1. Background
Sleep is one of the most important natural and biological cycles. Sleep is affected by two factors: Circadian sleep processes and sleep homeostasis (night sleep adequacy, sleep quantity, and daily sleepiness). Regarding the high frequency of sleep disorders and the importance of sleep quality in psychological well-being, sleep quality is considered an essential indicator of health (1). High-quality sleep can help mental and physical reconstruction because cellular repair and mental relaxation depend on the quality and quantity of sleep (2).
Obstructive sleep apnea (OSA) is among the most common respiratory sleep disorders associated with various complications and even mortality (3). The prevalence of OSA in Iran has been reported as 44% (4). The symptoms of OSA include fatigue, daytime drowsiness, poor sleep quality, impaired concentration, memory loss, and headaches. These complications significantly affect OSA patients’ health, mood, and quality of life (3). Also, OSA is usually associated with cognitive dysfunctions (e.g., memory deficits), and all components of memory may be affected by OSA (5). Furthermore, OSA significantly impairs daily performance (for example, causing traffic accidents) and can result in reduced productivity (6).
The physical effects of OSA and their treatments have been widely examined, but the psychological aspects of OSA, especially anxiety, have only been recently valued by researchers (7). Previous studies’ findings indicate a bidirectional relationship between OSA and anxiety; nevertheless, OSA management guidelines often neglect such an interaction. The prevalence of anxiety in OSA patients ranges from 11% to 70% (8). Although the risk of anxiety is high among patients with OSA, the exact link between these two disorders is unknown. Electroencephalography (EEG) changes in OSA include EEG slowing (characterized by increased low-frequency activity in the delta and theta waves during prolonged waking) and rapid eye movement (REM), which is associated with increased drowsiness, fatigue, and attention deficits (9).
Continuous positive air pressure (CPAP) is the treatment of choice for OSA (10). However, previous studies have reported inconsistent results for the effects of CPAP on mood in patients with OSA (11). This inconsistency may be due to differences in patients’ characteristics, mood assessment methods, and an overlap between mood changes and OSA-related symptoms in these studies. So, although CPAP seems to improve mood changes, more comprehensive studies are needed to confirm its effectiveness (12). Previous studies have also shown improvements in some mental status subscales, such as depression and anxiety, following CPAP therapy. However, there is little information about the effect of CPAP on sleep-dependent memory stabilization.
Compassion-focused therapy (CFT) is an integrated and multifaceted therapeutic approach rooted in evolutionary, social, and developmental concepts, as well as Buddhist psychology and neuroscience. The primary focus of this therapy is compassionate mind training to help individuals develop and engage with inner warmth experiences and achieve safety and peace through feeling compassion for others and themselves (13). The definition of compassion in CFT is based on the Buddhist tradition, which defines compassion as sensitivity to the suffering of oneself and others with a commitment to reducing and preventing suffering (14). Compassion-focused therapy encourages clients to focus on, understand, and feel compassion for themselves, compassion for others, as well as others' compassion towards themselves, and obtain skills to cope with negative thoughts instead of suppressing them. It appears that CFT may have many psychological benefits (13). Based on Jung’s theory, CFT affects survival-seeking behaviors of individuals by producing positive emotional attitudes toward oneself, through which one extends feelings of kindness and care toward oneself (15). It also helps motivate productive behaviors and protect against the debilitating effects of personal judgment, including depression and anxiety. People with higher levels of self-compassion demonstrate superior psychological health than those with lower levels of self-compassion because, in these individuals, inevitable pain and a sense of failure are not reinforced and perpetuated through intense self-condemnation (16). In general, CFT theory is based on providing individuals with the skills and alliances needed to cooperate. Therefore, CFT can reduce isolation and over-identification of thoughts and feelings. This self-supporting attitude is associated with various beneficial psychological outcomes, such as reduced depression, less anxiety, and neurotic perfectionism, along with better life satisfaction (15).
The theory behind CFT pertains to three systems: Threat, drive, and soothing. The threat system refers to the response to harm and can result in fear, anger, and anxiety (17). The drive system refers to a response to the need for resources, resulting in feelings of vitality and achievement. The soothing system refers to the response to caregiving and originates from early attachments, leading to a sense of calm and peace. Compassion is affected by fear and anger, situations where compassion may seem useless and meaningless (18). Compassion-focused therapy is believed to reduce fear by developing skills required to improve self-compassion, thus countering fears by activating the drive and soothing systems (17). This phenomenon can be an intermediary factor in enhancing psychological performance and improving quality of life. Increasing self-esteem and modifying the individual’s self-communication pattern can affect one’s mental health and improve his/her sleep quality (18).
Furthermore, self-compassion can improve positive thinking, which can improve self-satisfaction and adaptation skills, maintain mental cohesion, and improve the quality of life. High self-compassion is associated with better positive emotions and moods and less negative emotions (18). Therefore, compassion-based training interventions can play an essential role in improving sleep quality.
2. Objectives
This study aimed to evaluate the effects of CFT on anxiety, memory, and sleep quality in patients with OSA.
3. Methods
3.1. Design and Population
This study was conducted as an experimental study with a control group using the pre-test/post-test design. The current study was conducted on 37 patients (13 women and 24 men) referred to the sleep clinics of the Ibn-e-Sina and Imam Reza Hospitals, Mashhad, Iran, between 2022 and 2023. Patients with an apnea index higher than 5 based on polysomnography and those who had a documented diagnosis of OSA were selected by convenience sampling and were randomly divided into the control and intervention groups. The Mashhad University of Medical Sciences Ethical Committee approved the study protocol (code: IR.MUMS.MEDICAL.REC.1400.698).
Patients were briefed about the benefits of participating in the educational sessions and were ensured that refusal to participate in the study would not affect the physician-patient relationship. It should be pointed out that the intervention was offered as an addendum to the main treatment. Furthermore, instructions were provided to the patients regarding the benefits of the routine treatment of OSA and the complications of refusing to comply with these treatments. A sleep specialist provided these instructions to the patients. Those who were willing to participate in the study were enlisted after the briefing session and then were randomly divided into study groups using drawing cards.
After receiving ethical approval, a call was made to invite those interested in participating in the CFT program at the sleep clinic of the Ibn-e-Sina and Imam Reza Hospitals in Mashhad. Furthermore, sleep specialists were asked to refer patients willing to attend the CFT program to the researcher.
Inclusion criteria were the diagnosis of OSA within the past year, having a minimum apnea index score of 5 (19), age of between 18 and 65 years old, having at least high school education, having no history of medical (cardiovascular disease, motion disorders, or major surgeries) or psychiatric diseases, not being under treatment by another psychologist, and willingness to participate in the study. Participants were excluded if they missed 2 intervention sessions, experienced stressful life events (e.g., cardiovascular disease, heart attack, or stroke), or refused to continue cooperation with the researchers.
In the next step, the patients were screened based on the inclusion and exclusion criteria, and eligible patients were invited to participate in the study. In a face-to-face meeting, participants were subjected to a psychiatric interview based on the Structured Clinical Interview for DSM (SCID) to rule out psychiatric disorders and encounters with life stressors in the last six months. Furthermore, the possible benefits of the program were explained to the participants. The participants were then asked to sign a written informed consent form before being randomly divided into the intervention (n = 19) and control (n = 18) groups based on their will. Both groups completed the study’s questionnaires at the baseline and the end of the study period.
3.2. Instruments
3.2.1. Pittsburg Sleep Quality Index
The Pittsburg Sleep Quality Index (PSQI) is a 19-item standard questionnaire for estimating sleep quality. The tool has seven domains, including personal opinions about sleep quality, sleep duration, sleep latency, habitual sleep efficiency, sleep disturbances, the use of sleeping medications, and daytime dysfunction. Each item was scored based on a 3-point Likert scale. Therefore, PSQI scores could range between 0 and 21, with higher scores indicating worse sleep quality. According to the questionnaire’s designers, a score greater than 5 indicates poor sleep quality. The PSQI was translated into the Persian language, and its validity was evaluated using the translation back-translation method. The questionnaire was previously validated (Cronbach’s alpha = 0.83 and validity = 0.75) (20).
3.2.2. Beck Anxiety Inventory
The Beck Anxiety Inventory (BAI) is a self-report tool that includes 21 items and evaluates physical and cognitive symptoms during the past week. The current intensity of anxiety symptoms is scored on a 4-point Likert scale (0 to 3). The total BAI score can range between 0 and 13. The Persian version of the BAI has been approved in Iran with acceptable validity (P < 0.72, r = 0.001), reliability (P < 0.83, r = 0.001), and internal consistency (α = 0.92) (21).
3.2.3. Rey Auditory-Verbal Learning Test
Auditory-verbal short-term memory can be evaluated using the California, Hopkins, and Rey auditory-verbal learning tests. Among these tests, the Rey Auditory-Verbal Learning Test (RAVLT) has been widely used in recent studies due to its simplicity, short completion time, and not being affected by anxiety and depression. The psychometric validation of the tool has been subjected to various studies in Iran. For instance, Kaviani and Mousavi (22) reported the validity and reliability coefficients of 2.70 and 2.96 (after one month), respectively, along with Cronbach’s alpha of 80.2% (22, 23).
The RAVLT includes three sections. In the first section, 15 words with irrelevant meanings (list A) are read to the participants at the rate of one word per second, and the participant is asked to memorize as many words as possible. Each remembered word is given one point, and the relevant score is obtained by calculating the mean of five repetitions. In the second section, an interference list (list B) is read to the individual, after which the participant is asked to repeat the words in list A (each correct word is given one point, and the total achieved points comprise the learning with interference score). In the third section, the participant is asked to recall the words in list A after 20 to 40 minutes (each correct word is given one point, and the total score is regarded as the delayed learning score) (3). This test is sensitive to memory deficits in cognitive disorders, including Alzheimer's. In this test, an individual’s ability to retrieve, store, and stabilize verbal information is evaluated in terms of immediate memory, recognition of interfering stimuli, and delayed memory (3). Based on a previous study, the Persian version of the tool was reported to have a reliability and validity of 0.7 and 0.62, respectively, indicating high discriminant validity (23).
3.2.4. The Rey-Osterrieth Complex Figure
The Rey-Osterrieth Complex Figure (ROCF) test is a pencil-paper test that evaluates visual drawing, visual-perceptual ability, executive functions, organizational planning, visual-spatial memory, perceptual distortion, and drawing-motor coordination. This tool is efficient in evaluating memory function in people aged over 7 years old. This test has 18 perceptual components and is implemented in three steps. In the first step, the individual is asked to copy a shape on a piece of paper (i.e., the copying step). In the second and third steps, the individual is asked to draw the shape again after three (i.e., the immediate recall step) and 30 minutes (i.e., the delayed recall step) without prior notice. The first step of the test evaluates an individual’s perceptual activity, while the second and third steps evaluate the scope/accuracy of visual memory and long-term memory retention, respectively. Each step is separately given a score based on an 18-item tailor system. Each of the 18 items is scored between 0 and 2 based on the location and details of the drawings. Therefore, the overall score can range between 0 and 36. This test has been used by various studies in Iran. The construct validity and reliability coefficients of the Persian version of ROCF were reported as 0.5 and 0.59, respectively, indicating acceptable reliability and validity (24).
3.3. Procedures
The participants were randomly assigned to either the intervention or control group based on simple random allocation using cards randomly picked by the researcher. Participants in the intervention group attended 8 sessions of the CFT program (once a week). The intervention content was designed based on a comprehensive literature review and studying previously reported effective CFT interventions, as well as a CFT package used by Kazemi et al. (17, 25, 26). A systematic review showed that CFT interventions that were held for eight or more sessions were more effective compared to CFT interventions with less than eight sessions (17). Therefore, the training intervention in this study included 8 sessions.
In each session, which lasted 90 minutes, 20 individuals participated. The sessions’ contents were designed based on the CFT reference book and tailored to the study’s objectives. At the end of each session, a task related to the objectives of the session was given to the participants. The sessions’ content included participants’ familiarization with the program and each other (the first session), three emotion control systems and their effects on a person (the second session), training culminating in breathing, concentration awareness, sleep with awareness, and self-compassion (the third session), components of compassion (the fourth session), self-compassionate image formation and exercising the best self-status and imagination of a safe environment (the fifth session), thinking and its relationship with emotions and differences between threat-concentrated mind and compassionate mind (the sixth session), writing a compassionate letter to one-self and exercising the compassionate chair technique (the seventh session), and concluding remarks on previous sessions and revising the program (the eights session).
The control group received no intervention other than the routine medical treatment for OSA. However, the intervention content was provided to the participants of the control group who were willing to have the material and participate in a sample session of the program.
3.4. Statistical Analysis
Data were analyzed using the statistical package for social sciences (SPSS) software version 23. The normality of the data was evaluated using the Shapiro-Wilk test. Normally distributed variables were presented using mean and standard deviation, while non-normally distributed variables were presented using median and first and third quartiles. Categorical variables were presented using frequency and percentage. Between- and within-group comparisons of normally distributed continuous variables were performed using the independent and paired sample t-tests, respectively. Between- and within-group comparisons of non-normally distributed variables were conducted using the Mann-Whitney and Wilcoxon tests, respectively. The level of statistical significance was determined as P < 0.05.
4. Results
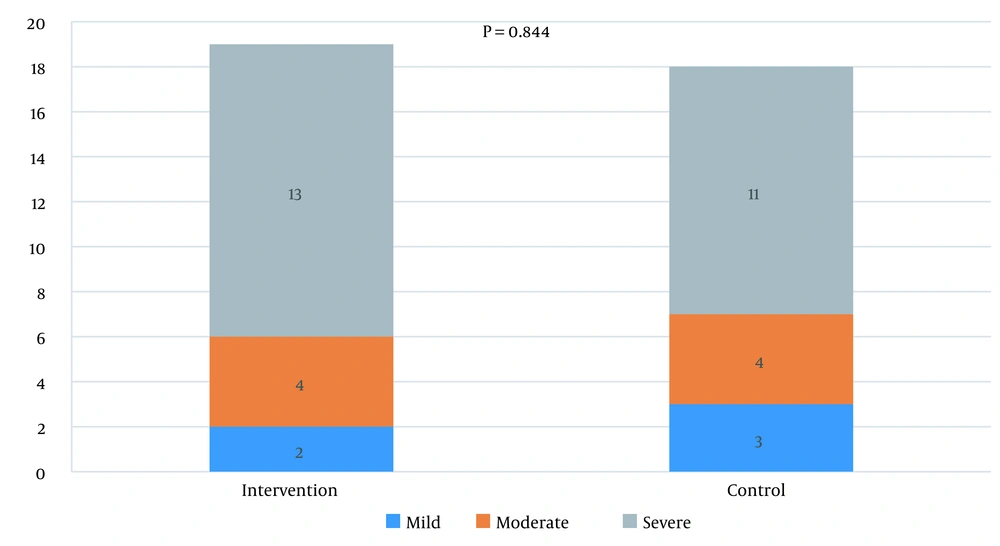
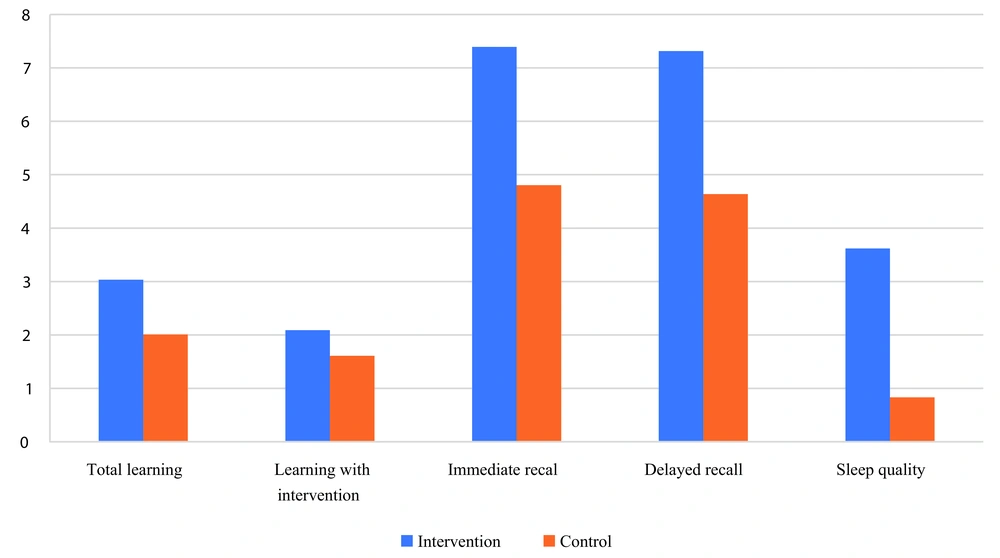
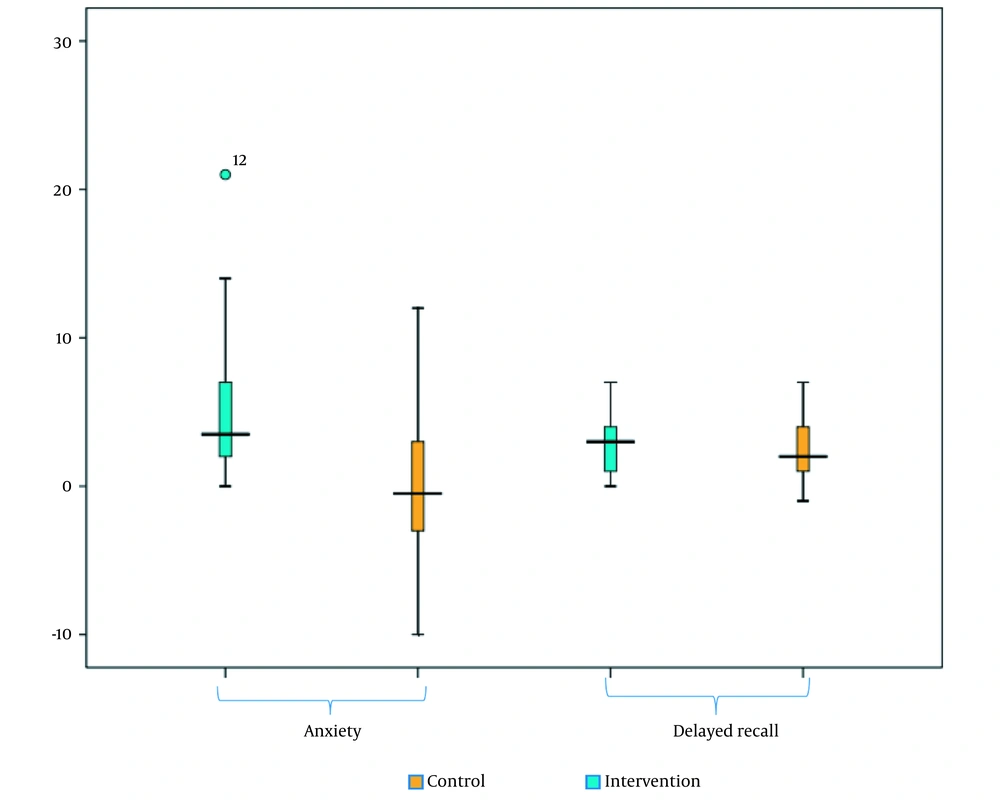
This study included 37 patients with OSA, who were randomly allocated into the intervention (n = 19) and control (n = 18) groups. The means and SDs of age of the participants in the intervention and control groups were 50.74 ± 10.34 and 53.56 ± 9.84 years old, respectively. There was no significant difference between the groups in terms of age (P = 0.402). The demographic characteristics of the participants in the two groups have been compared and presented in Table 1. There was no significant difference between the groups in terms of demographic variables. A comparison of OSA severity between the two groups (Figure 1) showed no significant difference between the two groups in this regard. Regarding anxiety, PSQI, and memory performance scores, the characteristics of patients in the intervention and control groups at the baseline and the end of the study have been presented in Table 2. Regarding changes in anxiety, PSQI, and memory performance scores in the intervention and control groups, as presented in Table 3 and Figures 2, and 3, there was a significant difference in changes in the BAI anxiety score (P = 0.002), PSQI score (P = 0.002), total learning score (P = 0.024), and immediate memory performance (P = 0.022) between the intervention and control groups. Our findings indicated that changes in the above-mentioned scores were significantly higher in the intervention group than in the control group.
| Variables | Total, N = 37 | Intervention, n = 19 | Control, n = 18 | P |
|---|---|---|---|---|
| Gender | 0.109 a | |||
| Male | 24 (64.68%) | 9 (43.37%) | 10 (52.63%) | |
| Female | 13 (35.14%) | 4 (22.2%) | 14 (77.78%) | |
| Education level | 0.999 b | |||
| Below high school diploma | 1 (2.7%) | 0 (0.00%) | 1 (5.56%) | |
| High school diploma | 23 (62.16%) | 12 (61.16%) | 11 (61.11%) | |
| Bachelor/masters | 9 (24.32%) | 5 (26.32%) | 4 (22.22%) | |
| Doctorate | 4 (10.81%) | 2 (10.53%) | 2 (11.11%) |
a The chi-square test was used for comparison.
b Fisher’s exact test was used for comparison.
| Variables and Groups | Baseline | After the Intervention | P |
|---|---|---|---|
| Anxiety score | |||
| Intervention | 12.00 (1.00) | 8.00 (5.00) | < 0.001 a, b |
| Control | 12.50 (9.50) | 12.5 (8.50) | 0.876 a |
| PSQI score | |||
| Intervention | 8.00 (6.00) | 4.00 (2.00) | 0.001 a, b |
| Control | 7.67 ± 2.61 | 6.83 ± 2.26 | 0.096 c |
| Total learning score | |||
| Intervention | 9.68 ± 12.74 | 12.74 ± 2.02 | < 0.001 b, c |
| Control | 3.04 ± 0.27 | 2.01 ± 0.23 | < 0.001 b, c |
| Learning with intervention score | |||
| Intervention | 10.00 (6.00) | 13.00 (4.00) | < 0.001 a, b |
| Control | 8.97 ± 2.73 | 10.78 ± 1.93 | < 0.001 b, c |
| Delayed learning | |||
| Intervention | 10.00 (5.00) | 13.00 (3.00) | < 0.001 a, b |
| Control | 10.00 (4.00) | 8.00 (4.50) | 0.001 a, b |
| Visual memory score | |||
| Intervention | 35.00 (2.00) | 36.00 (0.00) | 0.007 a, b |
| Control | 34.50 (3.63) | 36.00 (1.25) | 0.005 a, b |
| Object copying score | |||
| Intervention | 35.00 (2.00) | 36.00 (0.00) | < 0.001 a, b |
| Control | 34.50 (3.63) | 36.00 (1.25) | < 0.001 a, b |
Abbreviation: PSQI, Pittsburg sleep quality index.
a Median and interquartile range were presented, and the Wilcoxon test was used for comparison.
b Indicates a significant difference.
c Mean and standard deviation were presented, and the paired t-test was used for comparison.
| Variables | Intervention | Control | P |
|---|---|---|---|
| Anxiety score change | 4.00 (5.00) | -0.50 (0.00) | 0.002 a, b |
| PSQI score change | 3.62 ± 0.71 | 0.83 ± 0.47 | 0.002 b, c |
| Total learning score change | 3.036 ± 0.27 | 2.01 ± 0.23 | 0.024 b, c |
| Learning with intervention score change | 2.09 ± 0.42 | 1.61 ± 0.37 | 0.052 c |
| Delayed learning score change | 3.00 (4.00) | 2.00 (2.25) | 0.327 a |
| Immediate visual memory score change | 7.44 ± 3.23 | 5.166 ± 3.185 | 0.038 b, c |
| Delayed visual memory score change | 6.815 ± 4.09 | 5 ± 3.74 | 0.168 c |
| Object copying score change | 1.00 (2.00) | 1.00 (2.62) | 0.587 a |
Abbreviation: PSQI, Pittsburg sleep quality index.
a Median and interquartile range were presented, and the Mann-Whitney test was used for comparison.
b Indicates a significant difference.
c Mean and standard deviation were presented, and the independent t-test was used for comparison.
5. Discussion
This study was conducted to evaluate the effects of CFT training on sleep quality, anxiety, and memory performance in patients with OSA. The findings of this study showed that CFT significantly improved anxiety and sleep quality, as well as total learning and immediate memory. It was previously shown that CFT training explicitly targeted the development of compassion for oneself and others and, thus, augmented mindfulness and self-compassion (17).
This study showed that the training of CFT components improved sleep quality, as evidenced by reduced PSQI scores in the intervention group. This finding was consistent with previous research that confirmed the effectiveness of self-compassion-based interventions in improving sleep quality (27, 28). For example, a meta-analysis of 17 studies that examined the relationship between self-compassion and sleep quality reported that high self-compassion was associated with better sleep quality. Self-compassion has been identified as an emotion regulation strategy that can alleviate distressing symptoms and reduce general distress (27). The mechanism for this effect may be attributed to empowering individuals to stay calm and regulate their critical thoughts and feelings that demonetize sleep quality (28).
This study showed that CFT significantly reduced anxiety compared to the control group. This finding was consistent with the findings of previous studies (29, 30). The direct mechanism for this effect can be attributed to the effects of CFT on rumination and worry levels (30). This study also showed that CFT had a significant effect on verbal-auditory short-term memory (i.e., the general learning score) and visual-spatial short-term memory (i.e., the immediate recall score) as indicators of working memory. The mechanism for this effect can be justified based on the biased competition theory, noting that cognitive activities, including selective attention and memory, are improved as the result of an improvement in mindfulness (31). This finding was in line with studies that showed mindfulness could improve working memory (32, 33). At the same time, this study showed that CFT did not affect verbal-auditory long-term memory and visual-spatial long-term memory. This finding was in line with the findings of a meta-analysis that reported that although some studies showed improvements in long-term memory parameters, the overall effect was non-significant (34). Therefore, mindfulness training boosts working memory capacity by enhancing mindfulness, allowing individuals to use working memory more effectively by restricting irrelevant information and expanding the capacity of working memory to accommodate more information. Moreover, since mindfulness exercises employ attention skills, there is a possibility that one reason for improving working memory in this study may be an improvement in concentration and attention and maintaining information in the mind by increasing attention and awareness.
On the other hand, the findings of this study showed that although CFT improved long-term memory, this effect was not statistically significant. This finding was in line with the report of a meta-analysis of 25 studies (n = 1439), declaring that mindfulness interventions could not significantly affect attention, working memory, and long-term memory. At the same time, a small effect was observed on executive function (34), the mechanism of which can be attributed to the increase in self-awareness and sensitivity to one’s inner feelings, as well as the feelings of others (35). All these benefits are closely related to communication skills.
Overall, this study’s findings indicated that the CFT program was effective in reducing anxiety and improving the quality of sleep and short-term memory in patients with OSA. It is also possible that some well-being outcomes are more apparent as the impact of compassion is indirect. For example, psychological outcomes such as improved sleep quality and anxiety may be more apparent than outcomes such as memory and brain wave changes, leading some people to feel worse before and feel better in response to compassion. It should also be taken into mind that people have different emotional responses to different exercises.
One of the limitations of this study was the possible differences in responses to the intervention due to different underlying causes of sleep apnea. Although the findings of this study indicated beneficial effects, further studies should be conducted specifically on each etiological group of sleep apnea. Another limitation of this study was the inability to compare outcomes between genders. Although the gender distribution was similar in both the intervention and control groups, statistical comparison was not applicable in this study due to the small number of females and males in each group. Therefore, further studies should be conducted on larger populations to be able to conduct gender-stratified comparisons.
5.1. Conclusions
The findings of this study showed that CFT could improve the quality of life in patients with OSA by reducing anxiety and improving sleep quality and short-term memory. Therefore, CFT could be used as an effective complementary method to manage OSA. However, there is a need for further studies with long-term follow-up to determine the durability of the effects of CFT components on these parameters.