1. Background
Breast cancer is defined by the unchecked proliferation of abnormal cells in the breast tissue, capable of invading adjacent tissues and spreading to distant organs via lymphatic channels and the bloodstream (1). It stands as the most prevalent cancer among women globally and the second leading cause of cancer-related mortality in women, following lung cancer (2). In the United States, approximately 3.1 million women with a history of breast cancer are living, and more than 200,000 new cases are diagnosed each year (3). In Iran, up to 2016, there were about 40,000 cases of breast cancer, with around 7,000 new cases identified annually (4). A meta-analysis of 12 countries worldwide indicated that Iran experienced the highest prevalence of breast cancer at 57.1%, whereas the UK had the lowest at 8.9% (5). Moreover, over 40% of patients were in the 40 - 50 age range, and the average age at diagnosis for Iranian women was younger compared to other countries (6).
Patients with breast cancer often face mental health challenges due to pain, fear of death, diminished functionality, complications from treatments, and a lack of financial and social support (7). A prevalent issue among these patients is disturbances in body image. Body image encompasses a person's perception of their physical appearance and their attitudes and perceptions regarding how they believe they are viewed by themselves and others (8). It is comprised of three components: Perceptual, cognitive, and behavioral. The perceptual component involves how a person sees and evaluates their physical appearance, the cognitive component relates to their satisfaction or concerns about their appearance, and the behavioral component is associated with actions taken to avoid distress and anxiety related to body image (9). Studies have identified a positive link between poor body image and various adverse outcomes, including depression, lower quality of life, unhealthy behaviors, and interpersonal issues in breast cancer survivors (10). The perception of breasts as symbols of femininity, attractiveness, and sexuality means that breast cancer can profoundly affect a woman's body image (11). Research has documented that alterations resulting from surgical procedures, chemotherapy (e.g., hair loss), and radiation (e.g., burns) can reduce perceived attractiveness (12) and lead to social challenges, such as avoiding social interactions, concerns about acceptance by partners or others, fear of negative judgments, increased sensitivity, and dissatisfaction with body image (13). This fear of negative assessment by others can amplify body image dissatisfaction, potentially culminating in depression and reduced self-esteem (14).
Studies have shown that patients with breast cancer frequently encounter challenges in their interpersonal relationships, with interpersonal stress being a prevalent issue (15). This stress can stem from disputes, tense discussions, and worries about offending the feelings of family, friends, and colleagues (16). It is identified as the most commonly experienced form of stress in daily life, with its adverse effects being more severe than those of other stressors (17). Interpersonal stress significantly affects quality of life, physical health, and functionality, suggesting it may heighten the risk of depression (18). Approximately 10 - 30% of cancer patients display clinical symptoms of post-traumatic stress at the time of their diagnosis (19).
Moreover, changes in physical appearance due to weight gain and surgical scars can adversely impact marital satisfaction, intimacy, and sexual relationships, including the frequency and pleasure of sexual activity, thereby increasing stress and diminishing marital satisfaction (20). The research underscores the importance of effective communication for coping with cancer, highlighting that the social interactions of cancer patients directly influence their physiological symptoms. This includes the function of glands, heart, immune system, stress hormone levels, energy, and fatigue. Additionally, interpersonal dynamics significantly affect their psychological well-being, encompassing relationship satisfaction and compliance with medical advice (21).
The identification of communication patterns has been recognized as beneficial in facilitating psychological adjustment and coping mechanisms in cancer patients. Given the crucial role of interpersonal communication in managing cancer, a wide array of intervention opportunities exists (21).
Several psychological interventions have proven to improve both the physical and psychological health of patients with breast cancer, among which cognitive-behavioral therapy (CBT) stands out. Despite CBT's widespread application and its generally positive outcomes, recent research suggests that its mental health benefits for cancer patients, especially those with breast cancer, are moderately effective at best (22). Moreover, CBT has been deemed ineffective in enhancing the quality of life or alleviating psychological distress among cancer patients facing significant psychological challenges (23). Compassion-focused therapy (CFT) represents an innovative psychotherapeutic approach that incorporates elements of CBT, such as reevaluating thoughts, targeting behavioral changes, and utilizing imagery. However, CFT uniquely integrates concepts from attachment and evolutionary theories, neuroscientific findings, and insights into compassion (24). Compassion-focused therapy offers a more promising method for addressing prevalent psychological issues in cancer patients by promoting an acceptance and compassionate understanding of their experiences rather than avoiding or suppressing negative emotions (25).
Randomized clinical trials (RCTs) have demonstrated the therapeutic effectiveness of CFT in mitigating psychological issues and enhancing mental health in individuals with multiple sclerosis (26). Additionally, CFT has been found to reduce perceived stress and psychological distress (27), decrease rumination and anxiety (28), and improve body image and marital satisfaction in women diagnosed with breast cancer (29). Despite these findings, limited research has been conducted on the effectiveness of CFT in cancer patients, particularly women with breast cancer, and further investigation is warranted in this area. Therefore, this study aimed to assess the effectiveness of CFT in improving body image and interpersonal stress in women diagnosed with breast cancer.
2. Objectives
The objectives of this study were established as follows:
(1) To ascertain the average body image and interpersonal stress scores, including their respective subscales, within both groups.
(2) To compare the average scores for body image and interpersonal stress, alongside their subscales, within both groups before and after the intervention and at the follow-up stage.
(3) To assess the efficacy of group CFT in improving body image and reducing interpersonal stress among women with breast cancer.
(4) To evaluate the range of impact, from least to greatest, that CFT had on the subscales of these 2 variables.
3. Methods
3.1. Participants
Using G*Power version 3.1 (30), a repeated measures analysis of variance (ANOVA) was conducted with a test power of 0.80, an alpha level of 0.05, and a medium effect size (0.53) based on a similar study (27) comparing two groups across three measurement points. The analysis determined that a total of 38 participants would be appropriate for this study, allocating 19 participants each to the experimental and control groups. To accommodate potential dropouts and to enhance the sample size by 15%, 44 women diagnosed with breast cancer, aged between 30 to 57, were chosen from Yasrebi and Beheshti Hospitals in Kashan through convenience sampling. They were randomly assigned to both the experimental and control groups, with 22 participants in each. The random assignment of eligible participants to the CFT and control groups was facilitated using a randomization website designed for psychological experiments, medical trials, and field studies at www.randomizer.com.
Additionally, three different individuals were responsible for conducting evaluations, interventions, and analyses. The inclusion criteria specified for participation in the study were a current diagnosis of breast cancer confirmed by an oncologist, a minimum of an elementary education level, and a willingness to participate. The exclusion criteria included the presence of any mental disorder or other physical illnesses, participation in other psychotherapy sessions, or the use of psychiatric medications. The groups were matched in terms of surgical history, duration of cancer diagnosis, cancer medications taken, and physical treatment methods utilized.
3.2. Tools
3.2.1. Body Image Scale
The Body Image Scale (BIS) serves as a tool for assessing the body image of cancer patients. It comprises ten items that evaluate emotional, behavioral, and cognitive aspects related to body image. These items are rated using a 4-point Likert scale that ranges from 0 (not at all) to 3 (very much), where higher scores signify greater symptoms of distress or concerns about body image. The BIS is applicable across various types of cancer or treatments, offering a thorough evaluation of body image issues encountered by cancer patients. The Cronbach's alpha reliability coefficient for this scale is reported to be 0.93, indicating high internal consistency and its differential validity coefficient is considered appropriate (31). In a separate study, the Cronbach's alpha for this scale was found to be 0.94, showcasing significant convergent and divergent validities (32). Additionally, the Persian version of the BIS has shown good internal consistency (Cronbach's alpha coefficient = 0.70) and divergent validity (33).
3.2.2. Interpersonal Stress Scale
The Interpersonal Stress Scale (ISS) consists of 32 items designed to evaluate various dimensions of interpersonal stress, including conflicts with family, colleagues, friends, and relatives, stress arising from environmental changes, and stress due to alterations in personal life. Responses are scored on a 5-point Likert scale from 0 (not experienced) to 4 (very much), where higher scores reflect increased levels of interpersonal stress. Based on the study by Amiri et al. (34), Cronbach's alpha coefficients for these factors varied between 0.67 to 0.89, demonstrating good internal consistency. Furthermore, the test-retest reliability ranged from 0.69 to 0.96. The overall test-retest reliability of the ISS was recorded at 0.83.
3.3. Procedure
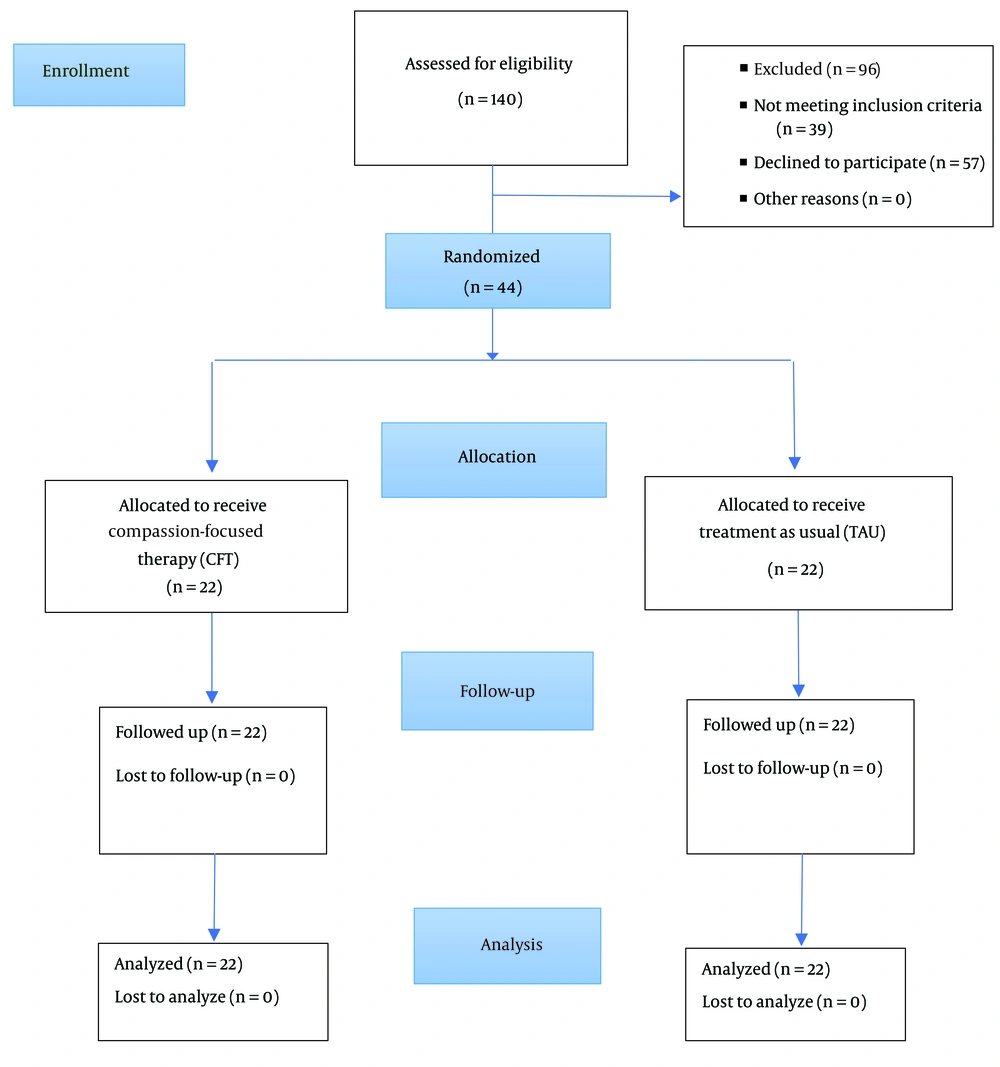
Among 140 women with breast cancer who were enrolled in the study, 44 who fulfilled the inclusion criteria were chosen to participate. Ethics approval was secured from the research ethics committee of Kashan University of Medical Sciences (IR.KAUMS.MEDNT.REC.1400.214) prior to commencing the study, which is also registered with the Iranian Registry of Clinical Trials under the code IRCT20220318054327N1. Following the acquisition of informed consent, an initial assessment was performed. Subsequently, participants were randomly allocated to either the intervention group (n = 22) or the control group (n = 22), with the allocation being concealed from them. The intervention group received eight weekly sessions of CFT administered by a clinical psychologist skilled in CFT and psychotherapy for women with cancer. Assessments post-intervention and at two months follow-up were carried out immediately after the final CFT session and two months thereafter, respectively. There was no loss of participants during the course of the study (Figure 1). Data collected were analyzed utilizing SPSS 26.
3.4. Treatment
Compassion-focused therapy is a psychotherapeutic approach aimed at fostering self-compassion and compassion towards others. This approved method includes a preliminary individual session for all participants before the main treatment, focusing on psychoeducation, normalization, and encouragement for participating in group sessions. The ensuing group sessions, each lasting between 90 to 100 minutes, featured a range of therapeutic components and CFT exercises (Table 1) (35). Up to the point of this writing and upon review by the researchers, no drawbacks have been identified concerning the efficacy of CFT for breast cancer patients.
| Session | Steps |
|---|---|
| First | Introducing the members to each other, determining the goals of the group, and introducing and explaining the general treatment approach. Assignment: Listing the most important problems that patients face. |
| Second | Introducing different types of emotions and three-affect regulation systems and soothing breathing rhythm exercises. Assignment: Practicing soothing breathing rhythm daily and recording its effects. |
| Third | Introducing multi-mind, the interaction of the old and new brains, and examining self-critical blaming and individual responsibility. Assignment: Continue practicing soothing breathing rhythm, doing a reality check on current problems, and examining their fault and responsibilities. |
| Fourth | Introducing compassion (to oneself) and its characteristics, mindfulness, and its types, practicing mindful breathing, and focusing on the object. Assignment: Practicing mindful breathing, focusing on an object daily, and recording its effects. |
| Fifth | Introducing walking, sound, and eating mindfulness practices and informal mindfulness practices. Assignment: Conducting formal and informal exercises and recording their effects. |
| Sixth | Examining the obstacles to self-compassion, examining self-criticism and its functions and effects, and introducing and implementing imagery exercises. Assignment: Recording at least five self-critical situations and doing one of the imagery exercises afterward (suitable to the situation); noting feelings and thoughts before and after the exercise. |
| Seventh | Implementing the compassionate letter writing, compassion-focused imagery exercise. Assignment: Noting three disturbing situations and then performing a compassion-focused imagery exercise, noting feelings and thoughts before and after the exercise. |
| Eighth | Examining compassion towards others, examining situations where compassion towards others may be difficult, cognitive restructuring, exercising compassion with others, concluding the sessions, and conducting the post-test. |
The 8-Session Therapeutic Protocol of Compassion-Focused Therapy Was Implemented as Follows (35)
4. Results
There were no significant differences in age between the intervention and control groups [mean = 44.77, SD = 6.65 for the intervention group and mean = 43.59, SD = 8.91 for the control group; t (42) = 0.50, P = 0.621]. A majority of the participants in both groups were married, with 86.3% in the intervention group and 95.4% in the control group being married. Regarding employment status, 68.2% of the intervention group were homemakers and 31.8% were employed, while in the control group, 81.8% were homemakers and 18.2% were employed. The educational levels differed slightly between the groups, with 27.3% of the intervention group having a primary school education, 9.1% having a middle school diploma, 31.8% having a high school diploma, and 31.8% having a bachelor’s degree, compared to 31.8%, 18.2%, 8.31%, and 18.2%, respectively, in the control group. Chi-square tests showed no significant differences between the two groups in terms of marital status, education, and employment (P > 0.05), indicating that they were comparably matched on demographic variables.
A repeated measures ANOVA was utilized to assess differences in total body image and interpersonal stress scores between the intervention and control groups across three evaluation points (pre-test, post-test, and follow-up). The findings revealed that CFT significantly alleviated body image disturbances in women with breast cancer in comparison to the control group (P = 0.001). Pairwise comparisons indicated that in both the intervention and control groups, total scores for body image disturbance significantly decreased in the post-test and follow-up phases relative to the pre-test phase (P < 0.05). However, there was no significant reduction in body image disturbance from the post-test to the follow-up phase in either group (P > 0.05). Furthermore, the effect size for the total body image score was η2 = .92, P < 0.001.
Total scores for interpersonal stress reveal that CFT significantly lowered interpersonal stress in comparison to the control group (P < 0.05). Pairwise comparisons indicated that in both groups, total interpersonal stress scores significantly decreased in the post-test and follow-up phases relative to the pre-test phase (P < 0.05). Within the control group, there was no significant change in interpersonal stress scores from the post-test to the follow-up phase (P > 0.05) (Table 2). Moreover, the effect size for the total interpersonal stress score was η2 = 0.59, P < 0.001. Consequently, CFT demonstrated a more pronounced impact on body image than on interpersonal stress.
| Variables | PR/PO/FO a (Mean ± SD) | Group | Time*Group | Within-Subject b | Post Hoc c |
|---|---|---|---|---|---|
| Total body image score | F (1, 42) = 12.40; P = 0.001, η2 = 0.23 | F (1.48, 62.10) = 46.32; P < 0.001, η2 = 0.84 | |||
| Intervention | 20.23 ± 1.97)/12.45 ± 1.71/12.77 ± 1.51 | F (1.06, 28.41) = 250.51; P < 0.001, η2 = 0.92 | PR > PO; PR > FO; PO = FO; | ||
| Control | 19.36 ± 2.04/16.54 ± 3.31/16.59 ± 3.54 | F (1.35, 22.41) = 28.88; P = 0.001, η2 = 0.58 | PR > PO; PR > FO; PO = FO | ||
| Total interpersonal stress | F (1, 42) = 5.53; P = 0.023, η2 = 0.12 | F (1.38, 58.11) = 18.11; P < 0.001, η2 = 0.30 | |||
| Intervention | 24.09 ± 8.52/15.41 ± 4.86/15.32 ± 5.27 | F (1.38, 29.02) = 30.15; P < 0.001, η2 = 0.59 | PR > PO; PR > FO; PO = FO | ||
| Control | 23.73 ± 6.62/21.86 ± 6.26/21.77 ± 6.28 | F (1.17, 24.61) = 90.28; P < 0.001, η2 = 0.81 | PR > PO; PR > FO; PO = FO |
Linear Analysis of Variance Repeated Measure for Dependent Variables
The results from the repeated measures of Linear MANOVA indicated that CFT significantly reduced all three components of body image—emotional, cognitive, and behavioral—in women with breast cancer in comparison to the control group (P = 0.001). Subsequent pairwise comparisons showed that CFT significantly diminished the emotional, cognitive, and behavioral components in the post-test and follow-up phases relative to the pre-test phase (P < 0.05). No significant differences were observed between the post-test and follow-up phases for these three components within the intervention group (P > 0.05). The effect sizes for the body image subscales ranged from 0.75 to 0.89 (P < 0.001), indicating that CFT had the least impact on the behavioral subscale and the most on the emotional component.
In the control group, significant reductions in the emotional and behavioral components were noted in the post-test and follow-up phases compared to the pre-test phase (P < 0.05). However, there were no significant differences between the post-test and follow-up phases for the emotional and behavioral components in the control group (P > 0.05). Likewise, no significant changes were found in the cognitive component across the three measurement phases (P > 0.05) (Table 3).
| Body Image Subscales | PR/PO/FO a (Mean ± SD) | Group | Time*Group | Within-Subject b | Post Hoc c |
|---|---|---|---|---|---|
| Emotional | F (1, 42) = 4.49; P = 0.04, η2 = 0.06 | F (1.24, 52.26) = 23.44; P < 0.001, η2 = 0.36 | |||
| Intervention | 9.05 ± 0.65/5.36 ± 0.90/5.64 ± 0.90 | F (1.52, 31.89) = 175.55; P < 0.001, η2 = 0.89 | PR > PO; PR > FO; PO = FO | ||
| Control | 8.27 ± 1.03/6.81 ± 1.99/7.05 ± 1.76 | F (1.08, 22.84) = 13.55; P = 0.001, η2 = 0.39 | PR > PO; PR > FO; PO = FO | ||
| Behavioral | F (1, 42) = 31.44; P < 0.001, η2 = 0.43 | F (1.37, 57.67) = 12.61; P < 0.001, η2 = 0.25 | |||
| Intervention | 3.76 ± 0.75/1.73 ± 0.77/2.00 ± 0.44 | F (1.57, 33) = 61.69; P < 0.001, η2 = 0.75 | PR > PO; PR > FO; PO = FO | ||
| Control | 3.77 ± 0.61/2.95 ± 0.84/3.14 ± 0.71 | F (1.15, 24.20) = 5.78; P = 0.002, η2 = 0.34 | PR > PO; PR > FO; PO = FO | ||
| Cognitive | F (1, 42) = 4.91; P = 0.032, η2 = 0.11 | F (1.24, 52.06) = 13.66; P < 0.001, η2 = 0.25 | |||
| Intervention | 7.41 ± 1.50 /5.36 ± 1.00/5.14 ± 1.09 | F (1.38, 28.98) = 110.85; P < 0.001, η2 = 0.84 | PR > PO; PR > FO; PO = FO | ||
| Control | 7.31 ± 1.13/6.77 ± 1.51/6.41 ± 2.06 | F (1.03, 21.54) = 5.78; P = 0.025, η2 = 0.22 | PR = PO; PR = FO; PO = FO |
Linear MANOVA Repeated Measure for Body Image Subscales
The results from the repeated measures of Linear MANOVA indicated that CFT significantly alleviated stress arising from conflicts with family members in women with breast cancer, as compared to the control group (P < 0.05). Pairwise comparisons revealed that stress due to conflicts with both family members and friends and relatives markedly decreased in the post-test and follow-up phases relative to the pre-test phase (P < 0.05). No significant differences were found in these components between the post-test and follow-up phases (P > 0.05). The effect sizes for the interpersonal stress subscales ranged from 0.01 to 0.74 (P < 0.001), suggesting that CFT had the minimal impact on stress from conflicts with colleagues and changes in personal life and the most significant impact on conflicts with family.
In the control group, stress from conflicts with colleagues significantly declined over time (P < 0.05), with significant reductions observed in both the post-test and follow-up phases compared to the pre-test phase (P < 0.05). No significant differences were noted in this component from the post-test to the follow-up phase (P > 0.05) (Table 4).
| Interpersonal Stress Subscales | PR/PO/FO a (Mean ± SD) | Group | Time*Group | Within-Subject b | Post Hoc c |
|---|---|---|---|---|---|
| Conflicts with family | F (1, 42) = 13.04; P = 0.001, η2 = 0.24 | F (1.14, 47.96) = 12.42; P = 0.001, η2 = 0.23 | |||
| Intervention | 7.09 ± 3.07/2.27 ± 1.08/2.54 ± 0.80 | F (1.07, 22.54) = 60.24; P < 0.001, η2 = 0.74 | PR > PO; PR > FO; PO = FO | ||
| Control | 7.54 ± 3.61/6.04 ± 3.05/5.78 ± 2.99 | F (1.16, 24.44) = 0.6.83; P = 0.012, η2 = 0.25 | PR = PO; PR = FO; PO = FO | ||
| Conflicts with colleagues | F (1, 42) = 3.31; P = 0.076, η2 = 0.07 | F (1.13, 47.27) = 8.52; P = 0.004, η2 = 0.17 | |||
| Intervention | 3.05 ± 2.01/2.86 ± 3.51/2.77 ± 3.24 | F (1.05, 22.12) = 0.16; P = 0.704, η2 = 0.01 | PR = PO; PR = FO; PO = FO | ||
| Control | 3.27 ± 0.88/0.91 ± 1.41/1.18 ± 1.37 | F (1.27, 26.66) = 40.21; P < 0.001, η2 = 0.66 | PR > PO; PR > FO; PO = FO | ||
| Conflicts with friends | F (1, 42) = 3.40; P = 0.129, η2 = 0.05 | F (1.09, 47.76) = 21.04; P < 0.001, η2 = 0.34 | |||
| Intervention | 7.45 ± 3.92/3.14 ± 1.70/3.41 ± 1.37 | F (1.05, 31.94) = 29.68; P < 0.001, η2 = 0.59 | PR > PO; PR > FO; PO = FO | ||
| Control | 6.32 ± 3.46/5.77 ± 3.75/5.95 ± 3.66 | F (1.23, 25.84) = 0.3.97; P = 0.397, η2 = 0.16 | PR = PO; PR = FO; PO = FO | ||
| Changes in the environment | F (1, 42) = 2.00; P = 0.165, η2 = 0.05 | F (1.72, 72.40) = 0.71; P = 0.705, η2 = 0.007 | |||
| Intervention | 3 ± 1.66/2.81 ± 2.38/3.18 ± 2.46 | F (1.52, 31.95) = 0.88; P = 0.704, η2 = 0.04 | PR = PO; PR = FO; PO = FO | ||
| Control | 2.36 ± 0.79/2.27 ± 1.20/2.36 ± 0.95 | F (1.70, 35.66) = 0.11; P = 0.869, η2 = 0.005 | PR = PO; PR = FO; PO = FO | ||
| Changes in personal life | F (1, 42) = 1.50; P = 0.227, η2 = 0.03 | F (1.14, 48.02) = 0.06; P = 0.842, η2 = 0.001 | |||
| Intervention | 3.5 ± 1.99/3.23 ± 2.25/3.41 ± 2.26 | F (1.07, 22.41) = 0.31; P = 0.599, η2 = 0.01 | PR = PO; PR = FO; PO = FO | ||
| Control | 4.23 ± 1.51/3.86 ± 2.70/4.23 ± 2.41 | F (1.15, 24.24) = 0.56; P = 0.486, η2 = 0.03 | PR = PO; PR = FO; PO = FO |
Linear MANOVA Repeated Measure for Interpersonal Stress Subscales
5. Discussion
Breast cancer can lead to adverse physical, psychological, and social effects (29, 36). This study sought to evaluate the impact of compassion-focused group therapy on body image and interpersonal stress in women with breast cancer. The findings align with previous research, indicating that CFT can improve the body image of these patients (29, 37-39). Medical interventions for breast cancer, such as mastectomy, chemotherapy-induced alopecia, and radiation therapy burns, can significantly affect an individual's perception of their physical appearance and disrupt their body image. Consequently, patients may feel shame and engage in negative self-assessment or perceive others' attitudes towards them as negative, leading to distressing emotions. These emotions activate the threat system, compelling patients to adopt protective measures and employ safety strategies like self-blame or blaming others for their issues, which can result in rumination over physical alterations, marital discord, disruption of daily routines, fear of cancer recurrence, and death anxiety (29). Compassion-focused therapy encourages self-compassion, aiding individuals in navigating the challenges posed by cancer and its consequences. Through the cultivation of self-compassion, individuals experience reduced negative emotions and are better prepared to manage difficult situations (40). Research shows that people with higher levels of self-compassion report better mental health outcomes compared to those with lower levels of self-compassion (39). Compassion-focused therapy trains patients to approach their painful inner experiences with mindfulness and compassion rather than isolating themselves socially or engaging in self-blame, which could exacerbate their condition (41). Such individuals are less inclined to self-blame or avoid social interactions when faced with inevitable pain or feelings of inadequacy (42). Patients gradually come to accept their physical states as they are, understanding that these changes are a part of their survival journey. This acceptance helps them better tolerate the painful and uncomfortable emotions associated with their altered bodies, fostering a more adaptable approach to facing these challenges. Moreover, self-compassion triggers the activation of the soothing system, which decreases fear and withdrawal behaviors, aims to regulate negative emotions, and develops coping strategies that enhance self-efficacy (43). Additionally, research has demonstrated the significant role of self-compassion in mediating the relationship between mindfulness and recovery from illness (44).
Furthermore, the findings of this study align with prior research that suggests CFT can diminish interpersonal stress in women with breast cancer (29, 45-47). This outcome can be attributed to the visible impacts of the disease, which may lower women's self-esteem and be socially acknowledged, whether deliberately or not, leading to substantial psychological distress alongside rumination (48). Women might avoid social interactions out of shame or self-blame for their condition and its complications. Conversely, attributing blame to others and harboring resentment could adversely affect their social connections. In both scenarios, the absence of social support can exacerbate negative emotions such as sadness, interpersonal tension, and stress, further fueling adverse thoughts, feelings, and self-criticism. Compassion-focused therapy, by acknowledging the neural and evolutionary underpinnings of human challenges, activates the parasympathetic nervous system and oxytocin system at a physiological level, thereby fostering psychological resilience and improved behavioral outcomes (49, 50). Socially, it fosters enhanced relationships and more adaptive behaviors free from shame (51). Recent research indicates that compassion-based practices can activate specific brain areas associated with empathy, altruism, and understanding one's own and others' emotions, potentially cultivating positive emotional states and strengthening the biological immune system (52). Through practices such as soothing imagery and compassion exercises, patients learn to extend compassion towards themselves and others. This shift in perspective can enhance mutual positive emotions and facilitate interactions with others, encouraging individuals to refrain from judgment, condemnation, or blame towards themselves (their bodies) or others, thus improving their self-relationship and social connections. Additionally, individuals with higher levels of self-compassion tend to experience less emotional turmoil and possess a better capacity for managing personal conflicts. Compassion acts as a buffer for women diagnosed with breast cancer, protecting them from the detrimental effects of both intra- and interpersonal tensions and consequently fostering improved mental health and lower stress levels (47).
Participating in therapy groups that foster mutual interaction can assist patients in recognizing that they are not isolated in their struggles, which can lead to a decrease in self-blame and body image disturbances (53). This realization, in turn, allows them to perceive their own and others' suffering without fear and to take the necessary steps to address it. Therefore, compassion-focused therapy serves as an effective approach for alleviating interpersonal stress among women with breast cancer.
5.1. Study Limitations and Suggestions
This study, like others, faced certain limitations. The participant count was modest, and the duration of follow-up was comparatively brief. Additionally, there exists a scarcity of research on interpersonal stress within the context of cancer patients. Conducted via self-reporting, this study, akin to all similar inquiries, may carry an inherent bias to some extent. One notable limitation was the lack of a comparative analysis with alternative therapeutic methods to gauge CFT's relative efficacy. Although some subscales of interpersonal stress variables did not yield significant results in this investigation, it is advisable to undertake similar studies with broader and more varied participant bases (for example, including employees and students) and to pursue further research encompassing extended follow-up periods for a more reliable evaluation of treatment efficacy. Moreover, it is crucial to compare CFT's effectiveness against other psychotherapeutic strategies, such as CBT or acceptance and commitment therapy (ACT).
5.2. Conclusions
Compassion-focused therapy represents a relatively recent addition to psychotherapeutic treatments. Despite limited extensive research, existing studies highlight its substantial positive impacts. The outcomes of this study further corroborate the effectiveness of CFT, suggesting that healthcare and treatment facilities should consider integrating psychological interventions, particularly CFT, into their offerings.