1. Background
Irritable bowel syndrome (IBS) is a functional gastrointestinal disorder that causes symptoms such as altered bowel habits, abdominal discomfort, and bloating. As per ROME IV criteria, IBS diagnosis involves experiencing abdominal pain or discomfort for at least one day per week over three months. This is coupled with two or more of these: (I) Related to defecation, (II) Altered stool frequency, or (III) Changes in stool appearance (1). IBS prevalence is 4.7% in the United States, 4.5% in Canada, and 4.6% in Britain (2). Iran's reported IBS prevalence varies between 1.1% and 25% (3). IBS significantly impacts patients and healthcare systems, reducing quality of life (1). Moreover, evaluating the quality of life is vital, shedding light on psychological, social, and physical well-being (4).
Personality is essential to health, typically assessed via the Five-Factor Model. Conscientiousness is associated with improved health. Research shows high conscientiousness relates to longer life, better health, and less smoking (5). Notably, it reduces gastrointestinal complaints in IBS patients, elevating their quality of life (6). Nevertheless, recent research indicates a U-shaped well-being connection (7), with both very low and very high conscientiousness negatively impacting well-being (8).
The Five-Factor Model of personality encompasses factors that can be further subdivided into subcomponents, offering a nuanced understanding of health outcomes. Conscientiousness includes orderliness, goal-striving, and dependability (9). In extreme cases, orderliness can mean excessive cleanliness, dependability, rigid morals, goal-striving, excessive work focus, and competence perfectionism (7). Particularly, perfectionism negatively impacts IBS patients' health-related quality of life (10).
2. Objectives
Previous research didn't investigate whether conscientiousness and IBS patients' quality of life have a linear or curvilinear connection. This study aims to discover the inverted U-shaped curvilinear relationship between conscientiousness and the quality of life in patients with irritable bowel syndrome.
3. Methods
3.1. Participants
Participants were selected from a private gastroenterologist's clinic in Tehran in 2020, and the sample size was determined using Hulley et al.'s formula (11) for correlational studies:
Using a correlation value of 0.19 from Steel et al. (12), a sample size of 215 was determined, accounting for a 0.05 type I error, 0.80 power, and 0.19 correlation. In 2020, 246 individuals were included to address potential questionnaire issues.
Inclusion criteria: IBS diagnosis by a gastroenterologist, age 18 - 40, and participant consent. Exclusion criteria: Severe psychological disorders, cancer, or inflammatory bowel disease. After providing the necessary research information, willing participants were sequentially included. Google Forms were used for the questionnaire design. Participants who gave their written consent were contacted via email or WhatsApp. This sampling process took 8 months. In total, 246 questionnaires were collected, and data from 232 questionnaires were analyzed after discarding 14 incomplete responses.
3.2. Instruments
3.2.1. NEO Five-Factor Inventory
The NEO Five-Factor Inventory (NEO-FFI) personality questionnaire contains 60 items, measuring 5 scales: Neuroticism, Extraversion, Openness to Experience, Agreeableness, and Conscientiousness. Reliability varies by country (0.66 to 0.87) (13). Conscientiousness includes the Orderliness, Goal-Striving, and Dependability sub-scales (9). Anisi reported NEO-FFI reliability and validity in an Iranian sample (14). In our study, Conscientiousness had a Cronbach's alpha of 0.875, while Orderliness, Goal-Striving, and Dependability sub-scales scored 0.807, 0.699, and 0.752, respectively.
3.2.2. Irritable Bowel Syndrome Quality of Life
The Irritable Bowel Syndrome Quality of Life (IBS-QOL) questionnaire assesses IBS-related effects with strong reliability (Cronbach's alpha of 0.95) and validity (15). Haghayegh et al. documented the reliability and validity of the IBS-QOL in a sample of Iranian individuals (16). In our study, IBS-QOL had a Cronbach's alpha of 0.944.
3.3. Statistical Analysis
Data were analyzed using SPSS 26 and Excel 2023 for charting. Linear and quadratic regression models assessed conscientiousness and sub-scale effects on IBS patients' quality of life. Skewness and kurtosis assessed normality, and significance was set at the 0.05 level.
4. Results
The study comprised 232 IBS patients aged 18 to 40 (mean age 29.26 ± 6.12). Of these, 175 (75.4%) were female, 57 (24.6%) were male, 147 (63.4%) were single, and 85 (36.6%) were married.
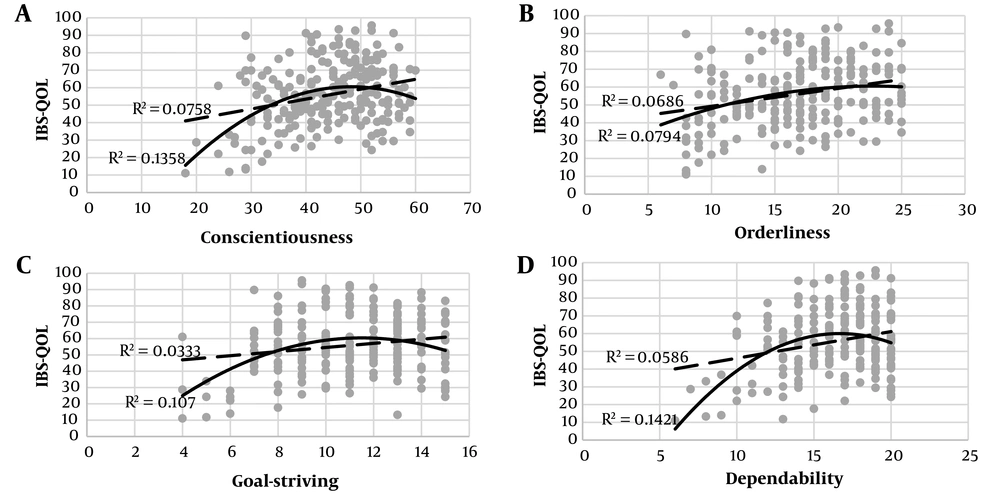
Skewness and kurtosis values within the -2 to +2 range indicate a normal variable distribution. Figure 1 shows a scatterplot predicting the quality of life in IBS patients based on conscientiousness and its subcomponents (orderliness, goal-striving, and dependability). A curvilinear (inverted U-shaped) trend was observed in the relationship between conscientiousness, goal-striving, dependability, and quality of life. No significant difference existed in the linear and curvilinear relationship between the orderliness subcomponent and quality of life in these patients.
Table 1 displays linear and curvilinear regression results for conscientiousness and its subcomponents (orderliness, goal-striving, and dependability) with quality-of-life in IBS patients. All coefficients were statistically significant at the 5% level, except for the second-degree coefficient related to the orderliness subcomponent and quality of life.
| Variables | Linear Regression (β) | Quadratic Regression (β1) | Quadratic Regression (β2) |
|---|---|---|---|
| Conscientiousness | 0.275*** | 2.304*** | -2.043*** |
| Orderliness | 0.262*** | 0.922* | -0.668 |
| Goal-striving | 0.182** | 2.090*** | -1.927*** |
| Dependability | 0.242*** | 2.537*** | -2.313*** |
a * P < 0.05, ** P < 0.01, *** P < 0.001
5. Discussion
The study uncovered an inverted U-shaped relationship between conscientiousness and its subcomponents (goal-striving and dependability) and IBS patients' quality of life. Orderliness showed a linear correlation. Contrary to conventional research, which generally examines a linear and positive relationship between conscientiousness and health outcomes (5), our results align with Carter et al.'s curvilinear finding on conscientiousness and well-being (7). The difference could be attributed to study populations, tools, and assessment methods (linear vs. curvilinear).
Conscientiousness is associated with improved health (5). Nonetheless, excessive conscientiousness may be associated with obsessive-compulsive personality disorder (7), marked by symptoms like mental fatigue (17). Notably, mental fatigue is a common extraintestinal symptom in IBS, impacting patients' quality of life (18).
Goal-striving, including self-control and effortful control (9), links positively to health in various studies (5). However, excessive levels risk adverse outcomes. Based on the process model of depletion, prolonged self-control efforts can lead to fatigue. In a maladaptive state, individuals may struggle to prioritize goals and expend excessive effort on limited rewards (19). Heightened goal-striving may relate to workaholism, reduced leisure, and subsequent mental and physical fatigue (8), impacting the quality of life in IBS patients (18). Dependability, involving responsibility and reliability, is health-promoting in chronic conditions like IBS (20). Yet, excessive responsibility can lead to perfectionism (7), negatively affecting IBS patients' quality of life (10).
Limitations include a cross-sectional design and hindering time-related assessments. Descriptive data prevents causal claims. Suggested are longitudinal conscientiousness studies and clinical trials.
5.1. Conclusions
The study found an inverted U-shaped link between conscientiousness and its subcomponents (goal-striving and dependability) and IBS patients' quality of life. Therefore, exceptionally high levels of conscientiousness also require clinical attention from healthcare professionals.