1. Background
There is a lack of deep knowledge and consensus regarding the functional problems of children with cerebral palsy (CP), a group characterized by permanent brain abnormalities primarily affecting mobility and posture, among rehabilitation professionals (1, 2). The International Classification of Functioning, Disability and Health (ICF) and its Children and Youth version (ICF-CY), which adopt a bio-psychosocial model, offer a comprehensive framework to understand and address human functioning and related phenomena. This model encompasses four components: body functions and structures, activities and participation, personal factors, and environmental factors (3, 4). Consequently, the ICF is a valuable tool for systematically addressing the various aspects of functional abilities and challenges of children with CP in daily activities (4). However, some studies have noted that clinical practices of Occupational Therapists (OTs) often focus more on body functions and structures than on environmental and contextual factors when treating these children (2, 5). Yet, environmental and contextual factors significantly influence their functioning, including social and school participation (6, 7). These findings underscore the potential utility of the ICF-CY (hereafter referred to simply as ‘ICF’ in this article) in the clinical practices of OTs for these children. To enhance the application of the ICF in clinical settings, a concise list of ICF categories called the ICF core set (ICF-CS) has been developed for children aged 0 - 18 with CP (8). This ICF-CS includes a Comprehensive version and three age-based Brief versions for the age groups 0 - 6, 6 - 14, and 14 - 18 years (8). The brief ICF-CSs consist of essential categories that should be considered in clinical settings requiring brief assessments to address the functioning and related environmental challenges of these children, while the comprehensive set serves as a framework for use in interdisciplinary teamwork (8, 9).
The validation studies of the ICF core sets (ICF-CS) have been particularly emphasized in low- and middle-income countries (10, 11). In our previous study, the content validity of the comprehensive version of this ICF-CS was evaluated for 6 - 12-year-old children with CP from the perspective of Iranian occupational therapists (OTs), resulting in the confirmation of 119 categories. However, it remains unclear which ICF categories should be minimally addressed in clinical settings when only a brief assessment is feasible for such children.
Extensive research indicates that the level of functional limitation in children with CP significantly influences their participation in various situations and the corresponding environmental challenges they face (6, 12-15). Children with CP typically experience functional limitations in gross motor (GM), fine motor (FM), eating and drinking (E&D), communication function (CF), and visual function (VF) due to CP or its secondary consequences (16-19). Literature suggests that the dependency of children with CP on assistance, assistive devices, and/or modifications in activity and environment for these functions exposes them to substantial functional and environmental challenges (20, 21).
These findings collectively indicate that creating brief ICF category sets based on the significant functional limitations of children with CP in GM, FM, E&D, CF, and VF could define the most relevant categories that should be minimally considered in clinical brief assessments to address their functioning and related environmental challenges. However, such brief sets have not yet been developed for these children.
2. Objectives
This study aimed to develop and validate the content of five ICF brief sets for 6 - 12-year-old children with CP based on their significant limitations in GM, FM, E&D, CF, and VF, from the perspective of Iranian OTs.
3. Methods
3.1. Study Design
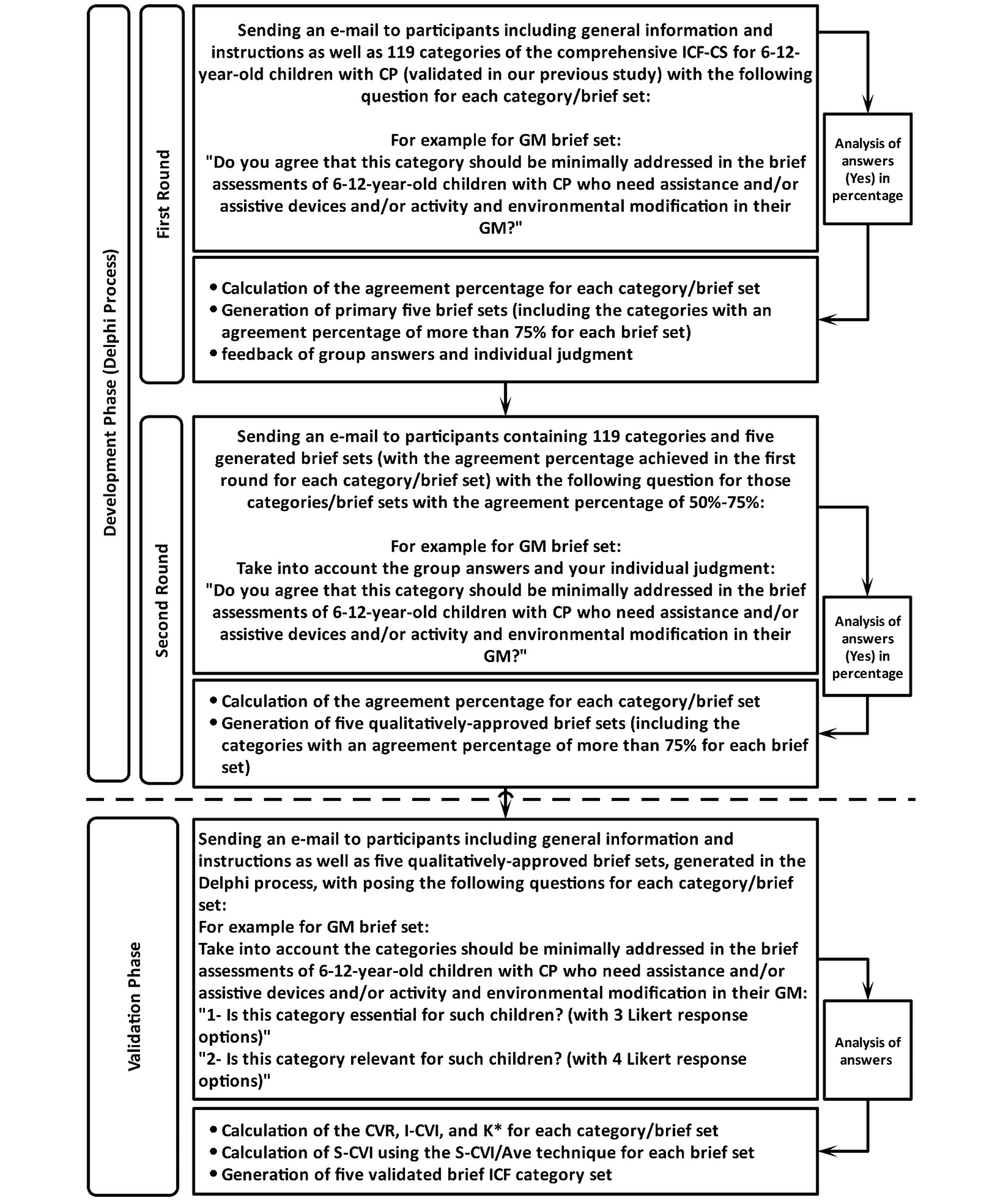
This cross-sectional, multi-method study was conducted in two phases. The first phase involved developing brief sets through a Delphi process among Iranian OTs experienced in CP and the ICF. The second phase focused on content validation of the brief sets, where the content validity ratio (CVR), content validity index (CVI), modified Kappa (K*), and Scale-CVI (S-CVI) were calculated through an electronic survey with an expert panel of Iranian OTs.
3.2. Participants
To recruit Iranian OTs expert in CP and ICF, a combination of literature search, personal recommendations, and contact with the Iranian Occupational Therapy Association (IROTA) was employed. From the initially identified OTs across the country, 23 who met the inclusion criteria were purposively selected for the Delphi process. The inclusion criteria specified at least five years of experience in CP treatment and familiarity with ICF, as detailed in the invitation letter. Nineteen OTs agreed to participate in the Delphi process. For the second phase, the inclusion criteria for the expert panel required a minimum of ten years of educational and research experience in CP and ICF. Potential participants were further identified through a literature search and referrals from initially identified participants, employing a snowball sampling method. Thirteen OTs were identified, and 10 agreed to participate in the expert panel upon receiving the invitation letter.
3.3. Development Phase (Generation of the Brief ICF Category Sets)
A Delphi process involving two rounds of electronic mail surveys was utilized to generate the brief sets. Initially, for the first round of the Delphi, participants were provided with general information, a demographic questionnaire, and an Excel file containing 119 categories identified in our previous study as the comprehensive ICF-CS for 6 - 12-year-old children with CP. Participants were requested to evaluate each of the 119 categories by answering five targeted questions for each category, applicable to GM, FM, E&D, CF, and VF. For example, for GM, the question was: "Do you agree that this category should be minimally addressed in the brief assessments of 6 - 12-year-old children with CP who require assistance and/or assistive devices and/or activity and environmental modifications in their GM?" Additionally, participants were asked to provide information based on their professional experience and demographic data. A two-week deadline was set for the completion and return of the questionnaire in each Delphi round. Reminder emails were sent one week before and one week after the deadline. Responses were collected and a descriptive analysis was performed to determine the percentage of participants who answered “Yes” for each category/brief set.
In the second round, an Excel file containing the 119 categories, along with the percentage of group answers for each category/brief set from the first round, was sent to participants. They were asked to consider the group responses and their own judgments before re-answering the same question for those categories/brief sets that achieved an agreement percentage of 50 - 75% in the first round. Descriptive analysis was again conducted after collecting the responses.
3.4. Validation Phase
During the validation phase, participants received general information, a demographic questionnaire, and an Excel file containing the categories generated for each of the brief sets from the Delphi process via email. The experts were tasked with rating the essentiality and relevancy of each category for each brief set using a 3-point Likert scale ("Essential," "Useful, but not essential," or "Not necessary") and a 4-point Likert scale (ranging from 1 [not relevant or not representative] to 4 [extremely relevant or representative]), respectively. Participants were given a two-week deadline to complete and return the questionnaire, with reminders sent one week before and two days after the deadline. The CVR, CVI, K*, and Scale-CVI (S-CVI) were calculated once responses were collected. Figure 1 provides an overview of the development and validation processes for the brief sets.
3.5. Data Analysis
3.5.1. Development Phase (Delphi Process)
To assess the participants’ characteristics and calculate the frequencies of answers in the Delphi rounds, descriptive statistics were conducted using SPSS software version 16.0 (IBM Corporation, USA). In each Delphi round, the percentage of participants who answered “Yes” to the question for each category/brief set was determined. It has been established that an agreement percentage of at least 75% among participants is considered sufficiently high (22, 23). Consequently, for each brief set, categories that achieved at least 75% agreement from participants in the Delphi process were included.
3.6. Validation Phase
For each category/brief set, the CVR was calculated. To ensure that the agreement among experts was not due to chance, the minimum required CVR for each category/brief set was set at 0.62 (one-tailed test, α = 0.05) given the total number of experts (24). Additionally, the CVI for each category/brief set (Item-level CVI or I-CVI) and for each of the brief sets (scale-level CVI or S-CVI) were calculated. An I-CVI of at least 0.78 was accepted, adhering to Lynn’s proposed guidelines (25). To adjust the I-CVIs for chance agreement, the K* was calculated for each category/brief set using the formula: K* = (I-CVI - Pc) / (1 - Pc), where Pc (Probability of chance) = N! / (A! * ((N-A)!) * 0.5N, and N is the number of experts, and A is the number of experts agreeing on good relevance. Although the values of K* and I-CVI become closer as the number of experts increases, K* values of 0.74 or higher for each category/brief set were accepted, as these values are considered to fall within the range deemed excellent (26).
The S-CVI for each brief set was calculated using the S-CVI/Ave technique. An S-CVI/Ave of 0.90 or higher is considered to indicate excellent content validity (27).
3.7. Ethics
The study protocol was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences in October 2021 (IR.USWR.REC.1400.164). Children were not directly involved in this study. All participants were informed about the study objectives, and informed consent was obtained from each participant. All procedures adhered to the ethical standards of the Regional Research Committee and were in accordance with the Declaration of Helsinki of 1964 and its later amendments.
4. Results
4.1. Participants
Out of 23 identified OTs from across the country, three declined to participate in the Delphi process and one did not return the questionnaires despite two reminders. Consequently, 19 OTs participated in the first round of the Delphi process, resulting in a dropout rate of 17.40% (19/23; 82.60%). All 19 OTs also participated in the second round of the Delphi. In the validation phase, of the 13 identified experts, 10 agreed to participate in the expert panel and returned the completed questionnaires (10/13; 76.92%). Three experts declined to participate in the panel due to personal reasons. The demographic and professional characteristics of the participants are shown in Table 1.
| Study Phase | Number | Male Gender | Age (y) | Professional Experience (y) | CP Experience (y) | |
|---|---|---|---|---|---|---|
| 5 - 10 | > 10 | |||||
| Development phase (Delphi) | ||||||
| Round 1 | 19 | 10 (52.6) | 40 (28 - 56) | 18 (6 - 29) | 5 (26.3) | 14 (73.7) |
| Round 2 | 19 | 10 (52.6) | 40 (28 - 56) | 18 (6 - 29) | 5 (26.3) | 14 (73.7) |
| Validation phase (Expert panel) | ||||||
| CVR and CVI | 10 | 5 (50) | 42.5 (36 - 56) | 19.5 (10 - 29) | 1 (10) | 9 (90) |
a Values are expressed as No. (%) or median (min-max).
4.2. Development Phase
In the first round of the Delphi, participants confirmed 53, 58, 42, 68, and 54 categories respectively for the GM, FM, E&D, CF, and VF brief sets. Collectively, 205 categories/brief sets were rejected in the first round due to an agreement percentage of less than 50%. Additionally, 115 categories/brief sets that obtained an agreement percentage of 50-75% in the first round were revisited in the second round. Of these, 67 categories/brief sets were collectively confirmed in the second round, resulting in totals of 74, 69, 52, 73, and 74 categories respectively for GM, FM, E&D, CF, and VF brief sets. Therefore, 48 categories/brief sets were rejected due to their agreement percentage of less than 50% in this round. Table 2 presents the final agreement percentage for each category within each brief set obtained in the first or second round of the Delphi.
| ICF Code | Final Agreement in the Delphi Rounds (%) | |||||
|---|---|---|---|---|---|---|
| 2nd Level | 3rd Level | GM | FM | E & D | CF | VF |
| s110 | 84 a | 89 a | 84 a | 78 a | 84 a | |
| s730 | 84 a | 100 a | 100 a | 47 | 26 | |
| s750 | 100 a | 15 | 10 | 10 | 15 | |
| s760 | 94a | 84 a | 89 a | 42 | 42 | |
| s7700 | 84 a | 84 a | 78 a | 21 | 15 | |
| s7703 | 78 a | 78 a | 78 a | 21 | 47 | |
| b114 | 77 a | 47 | 47 | 94 a | 78 a | |
| b117 | 94 a | 78 a | 78 a | 100 a | 78 a | |
| b126 | 36 | 31 | 77 a | 94 a | 31 | |
| b1301 | 89 a | 89 a | 89 a | 100 a | 78 a | |
| b134 | 42 | 31 | 42 | 77 a | 47 | |
| b140 | 78 a | 89 a | 84 a | 100 a | 94 a | |
| b144 | 31 | 36 | 36 | 89 a | 94 a | |
| b1473 | 47 | 100 a | 89 a | 47 | 78 a | |
| b1474 | 78 a | 94 a | 78 a | 42 | 78 a | |
| b152 | 47 | 77 a | 77 a | 94 a | 47 | |
| b156 | 89 a | 94 a | 78 a | 100 a | 100 a | |
| b163 | 78 a | 89 a | 100 a | 100 a | 100 a | |
| b164 | 47 | 78 a | 47 | 100 a | 78 a | |
| b167 | 21 | 36 | 47 | 94 a | 36 | |
| b210 | 42 | 83 a | 47 | 78 a | 100 a | |
| b230 | 15 | 10 | 15 | 100 a | 42 | |
| b235 | 100 a | 47 | 47 | 44 | 78 a | |
| b260 | 100 a | 100 a | 78 a | 42 | 47 a | |
| b265 | 77 a | 100 a | 94 a | 77 a | 78 a | |
| b280 | 94a | 94 a | 78 a | 47 | 47 a | |
| b320 | 10 | 10 | 31 | 100 a | 21 | |
| b440 | 77 a | 26 | 100 a | 84 a | 21 | |
| b445 | 77 a | 36 | 84 a | 78 a | 15 | |
| b455 | 100 a | 94 a | 78 a | 36 | 21 | |
| b510 | 15 | 15 | 89 a | 47 | 21 | |
| b525 | 31 | 21 | 78 a | 31 | 21 | |
| b620 | 21 | 15 | 78 a | 21 | 21 | |
| b710 | 100 a | 100 a | 78 a | 21 | 10 | |
| b715 | 100 a | 100 a | 78 a | 21 | 26 | |
| b730 | 100 a | 100 a | 84 a | 26 | 15 | |
| b735 | 100 a | 100 a | 89 a | 26 | 21 | |
| b740 | 100 a | 100 a | 78 a | 31 | 21 | |
| b750 | 100 a | 94 a | 89 a | 42 | 78 a | |
| b755 | 94 a | 89 a | 84 a | 47 | 36 | |
| b760 | 100 a | 100 a | 94 a | 47 | 47 | |
| b765 | 84 a | 84 a | 94 a | 47 | 36 | |
| b770 | 100 a | 36 | 21 | 31 | 31 | |
| d110 | 26 | 36 | 47 | 84 a | 100 a | |
| d115 | 15 | 21 | 26 | 94 a | 42 | |
| d120 | 47 | 77 a | 78 a | 84 a | 77 a | |
| d130 | 47 | 94 a | 36 | 84 a | 78 a | |
| d131 | 36 | 78a | 47 | 89 a | 89 a | |
| d133 | 10 | 10 | 26 | 100 a | 47 | |
| d137 | 26 | 36 | 42 | 94 a | 78 a | |
| d140 | 21 | 31 | 26 | 84 a | 78 a | |
| d145 | 42 | 78 a | 26 | 26 | 88 a | |
| d155 | 83 a | 89 a | 77 a | 94 a | 78 a | |
| d160 | 47 | 77 a | 48 | 100 a | 89 a | |
| d161 | 77 a | 84 a | 84 a | 94 a | 89 a | |
| d166 | 21 | 31 | 26 | 89 a | 89 a | |
| d170 | 42 | 78 a | 26 | 89 a | 89 a | |
| d172 | 10 | 36 | 15 | 22 | 44 | |
| d175 | 26 | 36 | 31 | 89 a | 78 a | |
| d177 | 31 | 36 | 36 | 77 a | 44 | |
| d210 | 78 a | 84 a | 78 a | 84 a | 84 a | |
| d220 | 36 | 42 | 42 | 77 a | 47 | |
| d230 | 94 a | 94 a | 89 a | 89 a | 94 a | |
| d250 | 31 | 31 | 36 | 94 a | 38 | |
| d310 | 15 | 15 | 26 | 100 a | 44 | |
| d315 | 36 | 31 | 31 | 94 a | 94 a | |
| d330 | 21 | 21 | 36 | 100 a | 42 | |
| d335 | 31 | 47 | 42 | 100 a | 78 a | |
| d350 | 100 a | 10 | 31 | 100 a | 44 | |
| d360 | 26 | 36 | 36 | 100 a | 78 a | |
| d410 | 100 a | 78 a | 77 a | 36 | 77 a | |
| d415 | 94 a | 94 a | 78 a | 36 | 77 a | |
| d420 | 100 a | 47 | 36 | 31 | 77 a | |
| d430 | 100 a | 100 a | 42 | 36 | 47 | |
| d435 | 94 a | 21 | 15 | 26 | 77 a | |
| d440 | 47 | 100 a | 84 a | 42 | 77 a | |
| d445 | 83 a | 94 a | 84 a | 47 | 83 a | |
| d450 | 94 a | 15 | 15 | 36 | 77 a | |
| d455 | 100 a | 36 | 26 | 44 | 83 a | |
| d460 | 100 a | 26 | 21 | 47 | 78 a | |
| d465 | 89 a | 77 a | 26 | 42 | 78 a | |
| d470 | 94 a | 83 a | 31 | 84 a | 84 a | |
| d510 | 78 a | 94 a | 36 | 47 | 77 a | |
| d520 | 89 a | 100 a | 47 | 47 | 89 a | |
| d530 | 89a | 100 a | 36 | 42 | 89 a | |
| d540 | 94 a | 100 a | 36 | 36 | 100 a | |
| d550 | 77 a | 94 a | 94 a | 31 | 89 a | |
| d560 | 47 | 89 a | 94 a | 31 | 94 a | |
| d570 | 78 a | 84 a | 47 | 47 | 89 a | |
| d710 | 21 | 21 | 26 | 100 a | 78 a | |
| d750 | 26 | 21 | 15 | 89 a | 47 | |
| d760 | 21 | 21 | 21 | 100 a | 36 | |
| d820 | 77 a | 78 a | 47 | 100 a | 89 a | |
| d880 | 89 a | 100 a | 36 | 100 a | 100 a | |
| d920 | 94 a | 94 a | 47 | 100 a | 100 a | |
| e115 | 84 a | 94 a | 78 a | 78 a | 100 a | |
| e120 | 89 a | 84 a | 42 | 44 | 84 a | |
| e125 | 44 | 78 a | 31 | 100 a | 100 a | |
| e130 | 44 | 89 a | 36 | 100 a | 94 a | |
| e140 | 94 a | 89 a | 47 | 84 a | 89 a | |
| e150 | 94 a | 94 a | 47 | 78 a | 89 a | |
| e155 | 84 a | 89 a | 47 | 47 | 94 a | |
| e310 | 77 a | 47 | 77 a | 100a | 77 a | |
| e315 | 42 | 36 | 36 | 89 a | 47 | |
| e320 | 77 a | 47 | 42 | 100 a | 47 | |
| e325 | 47 | 42 | 42 | 94 a | 78 a | |
| e340 | 78 a | 78 a | 78 a | 89 a | 84 a | |
| e355 | 84 a | 84 a | 78 a | 94 a | 84 a | |
| e410 | 77 a | 77 a | 77 a | 89 a | 77 a | |
| e415 | 77 a | 47 | 47 | 84 a | 77 a | |
| e420 | 77 a | 47 | 47 | 89 a | 47 | |
| e425 | 77 a | 47 | 47 | 89 a | 47 | |
| e440 | 77 a | 77 a | 77 a | 89 a | 77 a | |
| e450 | 77 a | 47 | 77 a | 89 a | 77 a | |
| e460 | 77 a | 77 a | 77 a | 89 a | 77 a | |
| e465 | 77 a | 47 | 47 | 89 a | 47 | |
| e540 | 78 a | 77 a | 31 | 77 a | 77 a | |
| e575 | 77 a | 47 | 31 | 77 a | 77 a | |
| e580 | 78 a | 78 a | 77 a | 78 a | 78 a | |
a Included categories for each of the brief sets (the agreement percentage of at least 75%).
4.3. Validation Phase
Out of the 74, 69, 52, 73, and 74 categories respectively confirmed for GM, FM, E&D, CF, and VF brief sets in the Delphi process, a total of 71 categories/brief sets were rejected in the expert panel because their CVR, I-CVI, and K* values were less than 0.62, 0.78, and 0.74, respectively. Consequently, the final confirmed categories for the GM, FM, E&D, CF, and VF brief sets were reduced to 61, 57, 37, 59, and 57 categories respectively in the quantitative validation phase. The CVR and I-CVI values ranged from 0.80 to 1 among all finally confirmed categories/brief sets. Additionally, the lowest and highest S-CVI values of the brief sets were 0.95 and 0.98 respectively, calculated using the S-CVI/Ave method. According to the results, twelve categories (5 body functions, 3 activities and participation, and 4 environmental factors) were consistently confirmed across all five brief sets. Table 3 presents the quantitative validation statistics of the categories/brief sets obtained in the expert panel.
| ICF Code | Quantitative Validation Statistics CVR (I-CVI) K* | ||||||
|---|---|---|---|---|---|---|---|
| 2nd Level | 3rd Level | GM | FM | E & D | CF | VF | |
| s110 | 0.80 (0.90) 0.899 a | 0.80 (0.90) 0.899 a | 0.80 (0.90) 0.899 a | 0.40 (0.70) 0.660 | 0.40 (0.70) 0.660 | ||
| s730 | 0.80 (0.90) 0.899 a | 1 (1) 1 a | 1 (1) 1 a | - | - | ||
| s750 | 1 (1) 1 a | - | - | - | - | ||
| s760 | 1 (1) 1 a | 1 (1) 1 a | 0.80 (1) 1 a | - | - | ||
| s7700 | 0.80 (0.90) 0.899 a | 0.80 (0.90) 0.889 a | 0 (0.70) 0.660 | - | - | ||
| s7703 | 1 (1) 1 a | 0.80 (1) 1 a | 0.40 (0.60) 0.497 | - | - | ||
| b114 | 0.80 (0.80) 0.791 a | - | - | 0.80 (1) 1 a | 0.80 (0.90) 0.899 a | ||
| b117 | 0.80 (0.90) 0.899 a | 0.80 (1) 1 a | 0.80 (0.90) 0.899 a | 1 (1) 1 a | 0.80 (0.90) 0.899 a | ||
| b126 | - | - | 0.40 (0.60) 0.497 | 1 (1) 1 a | - | ||
| b1301 | 0.80 (0.80) 0.791 a | 0.80 (0.90) 0.889 a | 1 (1) 1 a | 1 (1) 1 a | 0.80 (0.90) 0.899 a | ||
| b134 | - | - | - | 0.80 (0.90) 0.899 a | - | ||
| b140 | 0.80 (1) 1 a | 0.80 (1) 1 a | 0.80 (1) 1 a | 0.80 (1) 1 a | 0.80 (1) 1 a | ||
| b144 | - | - | - | 1 (1) 1 a | 0.80 (0.90) 0.899 a | ||
| b1473 | - | 1 (1) 1 a | 1 (1) 1 a | - | 0.80 (0.90) 0.899 a | ||
| b1474 | 0.80 (0.90) 0.899 a | 0.80 (0.90) 0.889 a | 0.60 (0.70) 0.660 | - | 0.80 (0.90) 0.899 a | ||
| b152 | - | 0.80 (0.90) 0.889 a | 0.80 (0.90) 0.899 a | 0.80 (1) 1 a | - | ||
| b156 | 0.80 (0.90) 0.899 a | 1 (1) 1 a | 0.80 (1) 1 a | 0.80 (1) 1 a | 1 (1) 1 a | ||
| b163 | 0.80 (0.80) 0.791 a | 0.80 (0.90) 0.889 a | 0.80 (1) 1 a | 1 (1) 1 a | 0.80 (1) 1 a | ||
| b164 | - | 1 (1) 1 a | - | 1 (1) 1 a | 0.80 (1) 1 a | ||
| b167 | - | - | - | 1 (1) 1 a | - | ||
| b210 | - | 1 (1) 1 a | - | 0.80 (1) 1 a | 1 (1) 1 a | ||
| b230 | - | - | - | 1 (1) 1 a | - | ||
| b235 | 1 (1) 1 a | - | - | - | 1 (1) 1 a | ||
| b260 | 0.80 (1) 1 a | 1 (1) 1 a | 0.80 (1) 1 a | - | - | ||
| b265 | 0.40 (0.70) 0.660 | 1 (1) 1 a | 0.60 (0.60) 0.497 | 0.20 (0.50) 0.337 | 0.80 (0.90) 0.899 a | ||
| b280 | 0.80 (1) 1 a | 0.80 (1) 1 a | 0.80 (1) 1 a | - | - | ||
| b320 | - | - | - | 1 (1) 1 a | - | ||
| b440 | 0.20 (0.70) 0.660 | - | 0.80 (1) 1 a | 0.40 (0.70) 0.660 | - | ||
| b445 | 0.40 (0.60) 0.479 | - | 0.80 (1) 1 a | 0.60 (0.70) 0.660 | - | ||
| b455 | 1 (1) 1 a | 0.60 (0.70) 0.660 | 0.60 (0.70) 0.660 | - | - | ||
| b510 | - | - | 1 (1) 1 a | - | - | ||
| b525 | - | - | 0.80 (1) 1 a | - | - | ||
| b620 | - | - | 0.80 (1) 1 a | - | - | ||
| b710 | 1 (1) 1 a | 1 (1) 1 a | 0.80 (1) 1 a | - | - | ||
| b715 | 1 (1) 1 a | 0.80 (1) 1 a | 0.40 (0.70) 0.660 | - | - | ||
| b730 | 1 (1) 1 a | 0.80 (1) 1 a | 0.40 (0.60) 0.497 | - | - | ||
| b735 | 1 (1) 1 a | 0.80 (1) 1 a | 0.80 (1) 1 a | - | - | ||
| b740 | 1 (1) 1 a | 0.80 (1) 1 a | 0.80 (1) 1 a | - | - | ||
| b750 | 0.80 (1) 1 a | 0.40 (0.60) 0.497 | 0.40 (0.70) 0.660 | - | 0.20 (0.60) 0.497 | ||
| b755 | 1 (1) 1 a | 0.80 (1) 1 a | 0.80 (1) 1 a | - | - | ||
| b760 | 1 (1) 1 a | 1 (1) 1 a | 1 (1) 1 a | - | - | ||
| b765 | 0.80 (0.90) 0.899 a | 0.80 (0.90) 0.889 a | 0.80 (0.90) 0.899 a | - | - | ||
| b770 | 1 (1) 1 a | - | - | - | - | ||
| d110 | - | - | - | 1 (1) 1 a | 1 (1) 1 a | ||
| d115 | - | - | - | 1 (1) 1 a | - | ||
| d120 | - | 0.80 (0.90) 0.889 a | 1 (1) 1 a | 0.40 (0.70) 0.660 | 0.40 (0.70) 0.660 | ||
| d130 | - | 0.60 (0.70) 0.660 | - | 0.80 (0.90) 0.899 a | 0.80 (1) 1 a | ||
| d131 | - | 1 (1) 1 a | - | 1 (0.90) 0.899 a | 1 (1) 1 a | ||
| d133 | - | - | - | 1 (1) 1 a | - | ||
| d137 | - | - | - | 1 (1) 1 a | 0.80 (0.80) 0.791 a | ||
| d140 | - | - | - | 0.80 (1) 1 a | 1 (1) 1 a | ||
| d145 | - | 0.80 (1) 1 a | - | - | 0.80 (1) 1 a | ||
| d155 | 0.80 (0.90) 0.899 a | 1 (1) 1 a | 0.80 (0.80) 0.791 a | 0.80 (0.90) 0.899 a | 0.80 (1) 1 a | ||
| d160 | - | 0.80 (1) 1 a | - | 1 (1) 1 a | 0.80 (0.80) 0.791 a | ||
| d161 | 0.80 (0.90) 0.899 a | 0.80 (0.90) 0.889 a | 0.80 (0.90) 0.899 a | 1 (1) 1 a | 1 (1) 1 a | ||
| d166 | - | - | - | 0.80 (1) 1 a | 1 (1) 1 a | ||
| d170 | - | 0.80 (1) 1 a | - | 0.80 (1) 1 a | 0.80 (1) 1 a | ||
| d172 | - | - | - | - | - | ||
| d175 | - | - | - | 0.80 (1) 1 a | 0.60 (0.70) 0.660 | ||
| d177 | - | - | - | 0.60 (0.40) 0.245 | - | ||
| d210 | 0.20 (0.40) 0.245 | 0.20 (0.60) 0.497 | 0 (0.50) 0.337 | 0.60 (0.40) 0.245 | 0.40 (0.60) 0.497 | ||
| d220 | - | - | - | 0.60 (0.60) 0.497 | - | ||
| d230 | 1 (1) 1 a | 1 (1) 1 a | 1 (1) 1 a | 1 (1) 1 a | 1 (1) 1 a | ||
| d250 | - | - | - | 1 (1) 1 a | - | ||
| d310 | - | - | - | 1 (1) 1 a | - | ||
| d315 | - | - | - | 1 (1) 1 a | 0.80 (1) 1 a | ||
| d330 | - | - | - | 1 (1) 1 a | - | ||
| d335 | - | - | - | 1 (1) 1 a | 0.80 (1) 1 a | ||
| d350 | - | - | - | 1 (1) 1 a | - | ||
| d360 | - | - | - | 1 (1) 1 a | 0.80 (1) 1 a | ||
| d410 | 1 (1) 1 a | 0.60 (0.70) 0.660 | 0.40 (0.60) 0.497 | - | 0.40 (0.60) 0.497 | ||
| d415 | 1 (1) 1 a | 1 (1) 1 a | 0.80 (1) 1 a | - | 0.40 (0.70) 0.660 | ||
| d420 | 1 (1) 1 a | - | - | - | 0.40 (0.70) 0.660 | ||
| d430 | 1 (1) 1 a | 1 (1) 1 a | - | - | - | ||
| d435 | 1 (1) 1 a | - | - | - | 0.60 (0.70) 0.660 | ||
| d440 | - | 1 (1) 1 a | 0.80 (0.90) 0.899 a | - | 0.80 (1) 1 a | ||
| d445 | 0.80 (1) 1 a | 1 (1) 1 a | 1 (1) 1 a | - | 0.80 (1) 1 a | ||
| d450 | 1 (1) 1 a | - | - | - | 0.40 (0.60) 0.497 | ||
| d455 | 1 (1) 1 a | - | - | - | 0.80 (1) 1 a | ||
| d460 | 1 (1) 1 a | - | - | - | 1 (1) 1 a | ||
| d465 | 1 (1) 1 a | 0.20 (0.60) 0.497 | - | - | 0.80 (1) 1 a | ||
| d470 | 1 (1) 1 a | 0.60 (0.60) 0.497 | - | 0.80 (0.90) 0.899 a | 1 (1) 1 a | ||
| d510 | 0.80 (1) 1 a | 1 (1) 1 a | - | - | 0.80 (1) 1 a | ||
| d520 | 0.80 (1) 1 a | 1 (1) 1 a | - | - | 0.80 (1) 1 a | ||
| d530 | 1 (1) 1 a | 1 (1) 1 a | - | - | 0.80 (1) 1 a | ||
| d540 | 1 (1) 1 a | 1 (1) 1 a | - | - | 0.80 (1) 1 a | ||
| d550 | 0.40 (0.70) 0.660 | 0.80 (1) 1 a | 0.80 (1) 1 a | - | 0.20 (0.70) 0.660 | ||
| d560 | - | 0.80 (1) 1 a | 0.80 (1) 1 a | - | 0.40 (0.70) 0.660 | ||
| d570 | 0.80 (0.90) 0.899 a | 0.80 (0.90) 0.899 a | - | - | 0.80 (0.90) 0.899 a | ||
| d710 | - | - | - | 1 (1) 1 a | - | ||
| d750 | - | - | - | 0.80 (1) 1 a | - | ||
| d760 | - | - | - | 1 (1) 1 a | - | ||
| d820 | 0.20 (0.60) 0.497 | 1 (1) 1 a | - | 1 (1) 1 a | 0.80 (1) 1 a | ||
| d880 | 1 (1) 1 a | 1 (1) 1 a | - | 1 (1) 1 a | 1 (1) 1 a | ||
| d920 | 0.80 (1) 1 a | 0.80 (1) 1 a | - | 0.80 (1) 1 a | 1 (1) 1 a | ||
| e115 | 0.80 (1) 1 a | 0.80 (1) 1 a | 0.80 (0.90) 0.899 a | 0.80 (0.90) 0.899 a | 0.80 (1) 1 a | ||
| e120 | 1 (1) 1 a | 1 (1) 1 a | - | - | 1 (1) 1 a | ||
| e125 | - | 0.80 (1) 1 a | - | 0.80 (1) 1 a | 0.80 (1) 1 a | ||
| e130 | - | 0.80 (1) 1 a | - | 0.80 (1) 1 a | 0.80 (1) 1 a | ||
| e140 | 0.80 (1) 1 a | 0.80 (1) 1 a | - | 0.40 (0.60) 0.497 | 0.80 (1) 1 a | ||
| e150 | 0.80 (1) 1 a | 0.40 (0.70) 0.660 | - | 0.40 (0.70) 0.660 | 0.80 (1) 1 a | ||
| e155 | 0.80 (1) 1 a | 0.40 (0.70) 0.660 | - | - | 0.80 (1) 1 a | ||
| e310 | 0.20 (0.60) 0.497 | - | 0 (0.50) 0.337 | 0.80 (1) 1 a | 0.20 (0.60) 0.497 | ||
| e315 | - | - | - | 0.20 (0.70) 0.660 | - | ||
| e320 | 0.20 (0.60) 0.497 | - | - | 0.80 (1) 1 a | - | ||
| e325 | - | - | - | 0.80 (1) 1 a | 0.20 (0.70) 0.660 | ||
| e340 | 0.40 (0.70) 0.660 | 0.20 (0.70) 0.660 | 0.40 (0.50) 0.337 | 0.40 (0.60) 0.497 | 0.80 (1) 1 a | ||
| e355 | 1 (1) 1 a | 1 (1) 1 a | 0.40 (0.70) 0.660 | 0.80 (1) 1 a | 0.80 (1) 1 a | ||
| e410 | 0.80 (0.80) 0.791 a | 0.80 (0.80) 0.791 a | 0.80 (0.80) 0.791 a | 0.80 (0.90) 0.891a | 0.80 (1) 1 a | ||
| e415 | 0.40 (0.70) 0.660 | - | - | 0.20 (0.50) 0.337 | 0.20 (0.50) 0.337 | ||
| e420 | 0.20 (0.50) 0.337 | - | - | 0.80 (0.90) 0.891 a | - | ||
| e425 | 0.40 (0.70) 0.660 | - | - | 0.20 (0.60) 0.497 | - | ||
| e440 | 0.40 (0.60) 0.497 | 0.40 (0.50) 0.337 | 0.40 (0.50) 0.337 | 0.80 (0.90) 0.891 a | 0.60 (0.40) 0.245 | ||
| e450 | 0.80 (0.90) 0.899 a | - | 0.80 (0.90) 0.899 a | 1 (1) 1 a | 0.80 (1) 1 a | ||
| e460 | 1 (0.80) 0.791 a | 1 (0.80) 0.791 a | 0.80 (0.80) 0.791 a | 1 (1) 1 a | 1 (1) 1 a | ||
| e465 | 0.80 (0.90) 0.899 a | - | - | 1 (1) 1 a | - | ||
| e540 | 0.80 (1) 1 a | 0.60 (0.60) 0.497 | - | 0.80 (1) 1 a | 1 (1) 1 a | ||
| e575 | 0.80 (0.90) 0.899 a | - | - | 0.80 (1) 1 a | 0.80 (1) 1 a | ||
| e580 | 0.80 (0.90) 0.899 a | 0.80 (0.90) 0.899 a | 0.80 (0.90) 0.899 a | 1 (1) 1 a | 0.80 (1) 1 a | ||
| Statistics of the whole brief sets | 0.80 - 1 | 0.80 - 1 | 0.80 - 1 | 0.80 - 1 | 0.80 - 1 | ||
| 0.80 - 1 | 0.80 - 1 | 0.80 - 1 | 0.90 - 1 | 0.80 - 1 | |||
| 0.96 | 0.97 | 0.95 | 0.98 | 0.97 | |||
a The final included categories for each brief set.
5. Discussion
This study aimed at developing and validating five functional-based brief ICF category sets for 6-12-year-old children with CP from the perspective of Iranian OTs. These brief sets contained the minimal ICF categories that should be addressed in clinical settings where brief assessments are necessary for such children, given their significant functional limitations in GM, FM, E&D, CF, and VF. It is anticipated that functional-limitation-based brief sets can potentially result in a more precise description of the functioning of such children than diagnostic-based brief sets, as the environmental factors and ICF elements of activity and participation can cross diagnostic boundaries (11).
In these brief sets, the majority of categories confirmed in the components of body structures and functions related to movement and its associated structures/functions. This focus reflects the primary manifestations of CP, which are predominantly movement and postural disorders (28). Additionally, in these brief sets, the component of activity and participation received considerable attention from OTs, resulting in the most confirmed categories. This aligns with the development process of ICF-CS for children aged 0 - 18 with CP, where therapists often concentrated on areas of activity and participation, while physicians tended to focus on body structures (29). The component of body functions was the second most frequently addressed component among these brief sets. Interestingly, the ICF components of body functions and structures align with what is defined in the occupational therapy practice framework, which may explain why these components are emphasized by OTs (30).
In the domain of environmental factors, categories related to individual, family, and social attitudes were prominently addressed in these brief sets. It has been observed that such attitudes significantly influence the participation rate of children with CP in social, leisure, and daily activities (31, 32). This finding is consistent with the inclusion of these categories in the ICF-CS for children with CP (8).
In the E&D brief set, categories related to cognition and motor reflexes were prominently addressed by OTs. This focus is supported by evidence that motor reflexes, poor trunk control, and mental and cognitive challenges are associated with dysphagia and feeding problems in children with CP (33, 34). Regarding the CF brief set, the categories most approved by OTs were related to cognitive functions and the application of knowledge. Other studies have also highlighted the correlation between cognitive abilities and communication skills in children with CP (35, 36).
For the VF brief set, the most approved categories fell within the components of activity and participation and environmental factors. Although research on visual impairments in children with CP is limited, a systematic review has found that visual impairments can affect half of these children and significantly impact their quality of life (16). Further studies have shown that social life, community participation, daily activities, and transportation use are more adversely affected in children with severe visual impairments (37, 38).
According to the results, twelve categories were confirmed for all five brief sets implying that they should be addressed in the clinical brief assessments of children with CP regardless of their functional limitations. Intellectual, basic cognitive, perceptual, and attention functions as well as motivation and acquiring skills were some of such categories. It was consistent with our expectation since the presence of cognitive impairments in a large proportion of children with CP has been approved and it has been demonstrated that these impairments expose them to learning disabilities and problems in peer relations (39, 40). Carrying out daily routines and individual, family, and social attitudes were some other common categories among all brief sets. The carrying out of daily activities is the highest priority of parents of children with CP (41), however, it has been demonstrated that while increasing the impairments of children with CP, their participation in everyday activities was more restricted (42). Moreover, as stated by parents, participation in everyday activities can affected by individual and social attitudes in such children (43). These results highlight the common categories to be addressed in the brief assessments of children with CP regardless of their limitations.
We employed the Delphi technique to develop the brief sets in this study, a method often utilized in previous research for developing or validating ICF core sets (8, 44, 45). The Delphi process in this study achieved a 100% response rate across its rounds, ensuring no attrition (46, 47). Additionally, we employed the calculation of CVR, I-CVI, K*, and S-CVI to assess the content validity of each brief set. However, this study encountered some limitations. Firstly, as these brief sets were developed from the perspective of OTs, the priorities of children and/or their families were not included in the creation of these brief sets. Secondly, while these brief sets address five types of functional limitations commonly associated with CP or its secondary consequences, other potential functional limitations related to CP should be considered in clinical brief assessments. Thirdly, these brief sets specify which categories should be minimally addressed in clinical brief assessments based on functional limitations but do not specify how to measure these categories. Nevertheless, this study has notable strengths: it was the first to develop brief sets based on functional limitations, and these five brief sets can result in more precisely addressing functioning and related phenomena in clinical brief assessments.
5.1. Conclusions
Five brief sets containing 61, 57, 37, 59, and 57 categories, respectively, were confirmed by Iranian OTs for 6-12-year-old children with CP who have significant functional limitations in GM, FM, E&D, CF, and VF. These brief sets also demonstrated excellent content validity from the perspective of Iranian OTs. They encompass the minimal categories that should be addressed by OTs in clinical settings when a brief assessment is required for such children based on their functional limitations. Therefore, it is recommended that OTs utilize these brief sets in their clinical assessments of 6 - 12-year-old children with CP. While these brief sets identify what aspects of functioning should be addressed based on children's functional limitations, they do not prescribe how these aspects should be measured. Consequently, further research is necessary to develop or recommend appropriate measurement tools for assessing these aspects.