1. Background
Posttraumatic stress (PTS) is a prevalent and debilitating psychological condition triggered by experiencing or witnessing a distressing event (1). It leads to persistent symptoms like flashbacks, nightmares, irritability, avoidance, detachment, as well as cognitive and mood disturbances (2), significantly impairing normal functioning across various life domains.
The consequences of PTS extend to health and well-being, elevating the likelihood of other physical and mental health issues, including depression, anxiety, substance abuse, and suicide (3). This underscores the importance of studying PTS and its determinants.
However, exposure to traumatic events does not universally result in PTS (4). The individual's subjective perception of the event primarily defines trauma, rather than the event's objective nature (5). Trauma is inherently personal, influenced by factors such as the event's characteristics, the individual's history, personality traits, coping mechanisms, and available social support (6, 7). Consequently, what constitutes a traumatic experience can vary greatly among individuals, with a single event potentially impacting people differently, or diverse events eliciting varying trauma responses (8). Thus, assessing PTS necessitates a focus on the individual's subjective trauma experience over the event's objective details (9).
Individuals aged 15 to 29 represent 20% of Iran's population (10). Official data highlight road accidents, suicide, and violence as leading causes of mortality among this demographic (11). Furthermore, the unemployment rate among Iranian youth stands at approximately 27% (12), signaling a bleak outlook for the future. Such conditions may escalate the incidence of traumatic events and the susceptibility to PTS among the youth (13).
In Iran, PTS is a widespread and severe mental health issue, notably among young individuals who have endured war, natural disasters, terrorism, and social turmoil (14). A meta-analysis suggests that the prevalence of posttraumatic stress disorder (PTSD) in Iran is about 21.35%, surpassing the global average of 15.38% (15). Consequently, addressing PTS in young individuals and devising preventative and therapeutic strategies is imperative.
Accurate diagnosis and evaluation are crucial for the effective treatment and prevention of PTS. Such assessments allow individuals to understand their symptoms, the contributing factors to the disorder, and identify appropriate treatment approaches (16).
Various evaluation methods, including interviews, observations, psychological tests, and questionnaires, are employed to assess PTS. Due to their ease of use, quick administration, cost-effectiveness, and suitability for statistical analysis, questionnaires are often preferred (17, 18). Numerous questionnaires have been developed to measure PTS, each with specific advantages and disadvantages. Among these are the Posttraumatic Stress Symptom Scale-Self Report (PSS-SR), Posttraumatic Stress Symptom Scale-5 (PSS-5), Impact of Event Scale (IES) (19), Impact of Event Scale-22 (IES-22) (20), and Impact of Event Scale-15 (IES-15) (21).
Most current questionnaires exhibit limited sensitivity and specificity, failing to comprehensively capture the complexities and nuances of PTS symptoms (22). The challenges in designing and utilizing these instruments stem from technological and cultural shifts, evolutions in the definitions and classifications of PTS, as well as cultural and linguistic variances (22). Consequently, to ensure effectiveness across diverse populations, these questionnaires require cultural and linguistic adjustments.
In light of the limitations associated with existing tools, there is a pressing need to validate a new questionnaire tailored to assess PTS among Iranian youth. The most recent instrument in this domain is the Post-Traumatic Symptom Scale (PTSS) introduced by Nedelcea et al. (23). This scale utilizes natural language reflective of the vernacular employed by individuals to articulate their mental experiences of PTS, as observed by experienced clinicians (23). Notably, this scale demonstrates superior psychometric characteristics and aligns with the latest, more refined models of PTS (23). Thus, the purpose of this study was to explore the psychometric properties of the Persian version of the PTSS within a cohort of Iranian youth.
2. Objectives
The primary goal of this research was to delineate the factor structure and validate the PTSS for assessing PTSD among the youth in Bandar Abbas in 2022.
3. Methods
This descriptive research focused on the validation of the PTSS for Adolescents (PTSS-A), as developed by Nedelcea et al. (23).
3.1. Translation
Permission was obtained from the original authors to translate the questionnaire. Utilizing the forward-backward method, the questionnaire was translated into Persian by two proficient English translators, then back-translated to English. The final version of the questionnaire was established following consensus between the translators (24).
3.2. Participants and Procedure
This study was conducted to evaluate the PTSs among all adolescents aged 15 to 29 in Bandar Abbas city in 2022. For concurrent validity, 100 adolescents were selected as sample group A [minimum required sample size of 60 (25)], and the PTSs and MSPSS questionnaires were completed. For exploratory factor analysis (EFA), 450 more people were selected as sample group B [minimum required sample 250 (26)], and only the PTS was completed. For confirmatory factor analysis (CFA), 300 additional people were included in sample group C [minimum required sample size of 200 (27)], and only the PTS questionnaire was completed. For internal reliability and stability of the questionnaire, 100 additional people were selected as sample group D, and the questionnaire was completed two times with a four-week interval [minimum required sample 40 (28)]. In total, 950 people were considered samples for the study. Sampling was performed via the random cluster method. For this purpose, two urban areas out of four urban areas in Bandar Abbas were randomly selected. Then, four streets were randomly selected from each of these areas. Then, each street was assigned to one of the sampling groups. The researcher subsequently visited each street and prepared the necessary samples based on systematic sampling. The samples for EFA and CFA were from the same population, but they were independent of each other.
Systematic sampling was used as the sample for concurrent validity as follows. For concurrent validity, two streets, Sadeghieh and Daneshmand, were sampled (50 people for each street). On Sadeghieh Street, 1650 households lived, which resulted in 33 households by dividing this number by 50. Using the RANDBETWEEN function in Excel, we obtained a random number between 1 and 33, which was 23. Therefore, residential house number 23 at the beginning of the street was selected as the origin, the next residential house was selected by adding 33 to 23, and the next residential house was also selected by adding 33 to the previous house number. This process continued until 50 houses were selected where adolescents aged 15 to 29 lived. The remaining 50 people were also selected from Daneshmand Street in a similar way.
3.3. Measures
3.3.1. Post-Traumatic Symptom Scale
The PTSS is a 20-item self-report measure that assesses PTSD symptoms according to DSM-5 criteria. Each item is rated on a 5-point Likert Scale from 1 (never) to 5 (always), indicating the frequency of symptoms experienced over the past month. The total score ranges from 20 to 100, with higher scores suggesting more severe PTSD symptoms. The PTSS include four subscales that align with the DSM-5 symptom clusters: Intrusion (items 1 - 4), avoidance (items 5 - 8), negative alterations in cognitions and mood (items 9 - 13), and arousal and reactivity (items 14 - 20). The PTSS demonstrate excellent psychometric qualities, including high internal consistency (alpha = 0.96), robust temporal reliability (r = 0.85), strong convergent validity (r = 0.92 with the PCL-5 and r = 0.89 with the IES-R), and moderate discriminant validity (r = 0.67 with depression, r = 0.64 with anxiety, and r = 0.62 with stress) (23). The PTSS were translated into Persian using the forward-backwards method, and this study confirmed their psychometric properties. The Persian version of the PTSS showed high internal consistency (alpha = 0.94), good temporal stability (r = 0.87), and strong convergent validity (r = 0.91 with the Mississippi Scale for Posttraumatic Stress Disorder (MSPSS)).
3.3.2. Mississippi Scale for Posttraumatic Stress Disorder
The MSPSS is a 35-item self-report instrument designed to measure PTSD symptoms across five categories: Reexperiencing, avoidance and numbing, hyperarousal, and self-harm. Respondents rate each item on a 5-point scale ranging from 1 (false) to 5 (completely true), leading to a total score between 35 and 175, where scores above 107 suggest the presence of PTSD. Eight items require reverse scoring. The MSPSS demonstrates high internal consistency (alpha = 0.94), test-retest reliability (r = 0.97), convergent validity (r = 0.86 with the CAPS and r = 0.85 with the SCID), and discriminant validity (r = 0.68 with depression, r = 0.66 with anxiety, and r = 0.65 with general distress) (27-29). Validated by Goodarzi, the Persian version of the MSPSS showed high internal consistency (alpha = 0.92), test-retest reliability (r = 0.91), and convergent validity (r = 0.87 with the IES-R) (29). In this study, the PTSS exhibited high internal consistency, with a Cronbach's alpha coefficient of 0.91.
3.3.3. Cut-off Point Selection
For selecting the cut-off point, the receiver operating characteristic (ROC) curve method was employed. The research questionnaire alongside the MSPSS served as the test and criterion measures, respectively. The ROC curve was plotted by adjusting the research questionnaire's cut-off score from 20 to 100 in increments of 10, calculating the true positive rate (TPR), false positive rate (FPR), true negative rate (TNR), false negative rate (FNR), and Youden Index for each cut-off score. True positive rate is the proportion of true positives out of the total positive cases, defined as TPR = TP / (TP + FN). False positive rate is the proportion of false positives out of the total negative cases, defined as FPR = FP / (FP + TN). The Youden Index, calculated as the difference between TPR and FPR (Youden Index = TPR - FPR), served as the criterion to determine the optimal cut-off point for maximizing the test's accuracy (30).
3.4. Statistical Analysis
For the evaluation of the questionnaire, both validity and reliability were assessed through various methods. Face validity was examined using both qualitative and quantitative approaches. In the qualitative phase, interviews with 10 members of the target group were conducted to assess the clarity and appropriateness of the questionnaire items, allowing for necessary modifications based on their feedback. The quantitative phase employed a five-point Likert Scale to ascertain the face validity quantitatively, with items scoring below 1.5 on the impact score being revised or excluded (31). Content validity was evaluated by consulting 10 experts, utilizing both the content validity ratio (CVR) and the Content Validity Index (CVI). A CVR exceeding 0.62 and a CVI above 0.79 were deemed satisfactory (32). Concurrent validity was established through correlation analysis between the PTSS and the MSPSS. Exploratory factor analysis (EFA), employing the principal factor extraction method and varimax rotation, was conducted to explore the questionnaire's structure, with the Kaiser–Meyer–Olkin (KMO) measure surpassing 0.7 and Bartlett's test of sphericity achieving significance at P < 0.05 indicating suitability for factor analysis (33).
Confirmatory factor analysis was applied to ascertain the model's fit, utilizing indices such as the standardized root mean square residual (SRMR), Goodness of Fit Index (GFI), Comparative Fit Index (CFI), adjusted Goodness of Fit Index (AGFI), root mean square error of approximation (RMSEA), and the ratio of chi-square to degrees of freedom (CMIN/DF) (34). Internal consistency was evidenced by a Cronbach's alpha coefficient greater than 0.7 (35). Temporal stability (test-retest reliability) and internal reliability (split-half method) were also evaluated. Descriptive statistics, along with SPSS 21 for basic analyses and LISREL 8.80 for CFA, were employed in data processing, with the threshold for statistical significance set at P < 0.05.
4. Results
The predominant age group among participants was 25 to 29 years (51.6%), followed by 20 to 24 years (34.2%), and 15 to 19 years (14.2%). Regarding educational attainment, 59.93% were students, 16.54% had a diploma or lower education, and 23.53% possessed a university degree. The distribution of participants by occupation revealed that 45.7% were university students, 14.2% were school pupils, 18.4% were unemployed, and 21.6% were employed. The gender distribution was nearly balanced, with 50.3% male and 49.7% female participants. The majority were unmarried (79%), with the remainder being married (21%) (Table 1).
| Total (n = 901) | Concurrent Validity (n = 95) | EFA (n = 427) | CFA (n = 285) | Reliability (n = 94) | |
|---|---|---|---|---|---|
| Age, y | |||||
| 15 to 19 | 128 (14.2) | 14 (14.7) | 68 (15.9) | 34 (11.9) | 12 (12.8) |
| 20 to 24 | 308 (34.2) | 34 (35.8) | 138 (32.3) | 102 (35.8) | 34 (36.2) |
| 25 to 29 | 465 (51.6) | 47 (49.5) | 221 (51.8) | 149 (52.3) | 48 (51.1) |
| Education | |||||
| Student | 128 (14.21) | 14 (14.74) | 68 (15.92) | 34 (11.93) | 12 (12.77) |
| Diploma and less | 149 (16.54) | 25 (26.32) | 89 (20.84) | 92 (32.28) | 27 (28.72) |
| Student | 412 (45.73) | 40 (42.11) | 196 (45.90) | 130 (45.61) | 46 (48.94) |
| University | 212 (23.53) | 16 (16.84) | 74 (17.33) | 29 (10.18) | 9 (9.57) |
| Employment status | |||||
| Pupil | 128 (14.2) | 14 (14.7) | 68 (15.9) | 34 (11.9) | 12 (12.8) |
| University student | 412 (45.7) | 40 (42.1) | 196 (45.9) | 130 (45.6) | 46 (48.9) |
| Unemployed | 166 (18.4) | 19 (20.0) | 79 (18.5) | 55 (19.3) | 13 (13.8) |
| Employed | 195 (21.6) | 22 (23.2) | 84 (19.7) | 66 (23.2) | 23 (24.5) |
| Gender | |||||
| Male | 453 (50.3) | 51 (53.7) | 217 (50.8) | 134 (47.0) | 51 (54.3) |
| Female | 448 (49.7) | 44 (46.3) | 210 (49.2) | 151 (53.0) | 43 (45.7) |
| Marital status | |||||
| Married | 189 (21.0) | 21 (22.1) | 96 (22.5) | 58 (20.4) | 14 (14.9) |
| Single | 712 (79.0) | 74 (77.9) | 331 (77.5) | 227 (79.6) | 80 (85.1) |
a Values are expressed as No. (%).
4.1. Face Validity
The impact scores for all questionnaire items varied between 1.6 and 3.6, all exceeding the 1.5 threshold, affirming the questions' satisfactory face validity (Table 2).
| Items | Factor | Impact Factor | CVI | CVR | |||
|---|---|---|---|---|---|---|---|
| Arousal and Reactivity | Negative Alterations in Cognitions and Mood | Avoidance | Intrusion | ||||
| i1 | 0.19 | 0.21 | 0.20 | 0.65 | 3.50 | 0.84 | 0.85 |
| i2 | 0.19 | 0.21 | 0.19 | 0.71 | 2.00 | 0.82 | 0.86 |
| i3 | 0.18 | 0.20 | 0.18 | 0.66 | 2.90 | 0.84 | 0.86 |
| i4 | 0.17 | 0.19 | 0.18 | 0.65 | 3.20 | 0.91 | 0.93 |
| i5 | 0.16 | 0.18 | 0.68 | 0.17 | 3.60 | 0.84 | 0.88 |
| i6 | 0.17 | 0.18 | 0.68 | 0.18 | 2.00 | 0.80 | 0.84 |
| i7 | 0.16 | 0.17 | 0.67 | 0.17 | 2.70 | 0.94 | 0.97 |
| i8 | 0.17 | 0.19 | 0.70 | 0.19 | 3.60 | 0.81 | 0.83 |
| i9 | 0.14 | 0.71 | 0.14 | 0.15 | 2.20 | 0.92 | 0.96 |
| i10 | 0.14 | 0.70 | 0.17 | 0.18 | 3.20 | 0.94 | 0.96 |
| i11 | 0.14 | 0.66 | 0.16 | 0.16 | 3.20 | 0.85 | 0.86 |
| i12 | 0.14 | 0.68 | 0.16 | 0.16 | 2.50 | 0.91 | 0.93 |
| i13 | 0.15 | 0.74 | 0.16 | 0.18 | 1.90 | 0.82 | 0.83 |
| i14 | 0.74 | 0.13 | 0.12 | 0.14 | 2.20 | 0.85 | 0.88 |
| i15 | 0.71 | 0.13 | 0.13 | 0.13 | 2.80 | 0.91 | 0.95 |
| i16 | 0.74 | 0.12 | 0.13 | 0.13 | 3.60 | 0.80 | 0.84 |
| i17 | 0.69 | 0.13 | 0.13 | 0.14 | 1.60 | 0.75 | 0.77 |
| i18 | 0.71 | 0.12 | 0.13 | 0.14 | 2.90 | 0.81 | 0.83 |
| i19 | 0.74 | 0.13 | 0.13 | 0.14 | 3.20 | 0.79 | 0.83 |
| i20 | 0.72 | 0.12 | 0.12 | 0.13 | 2.70 | 0.90 | 0.93 |
4.2. Content Validity
Content validity ratios for all items were above 0.75, and CVIs exceeded 0.77, surpassing the set benchmarks for content validity.
4.3. Concurrent Validity
A positive and significant correlation was found between the total scores of the PTSS and the MSPSS, at r = 0.64, P < 0.001. Similarly, each dimension of the PTSS —including intrusion, avoidance, negative alterations in cognitions and mood, and arousal and reactivity—showed a positive and significant correlation with the total MSPSS scores, ranging from r = 0.49 to r = 0.71, all significant at P < 0.001.
4.4. Exploratory Factor Analysis (EFA)
The Kaiser-Meyer-Olkin (KMO) measure stood at 0.913, and Bartlett's test confirmed suitability for factor analysis (chi-square = 4234.053, df = 190, P < 0.001). Using the principal axis factor extraction method with varimax rotation, four factors were identified, accounting for 56.288% of the variance. These factors included: Arousal and reactivity (questions 14 - 20), explaining 19.93% of variance; negative alterations in cognitions and mood (questions 9 - 13), accounting for 14.30% of variance; avoidance (questions 5 - 8), explaining 11.18% of variance; and intrusion (questions 1 - 4), contributing to 10.87% of the variance (Table 2).
4.5. Confirmatory Factor Analysis
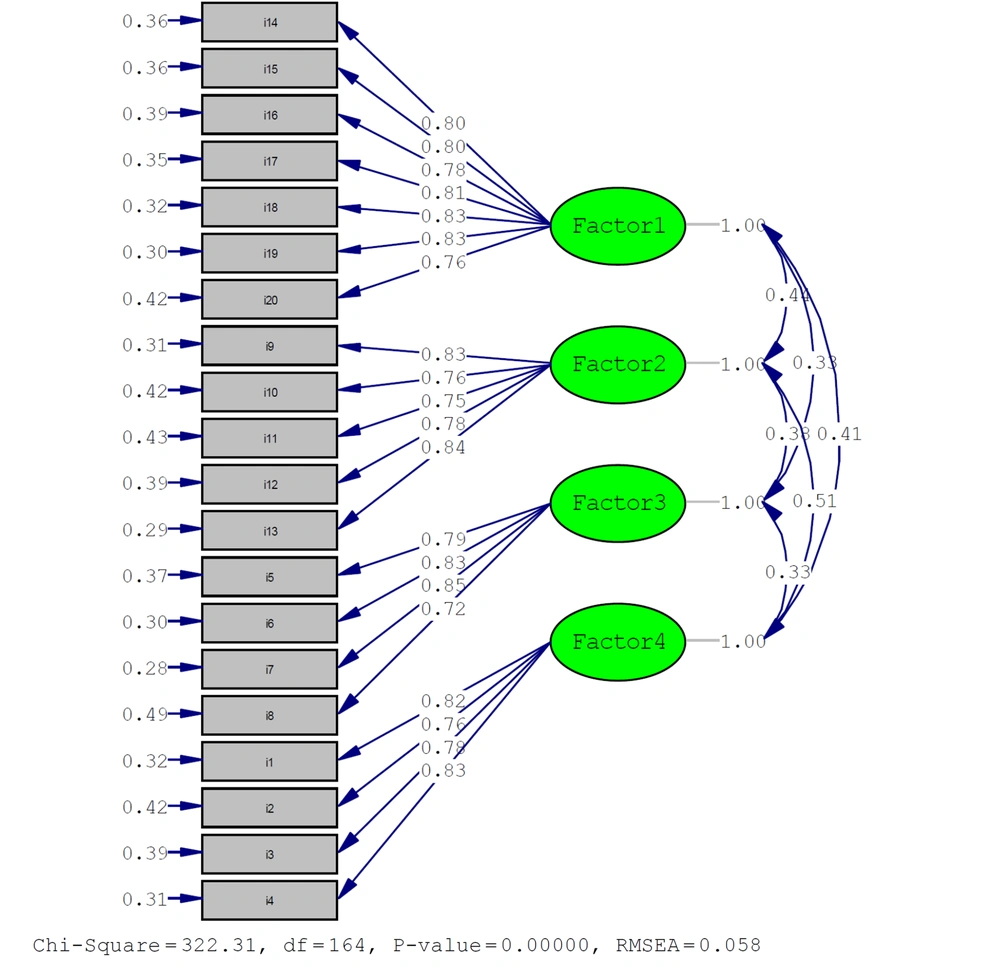
The results from the CFA demonstrated that the four-factor model exhibited a superior fit to the data compared to a seven-factor model, as indicated by various goodness-of-fit metrics: Standardized root mean square residual (SRMR) = 0.028 (below the 0.10 threshold), root mean square error of approximation (RMSEA) = 0.058 (below the 0.08 threshold), CFI = 0.98 (exceeding 0.90), Normed Fit Index (NFI) = 0.96 (exceeding 0.90), Goodness of Fit Index (GFI) = 0.90 (meeting the 0.90 benchmark), Adjusted Goodness of Fit Index (AGFI) = 0.87 (above the 0.80 standard), and the ratio of chi-square to degrees of freedom (CMIN/DF) = 1.98 (under 3) (27). Figure 1 further illustrates the model's fit with the data, underscoring the strong support for the four-factor model.
4.6. Reliability
In terms of reliability, the Cronbach's alpha coefficient for the entire scale was 0.87, and for the subscales—arousal and reactivity, negative alterations in cognitions and mood, avoidance, and intrusion—the coefficients were 0.88, 0.83, 0.82, and 0.77, respectively. All items showed positive and significant correlations with the scale score, ranging from 0.346 to 0.595 (P < 0.01). The split-half reliability scores were 0.81 for the first half (10 items) and 0.83 for the second half (10 items) of the questionnaire, with a correlation of 0.78 between them (P < 0.01). The test-retest reliability was found to be 0.81 (P < 0.01).
4.7. Cut-off Point
For the cut-off point, the highest Youden Index was achieved at a cut-off score of 60, which corresponded to a TPR of 70% and a FPR of 1.18%. This indicates that using a cut-off score of 60 for the PTSS could accurately identify 70% of individuals with PTSD while only misclassifying 1.18% of those without PTSD. Consequently, the optimal cut-off point for the PTSS was established at 60, based on the Youden Index criterion (Table 3).
| Cut-off Point | TP (True Positive) | FN (False Negative) | FP (False Positive) | TN (True Negative) | TPR (True Positive Rate), % | FPR (False Positive Rate), % | Youden Index |
|---|---|---|---|---|---|---|---|
| 20 | 8 | 0 | 87 | 0 | 8.42 | 0.00 | 0.08 |
| 30 | 8 | 0 | 87 | 0 | 8.42 | 0.00 | 0.08 |
| 40 | 8 | 0 | 82 | 5 | 8.89 | 0.00 | 0.09 |
| 50 | 8 | 0 | 36 | 51 | 18.18 | 0.00 | 0.18 |
| 60 | 7 | 1 | 1 | 86 | 70.00 | 1.18 | 0.69 |
| 70 | 0 | 8 | 0 | 87 | 0.00 | 8.42 | -0.08 |
| 80 | 0 | 8 | 0 | 87 | 0.00 | 8.42 | -0.08 |
| 90 | 0 | 8 | 0 | 87 | 0.00 | 8.42 | -0.08 |
| 100 | 0 | 8 | 0 | 87 | 0.00 | 8.42 | -0.08 |
5. Discussion
This study validated the Post-Traumatic Symptom (PTS) questionnaire, developed by Nedelcea et al. (23), for assessing posttraumatic stress symptoms within a young Iranian demographic. The validation process employed assessments of face validity, content validity, concurrent validity, and construct validity through exploratory and CFA.
Face validity results indicated that all items had impact factors exceeding 1.5, affirming the questionnaire's acceptable face validity. The PTS questionnaire was found to be straightforward, fluent, and relevant for identifying research problems, gaining acceptance from the sample population. These findings align with those reported by the original author (23).
Content validity outcomes revealed that all items possessed CVRs above 0.75 and CVIs above 0.77, surpassing the minimum criteria for content validity. This suggests the scale's adequacy in measuring posttraumatic stress disorder among young individuals, providing a comprehensive and inclusive assessment tool that resonates with the young Iranian populace's experiences. These observations are consistent with those made by the original author (23).
Concurrent validity testing demonstrated a positive and significant correlation between the total scores of the PTS questionnaire and the MSPSS. This consistency with the original author's findings (23) signifies the PTS questionnaire's suitable concurrent validity for evaluating posttraumatic stress disorder in young individuals, marking it as a reliable measure aligned with other validated tools in this domain.
Exploratory factor analysis delineated four principal factors—arousal and reactivity, negative alterations in cognitions and mood, avoidance, and intrusion—while CFA reinforced this four-factor model. These outcomes not only echo the findings from Nedelcea et al.'s (23) study but also adhere to the DSM-5 criteria for posttraumatic stress disorder (36), establishing a robust framework for the questionnaire's application within the specified demographic.
Our four-factor model aligns with the Posttraumatic Stress Disorder Checklist (PCL) (37) and the Mississippi Scale for Combat-Related PTSD (MCCP) (38), which similarly categorize PTSD into four dimensions (39). This correspondence, however, diverges from the PTSD Checklist for DSM-5 (PCL-5) (40) and the Impact of Event Scale-Revised (IES-R) (34), which include a fifth dimension addressing negative alterations in cognitions and mood or hyperarousal. Such disparities may echo the evolution of PTSD diagnostic criteria from DSM-IV to DSM-5 or variations in the nature and severity of traumatic experiences targeted by these questionnaires (41). Consequently, our questionnaire might offer a more tailored assessment framework for PTSD among Iranian individuals exposed to traumatic events like war, violence, or natural disasters (42).
Nonetheless, the factor structure for the PTSs does not receive uniform support across studies. A meta-analysis exploring pre-trauma risk factors and PTSD symptoms after subsequent trauma exposure highlighted varying findings, with some studies endorsing a four-factor model while others suggested a five-factor arrangement (43). Another investigation into the link between childhood posttraumatic stress and borderline personality disorder also delivered results diverging from our study's four-factor model (44).
The PTSs demonstrated robust psychometric properties, including high Cronbach's alpha coefficients, solid split-half correlations, and reliable test-retest results. Each item also showed positive and significant correlations with the overall scale score, mirroring findings from the original author's work (23). This consistency underlines the PTS as a reliable and valid instrument for evaluating posttraumatic stress symptoms in young Iranian individuals.
The cut-off score of 60 yielded the highest Youden Index (0.69), signifying optimal test accuracy. With a high TPR (70.00%) and a low FPR (1.18%), this threshold effectively distinguishes most participants with PTSD while minimizing misclassification of those without the condition.
This study's strengths include the first-time validation of the PTS questionnaire in Iran, adapting the questionnaire through back-translation for linguistic and cultural appropriateness, employing various validity and reliability assessments, and utilizing both exploratory and CFA to verify the questionnaire's four-factor structure.
However, the study faces limitations, notably the focus on young individuals from Bandar Abbas, which challenges the extrapolation of findings nationwide. The cross-sectional research design also precludes causal inferences. Moreover, relying on self-reported questionnaires might compromise the accuracy of participants' responses.
Given the outcomes and constraints identified in this study, future research should involve broader participant groups to enrich understanding of posttraumatic stress among young Iranians. Employing various research methodologies, such as experimental approaches, can enhance study robustness. Moreover, digitalizing the PTS questionnaire could bolster accessibility, efficiency, and data collection cost-effectiveness. Incorporating advanced technologies, like artificial intelligence and chatbots, could enable interactive responses, potentially increasing user engagement.
5.1. Conclusions
In conclusion, this investigation has affirmed the PTS as a viable tool for assessing posttraumatic stress symptoms in Iranian youth, demonstrating satisfactory validity, reliability, and a four-factor structure that aligns with the initial research and DSM-5 standards. While the PTS questionnaire proves to be straightforward and effective, its applicability is somewhat limited by the specific sample size and geographic focus of the study. Future research with larger and more varied cohorts is essential to further validate the instrument's psychometric characteristics. Adopting online and electronic modalities, along with cutting-edge technologies, may enhance the questionnaire's accessibility and appeal.