theory, parents' participation in treatment has been identified as an effective factor in increasing their internal motivation to adhere to treatment. The interactive nature of both the physical and social environment and their adaptations have also been emphasized in previous research (47-49). As the most important component of an ASD child's social environment, the family's active engagement in treatment can improve therapeutic outcomes and the consequences of occupational therapy interventions (50, 51).
In the present study, we incorporated two important interventional components of occupational therapy, namely play as a communication tool and motivational medium (play as a means) and parent engagement in the child's treatment process by teaching necessary environmental adaptations according to the Person-Environment-Occupation-Performance-Engagement (PEOP-E) model, and observed substantial improvements in the sensory processing patterns of children with ASD. However, in the case of the SK pattern, there was no significant difference in the recovery rate between the intervention and control groups. One possible explanation for this finding could be that in most sensory interventions, the main emphasis is on vestibular and proprioceptive activities, which are the main senses involved in the impairment of this sensory pattern. Also, most adaptations for therapeutic activities in the clinic and play activities taught to parents are related to these two modalities, and perhaps that is why the effects of both interventions on the SK pattern were similar (40, 52).
In the present study, we were not able to include children and families from other clinics, which might have limited the diversity of participants. To address this limitation and prevent data contamination, therapeutic sessions were held in different clinical spaces on different days, and efforts were made to prevent participants from meeting each other and being aware of each other's treatment process as much as possible. Additionally, some parents in the intervention group were unable to attend all in-person therapeutic sessions at the scheduled time, for whom compensatory meetings were scheduled to ensure that they would receive the same number of therapy sessions as planned.
In the present study, several measures were considered to eliminate potential sources of bias and imprecision. Inclusion criteria were clearly defined and applied consistently to ensure the enrollment of a representative sample of children with ASD. Randomization was used to allocate participants to the intervention and control groups, minimizing selection bias. Standardized assessment tools, such as the SP2 scale, were employed to measure outcomes, also reducing the risk of measurement bias. Assessments were conducted by trained professionals who were blinded to group assignments, further enhancing the objectivity of the data collected. To minimize the impact of confounding factors, baseline characteristics were assessed and matched so that there were no significant differences between the study groups in terms of age, gender, and ASD severity. Contamination between groups was addressed by holding therapeutic sessions in separate spaces and minimizing interaction between participants. Precision was enhanced by recruiting an adequate sample size and appropriate statistical analyses as indicated (e.g., t-test and the chi-square test to compare outcomes between groups). Nonetheless, it is important to acknowledge that there might still be other sources of bias and imprecision in our study. Future studies are recommended to consider additional measures, such as conducting independent assessments by multiple raters and controlling for unidentified confounding variables. By addressing potential sources of bias and imprecision as much as possible, we were able to secure acceptable validity and reliability for our findings, providing a more robust understanding of the effectiveness of sensory integration therapy and parental engagement in the treatment of children with ASD.
The external validity of our findings is supported by the fact that the interventions were agreed upon and approved by a group of occupational therapists familiar with the field of pediatric occupational therapy. The contribution of multiple therapists, both inside and outside the research team, enhanced the credibility and external validity of the combinational intervention employed in this study, suggesting its applicability and effectiveness for children with mild to moderate ASD.
Regarding our findings’ generalizability, the educational background of parents was taken into consideration when preparing sensory play activities by presenting their instructions in simple language. This approach ensured that the intervention could be easily understood and implemented by parents with a high school diploma. By making the intervention accessible to a broader range of parents, the generalizability of our findings improved, allowing for the widespread adoption and implementation of the intervention employed here.
It is important to note that despite the efforts made to enhance the external validity and generalizability of the findings, our study may still harbor certain limitations. For example, the study sample population may not fully represent the entire population of children with ASD, so the findings may not be applicable to children with more severe ASD or those with additional comorbidities. Moreover, cultural factors and contextual differences may influence the generalizability of our findings to patients living in other regions or cultural settings.
In summary, the involvement of occupational therapists in approving the intervention, and the use of accessible language for instructions enhanced the external validity and generalizability of the findings. However, it is important to consider the aforementioned potential limitations. Further research is needed to validate the present study’s findings and verify if they can be generalized to other children with ASD, especially those with more severe disease. Also, these limitations can be resolved by adding a follow-up phase to measure the stability of the effects of the intervention. Family outcome measures can also be employed to assess the effectiveness of the intervention on parents’ quality of life, stress, and parenting efficacy. Conducting a study to engage parents in the intervention according to the standard principles of coaching and comparing outcomes with a family-oriented educational intervention can also be considered. Furthermore, family-related variables (such as the socio-economic level, parents’ jobs, the number of children, etc.) can be considered to provide further insights into the effectiveness of parent engagement in occupational therapeutic interventions for children with ASD.