1. Background
The diagnostic and statistical manual of mental disorders (DSM-5) serves as the primary diagnostic system, providing operational criteria (1) for borderline personality disorder (BPD) and other psychiatric conditions to establish a common language among mental health professionals (2). However, it has been criticized for not accounting for the dimensional nature of BPD syndromes and symptoms, as well as the heterogeneity among BPD patients (3-5). As a result, individuals with severe emotional instability and interpersonal difficulties may not qualify for a BPD diagnosis if they exhibit fewer than four symptoms (6).
In response to these issues, the DSM-5 introduced the alternative model of personality disorder (AMPD), representing a significant step toward conceptualizing personality disorders dimensionally. The AMPD includes pathological personality domains and traits that align with normal equivalents in the "Big Five" model, which is based on factor analyses of normal personality domains: Extraversion, agreeableness, openness, conscientiousness, and neuroticism. Thus, all personality pathology traits can be viewed as maladaptive variations of the "Big Five" traits (2, 7, 8). While this model has made progress in defining personality disorders through the five-factor model of maladaptive traits/domains, DSM-5 authors retained categorical frameworks alongside this dimensional approach (2, 9).
To further address the limitations of categorical nosology (10, 11), the hierarchical taxonomy of psychopathology (HiTOP) was introduced as a quantitative nosology for mental illness. This approach is grounded in empirical research that examines the natural organization of psychopathology (12, 13). It includes factor-analytic studies that seek to detect symptoms and personality traits to identify empirical dimensions in psychopathology (14, 15), person-centered studies to identify natural classes among syndromes (16, 17), and factor analysis studies focused on shared psychopathologies and comorbidities across disorders (18, 19). This quantitative approach aims to improve upon categorical approaches by constructing mental disorders based on shared symptoms and traits, integrating comorbid disorders into spectra, and describing psychopathology dimensionally (12, 20, 21).
In the HiTOP model, BPD is conceptualized according to two dimensions: The distress sub-factor of negative affectivity and antagonism, based on research linking BPD to internalizing and externalizing dimensions (12, 19, 22, 23). Thus, it is hypothesized that antagonism-related traits (i.e., attention-seeking, manipulativeness, grandiosity, callousness, and deceitfulness) and negative affectivity-related traits (i.e., anxiousness, emotional lability, hostility, perseveration, low restricted affectivity, submissiveness, and separation insecurity) are significant factors in assessing and diagnosing BPD (24) and can be measured by tools such as the Personality Inventory for DSM-5 (12).
It is important to note that this model shows promise for both clinical practice and research settings (25). However, its clinical utility and readiness for real-world application remain subjects of ongoing debate (25-27). Many mental health professionals find a dimensional model of personality disorders, including HiTOP (28), to be more applicable than the DSM's categorical approach for aspects such as clinical decision-making, treatment planning, therapeutic communication, case formulation, and in describing functionality, personality, and psychopathology (29-31). Using HiTOP’s dimensional constructs can facilitate real-time monitoring, inform clinical decisions, guide intervention strategies, and improve communication. For example, evaluating the dimensions of emotional lability or hostility during treatment is more practical than simply determining whether the patient meets the "Explosive Anger" criterion (13).
Establishing operational standards is essential to implement HiTOP in clinical settings. For evaluating the HiTOP construct, it is critical to recognize the continuum of normal and pathological traits in terms of severity. This approach allows clinicians to develop treatment plans for patients with similar psychopathology by accounting for the severity of their symptoms (25). At the same time, the HiTOP consortium suggests that empirically based cut-off points are necessary for clinical decision-making (25, 32). Several studies have aimed to establish operational criteria for assessing psychopathology within the HiTOP framework. These efforts include research on depression and anxiety symptoms in general populations (33, 34), somatoform and eating disorders among university students (35), and internalizing symptom dimensions in children and adolescents (36).
Regarding BPD, recent research has introduced a self-report measure called the Dimensional Clinical Personality Inventory-BPD, designed to assess pathological traits associated with BPD in line with HiTOP principles. While this tool’s psychometric properties have been evaluated among adults in the Brazilian community, the absence of a defined cut-off point currently limits its use for screening purposes (37). Given this background, further evidence is necessary to establish operational criteria for diagnosing BPD within the HiTOP framework.
The HiTOP model has faced criticism for systemic bias related to culture, as it is based on studies conducted with Western samples. Personality is a cultural phenomenon influenced by social norms, with each culture’s history, values, and moral judgments guiding individuals and society in unique ways that affect personality development. Additionally, each culture provides methods for endorsing, expressing, accepting, and rejecting specific behaviors, which in turn shape personality traits and norms (38). Therefore, it is essential to consider the cultural context when diagnosing and treating individuals with personality disorders (39, 40). The diagnosis of BPD, in particular, is sensitive to cultural background (41, 42). Consequently, the HiTOP consortium has prioritized multicultural perspectives and focused on empirical research to demonstrate cross-cultural differences in order to enhance the model's generalizability (43, 44). Thus, one objective of this study was to identify the predictive domains of BPD in Iranian clinical samples.
2. Objectives
This study primarily aimed to investigate the clinical utility of the HiTOP model in diagnosing BPD within the Iranian population. Specifically, it sought to integrate the HiTOP model into clinical practice and replicate previous research regarding the underlying structure of BPD in an Iranian sample. By considering the cultural background of patients, the study aimed to implement a more flexible and tailored diagnostic strategy.
3. Methods
3.1. Participants
This cross-sectional study was conducted from June 2020 to September 2021 in Tehran, Iran. Two samples were recruited for the study. The clinical sample consisted of 113 inpatients who were hospitalized for various reasons, including paranoid ideation, risky behaviors, aggression, and poor adherence to treatment. Inclusion criteria for this sample included a primary diagnosis of BPD, Iranian nationality, fluency in Persian, being between 18 and 50 years old, and having completed at least a high school education. Additionally, patients were selected if they were in a stable mood and not experiencing psychotic episodes or impaired consciousness due to any medical conditions, including recent use of sedative-hypnotic drugs. The second sample included 100 participants from the general population of Tehran, Iran, who were selected through judgment sampling. The inclusion criteria for this sample required participants to be Iranian, Farsi-speaking adults aged 18 to 50, with a score of less than five on the BPD subscale of the Structured Clinical Interview for DSM-5 Screening Personality Questionnaire. Exclusion criteria for both samples included failing to complete the questionnaire validly or leaving more than 20% of the assessment tools unanswered.
3.2. Measurements
3.2.1. Personality Inventory for DSM-5
The Personality Inventory for DSM-5 (PID-5) assesses the five maladaptive personality domains and their relevant traits outlined in section III of the DSM-5 (2, 45). Many studies have examined the validity and reliability of this questionnaire in different clinical populations and cultures (46). Shojaei et al. (47) reported satisfactory psychometric properties for the Persian version of the PID-5. In this study, Cronbach’s alpha ranged from 0.84 (antagonism) to 0.94 (Psychoticism) for the domains, and from 0.92 (Depressivity) to 0.53 [(low) Restricted Affectivity].
3.2.2. Personality Assessment Inventory-Borderline Scale
This scale, comprising 24 items, measures BPD symptoms across four subscales: Affective instability, self-harm/impulsivity, interpersonal relationships, and identity problems. A study conducted on an Iranian undergraduate sample indicated that the 4-factor model adequately fit the data, with the scale exhibiting acceptable internal consistency (0.69 to 0.82) (48). The Personality Assessment Inventory-Borderline Scale (PAI-BOR) demonstrated satisfactory internal consistency in the current study (Cronbach’s α = 0.90).
3.2.3. Structured Clinical Interview for DSM-5 Screening Personality Questionnaire
The BPD section of the Structured Clinical Interview for DSM-5 Screening Personality Questionnaire (SCID-5-SPQ) consists of 15 items developed based on the diagnostic criteria for BPD in the DSM-5. Each item requires a "Right" or "Wrong" response (6). The Persian version of this questionnaire showed acceptable psychometric properties in the general Iranian population (49, 50). This scale exhibited adequate internal consistency in this research (Cronbach’s α = 0.90).
3.2.4. Structured Clinical Interview for DSM-5 Personality Disorders-BPD Section
This structured interview, based on the DSM-5 diagnostic criteria for BPD and nine other personality disorders, has established psychometric properties in European (51) and Iranian (52) populations. In the clinical sample, the BPD section of the SCID-5-PD revealed adequate reliability (Cronbach’s α = 0.73).
3.3. Procedures
3.3.1. Clinical Sampling
Upon admission to the inpatient ward, an attending psychiatrist or a group of psychiatric residents evaluated each patient's clinical history. Patients diagnosed with primary BPD were referred to the first author, a Ph.D. student in clinical psychology who was well-trained in conducting structured and semi-structured diagnostic interviews. After obtaining informed consent and explaining the research objectives and procedures, the patients completed the PID-5 and PAI-BOR. Subsequently, the BPD section of the SCID-5-PD was administered. A total of 130 patients were referred by the psychiatric team; however, 10 were not evaluated due to medical or psychiatric conditions or medication use that affected their consciousness and cognitive abilities, such as current dizziness, manic episodes, major depressive episodes, or psychotic episodes. Seven patients who left more than 20% of the questionnaires blank were excluded from the study. Data from the remaining 113 patients were analyzed, revealing that 87 patients met the criteria for a BPD diagnosis, while 26 exhibited subclinical BPD symptoms.
3.3.2. Nonclinical Sampling
Participants were recruited from parks, libraries, and a residential area in Tehran, Iran. The researcher provided a thorough explanation of the study's objectives and procedures to potential participants. Those who agreed to participate and met the inclusion criteria signed the informed consent form and completed the BPD subscale of the SCID-5-SPQ. Participants scoring less than 5 on this subscale proceeded to complete the remaining questionnaires.
3.4. Data Analysis
Data analysis was conducted using SPSS software version 26 (IBM Corp., Armonk, NY, USA). Descriptive statistics were employed to describe demographic characteristics and clinical variables and to check for multivariate normality. The Student's t-test was used to examine sex differences. To compare the BPD, subclinical BPD, and nonclinical groups, multivariate analysis of variance (MANOVA) and Cohen's d were calculated to determine whether there were differences among the three groups regarding PAI-BOR and PID-5 domain and trait scores. Pearson correlations were run to measure the association between PID-5 domains and BPD severity in the BPD sample.
Several analyses were performed to evaluate the diagnostic validity of the HiTOP model for BPD. First, a linear regression analysis (inter-method) was conducted on 87 BPD patients to test the predictive power of the hypothetical domains (negative affectivity and antagonism). Subsequently, new scores were generated for all participants based on the regression equation for predicting BPD severity. These new scores formed a new scale for BPD screening. Receiver operating characteristics (ROC) analyses were conducted to estimate the area under the curve (AUC) and standard error (SE) to examine the accuracy of the new scale. Sensitivity (the ability to correctly identify BPD patients) and specificity (the ability to correctly identify individuals without BPD) were utilized as metrics to evaluate the diagnostic efficiency of the scales. All analyses were repeated to build the proposed model, with the difference lying in the method of the second regression, which was stepwise, using the five domains as independent variables. Cohen's kappa coefficient was computed to assess the inter-rater reliability of these BPD diagnosis systems.
4. Results
4.1. Descriptive Statistics and Preliminary Analysis
The distribution of demographic variables among BPD patients, subclinical BPD patients, and nonclinical participants is presented in Table 1. The total scores of the PAI-BOR and PID-5 were normally distributed, as skewness and kurtosis fell between -1 and +1, except for antagonism (kurtosis = 1.46). Student's t-tests were conducted separately on both the clinical and nonclinical samples to assess whether male and female patients and participants differed in terms of age, PAI-BOR total scores, and PID-5 domains. Results indicated no significant differences between men and women in age (P > 0.28), PAI-BOR total score (P > 0.06), and PID-5 domains (P > 0.11) in both samples.
| Variables | BPD (N = 87) | Subclinical BPD (N = 26) | Nonclinical (N = 100) |
|---|---|---|---|
| Age, mean (SD) | 27.23 (7.31) | 28 (8.37) | 30.28 (9.82) |
| Sex | |||
| Female | 64 (73.6) | 21 (80.8) | 72 (72) |
| Male | 23 (26.4) | 5 (19.2) | 28 (28) |
| Education | |||
| High school diploma | 66 (76.7) | 17 (68) | 43 (43) |
| Bachelor's degree | 16 (18.6) | 7 (28) | 34 (34) |
| Postgraduate degree | 4 (4.7) | 1 (4) | 18 (18) |
| Marital status | |||
| Single | 64 (73.6) | 18 (75) | 60 (60) |
| Married | 15 (17.2) | 3 (12.5) | 40 (40) |
| Divorced | 7 (8) | 2 (8.3) | 0 |
| Widowed | 1 (1.1) | 1 (4.2) | 0 |
Abbreviations: BPD, borderline personality disorder; SD, standard deviation.
a Values are expressed as No. (%) unless otherwise indicated.
4.2. Multivariate Analysis of Variance
Table 2 presents the means and standard deviations for the PAI-BOR, the 25 traits, and the 5 domains of PID-5, along with the MANOVA results. Negative affectivity (partial Eta squared ≥ 28) distinctly differentiated BPD patients from the non-BPD sample, while Disinhibition (partial Eta squared ≥ 33) differentiated all three samples.
| Variables | Mean (SD) | F | P | Tukey Post-hoc | Partial η2a | ||
|---|---|---|---|---|---|---|---|
| BPD (N = 87) | Subclinical BPD (N = 26) | Nonclinical (N = 100) | |||||
| PAI-BOR | 49.95 (10.41) | 36.23 (14.22) | 26.91 (8.88) | 117.08 | 0.0001 | B > S > N | 0.52 |
| PID-5 trait facets | |||||||
| Anhedonia | 6.71 (5.44) | 10.46 (6.71) | 6.88 (4.35) | 28.99 | 0.0001 | B = S > N | 0.21 |
| Depressivity | 23.10 (10.08) | 16.88 (10.69) | 8.07 (5.89) | 73.85 | 0.0001 | B > S > N | 0.41 |
| Intimacy avoidance | 6.68 (4.06) | 6.04 (5.19) | 3.54 (2.62) | 15.42 | 0.0001 | B = S > N | 0.12 |
| Suspiciousness | 12.22 (3.66) | 9.31 (2.89) | 8.19 (3.05) | 35.21 | 0.0001 | B > S = N | 0.25 |
| Withdrawal | 14.19 (6.35) | 11.77 (6.62) | 9.68 (5.79) | 12.59 | 0.0001 | B = S; S = N; B > N | 0.10 |
| Ec00centricity | 21.69 (9.61) | 12 (6.71) | 8.90 (7.90) | 53.62 | 0.0001 | B > S = N | 0.33 |
| Perceptual dysregulation | 15.63 (7.63) | 10.13 (6.57) | 8.89 (5.92) | 24.04 | 0.0001 | B > S = N | 0.18 |
| Unusual beliefs and experiences | 10.19 (5.62) | 7.35 (5.20) | 6.19 (4.66) | 14.30 | 0.0001 | B > S = N | 0.12 |
| Anxiousness b | 17.02 (5.35) | 12.83 (5.07) | 0.57 (0.49) | 26.32 | 0.0001 | B > S = N | 0.20 |
| Emotional lability b | 13.86 (4.70) | 9.38 (4.55) | 6.72 (3.93) | 63.19 | 0.0001 | B > S > N | 0.37 |
| Hostility b | 17.83 (5.17) | 12.19 (4.69) | 10.46 (3.84) | 63.01 | 0.0001 | B > S = N | 0.37 |
| (Low) restricted affectivity b | 12.20(3.66) | 11.86 (3.72) | 13.16 (3.64) | 2.23 | 0.11 | ||
| Separation Insecurity b | 10.35 (5.47) | 8.02 (5.66) | 7.34 (4.12) | 9.007 | 0.0001 | B = S; S = N; B > N | 0.008 |
| Submissiveness b | 12.22 (3.66) | 9.31 (2.89) | 8.19 (3.05) | 0.80 | 0.45 | ||
| Attention seeking b | 13.46 (4.88) | 10.58 (4.75) | 9.97 (4.73) | 12.78 | 0.0001 | B > S = N | 0.10 |
| Callousness b | 13.10 (5.74) | 10 (5.34) | 5.26 (3.47) | 63.78 | 0.0001 | B > S > N | 0.37 |
| Deceitfulness b | 12.91 (5.55) | 9.50 (5.46) | 8.13 (4.63) | 20.53 | 0.0001 | B > S = N | 0.16 |
| Grandiosity b | 8.67 (4.17) | 6.54 (3.80) | 6.89 (3.42) | 6.19 | 0.002 | B > S = N | 0.05 |
| Manipulativeness b | 7.95 (3.13) | 5.60 (3.47) | 5.63 (2.63) | 15.92 | 0.009 | B > S = N | 0.13 |
| Distractibility | 17 (5.78) | 13.03 (7.05) | 8.76 (5.19) | 48.86 | 0.0001 | B > S > N | 0.31 |
| Impulsivity | 11.67 (3.70) | 8.04 (4.15) | 5.54 (2.73) | 78.29 | 0.0001 | B > S > N | 0.42 |
| Irresponsibility | 8.83 (3.85) | 6.35 (4.58) | 3.68 (2.59) | 52.38 | 0.0001 | B > S > N | 0.33 |
| (Low) rigid perfectionism | 15.08 (5.65) | 15.47 (5.005) | 16.03 (5.38) | 0.70 | 0.49 | ||
| Risk Taking | 25.24 (8.62) | 19.44 (7.53) | 15.25 (5.90) | 43.31 | 0.0001 | B > S > N | 0.29 |
| PID-5 Domains | |||||||
| Detachment | 68.47 (21.78) | 54.45 (26.05) | 36.37 (16.93) | 58.69 | 0.0001 | B > S > N | 0.35 |
| Psychoticism | 47.50 (20.08) | 29.49 (15.76) | 23.97 (16.06) | 41.77 | 0.0001 | B > S = N | 0.28 |
| Negative affectivity b | 89.25 (18.64) | 69.04 (18.64) | 62.56 (17.41) | 51.94 | 0.0001 | B > S = N | 0.33 |
| Antagonism b | 56.08 (17.13) | 42.22 (12.54) | 48.39 (9.05) | 13.86 | 0.0001 | B > S = N | 0.11 |
| Disinhibition | 77.81 (17.15) | 62.32 (19.53) | 48.58 (8.22) | 100.52 | 0.0001 | B > S > N | 0.48 |
Abbreviations: DSM-5, diagnostic and statistical manual of mental disorders; PID-5, Personality Inventory for DSM-5; PAI-BOR, Personality Assessment Inventory-Borderline Scale; BPD, borderline personality disorder.
a Partial η2 is the effect size (0.01 is small; 0.06 is medium; ≥ 0.14 is large).
b The hypothesized traits for BPD diagnosis in HiTOP.
4.3. Evaluating the Hypothesized HiTOP-BPD Model
4.3.1. Correlation
Table 3 shows Pearson correlations between the PID-5 domains and the BPD symptoms.
Abbreviation: PAI-BOR, Personality Assessment Inventory-Borderline Scale.
a α represents Cronbach's alpha.
b P < 0.01.
4.3.2. First Regression Analysis
In the first regression analysis, only the hypothesized scales (negative affectivity and antagonism) were included in the model. The negative affectivity and antagonism domains [F (2, 84) = 35.58, P < 0.001] predicted BPD severity; however, antagonism did not significantly predict it (Table 4). Based on the regression, an equation was derived, and each individual in the clinical and general samples was assigned a score. The scores were normally distributed, as skewness and kurtosis fell between -1 and +1.
| PAI-BOR, Method, and Predictors | B | S.E. | Beta | t | Sig. | R2 | R2 Change |
|---|---|---|---|---|---|---|---|
| First | |||||||
| Inter | 0.45 | 0.44 | |||||
| Constant | 15.90 | 4.20 | - | 3.78 | 0.0001 | ||
| Negative affectivity | 0.37 | 0.05 | 0.66 | 7.33 | 0.0001 | ||
| Antagonism | 0.01 | 0.05 | 0.02 | 0.32 | 0.74 | ||
| Second | |||||||
| Stepwise | 0.54 | 0.53 | |||||
| Constant | 8.40 | 4.26 | - | 1.97 | 0.05 | ||
| Negative affectivity | 0.29 | 0.04 | 0.52 | 6.27 | 0.0001 | ||
| Disinhibition | 0.19 | 0.05 | 0.32 | 3.90 | 0.0001 |
Abbreviation: PAI-BOR, Personality Assessment Inventory-Borderline Scale.
4.3.3. Receiver Operating Characteristic Curves and Criterion Validity
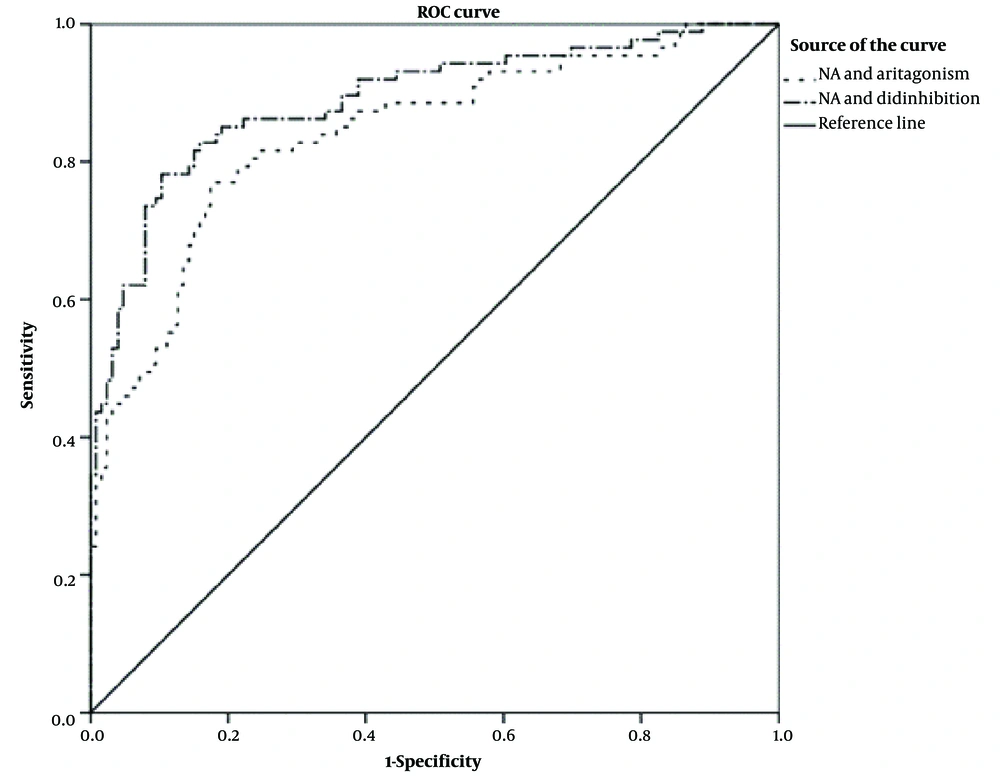
The antagonism/negative affectivity model measure (cut-point = 44.65) demonstrated a sensitivity of 81% and a specificity of 76% (AUC = 0.875, 95% CI 0.82 - 0.92, SE = 0.026; P = 0.0001), as expressed by the composite score in Figure 1. To assess the diagnostic agreement between the SCID-5-PD and the two-domain model measure in detecting BPD cases, the kappa coefficient was calculated (approximately t = 8.18, SE = 0.05, P < 0.0001), indicating a moderate level of agreement between the two scales, as suggested by Cohen (53).
ROC curve of the HiTOP-BPD algorithm (antagonism/negative affectivity) and the proposed BPD algorithm (disinhibition/negative affectivity) (ROC, receiver operating characteristic; NA, negative affectivity; HiTOP, hierarchical taxonomy of psychopathology; BPD, borderline personality disorder).
4.4. The Proposed Model
4.4.1. Second Regression
Two regression analyses were conducted to determine whether other domains were more valid in diagnosing BPD and its severity. As shown in Table 4, negative affectivity and disinhibition (standardized coefficients beta > 0.30) significantly predicted BPD severity [F (5, 81) = 21.22, P < 0.001]. In the final regression analysis, only negative affectivity and disinhibition were included in the model to calculate more accurate B coefficients [F (2, 84) = 49.56, P < 0.001]. Once again, each individual was assigned a score based on the obtained regression equation. The kurtosis and skewness of the scores were -0.55 and 0.22, respectively. The regression analyses indicated that the HiTOP-BPD model accounted for 45% of the variance, while the proposed model explained 54%.
4.4.2. Receiver Operating Characteristic Curves and Criterion Validity
According to ROC curves, the negative affectivity-disinhibition model, measured with a cut-off point of 42, demonstrated a sensitivity of 85% and a specificity of 81% (AUC = 0.893, 95% CI 0.84 - 0.93, SE = 0.023; P = 0.0001), as shown by the composite score in Figure 1. Individuals with a score greater than 42 were classified as BPD patients. With a kappa coefficient of 0.63, the agreement between the categorical diagnostic system and this measure in detecting BPD cases was substantial (approximately t = 9.38, SE = 0.05, P < 0.0001) (53).
5. Discussion
This cross-sectional study is the first to examine the clinical utility of the HiTOP model in diagnosing BPD within an Eastern cultural context, specifically in Iran. The primary objective of this investigation was to establish an operational framework for evaluating BPD psychopathology based on HiTOP constructs. The assessment of the model's clinical utility within a clinical setting presents initial evidence supporting the robust diagnostic validity of both the HiTOP-BPD algorithm (antagonism/negative affectivity) and the proposed BPD algorithm (disinhibition/negative affectivity). These results offer a novel perspective on the dimensional assessment of BPD pathology and serve as an initial step in conceptualizing BPD through the quantitative nosology of HiTOP.
The regression analysis revealed a significant predictive relationship between negative affectivity and disinhibition concerning BPD severity. However, contrary to HiTOP's conceptualization of BPD, antagonism did not demonstrate a significant predictive effect. Consequently, it was observed that the disinhibition-negative affectivity algorithm exhibited greater diagnostic validity for BPD diagnosis compared to the antagonism-negative affectivity algorithm. Furthermore, the MANOVA results indicated that while antagonism had a moderate effect in distinguishing BPD patients from those with sub-clinical BPD, Disinhibition exerted the strongest effect. Consistent with these findings, the AMPD associates BPD with negative affectivity and disinhibition, given that criterion B of BPD comprises traits related to these domains. These results align with previous research conducted by Fang et al. (54), which revealed that negative affectivity and disinhibition (not antagonism) predict BPD pathology. Collectivism, a common cultural characteristic between Iran and China (55), may explain these consistent results. Additionally, Calvo et al. (56) demonstrated that the three domains—negative affectivity, disinhibition, and antagonism—can be used to differentiate between patients with BPD and those without. However, these findings contradict those of Hopwood et al. (22), who demonstrated an inverse relationship between levels of agreeableness (low antagonism) and the severity of BPD pathology over time. Moreover, Forbes et al., in a study involving a large sample of psychiatric outpatients, concluded that BPD demonstrates cross-loading on core internalizing and antagonism (23).
Although it is unclear why antagonism did not predict BPD in this investigation, there are several interpretations of these findings. One plausible explanation pertains to the composition of the inpatient samples, some of whom were hospitalized due to disinhibited behaviors. Consequently, the increased Disinhibition scores observed within the sample may have skewed the results. Externalizing-disinhibition-related behaviors, such as uncontrolled aggression and risk-taking behaviors, often necessitate emergency interventions and hospitalization services (57). Given the mean age of the BPD inpatient sample and the potential influence of lifespan on personality pathology, heightened levels of Disinhibition could be anticipated (58).
Additionally, it is conceivable that BPD patients characterized by higher levels of antagonism and lower levels of disinhibition may predominantly seek treatment in outpatient centers. These individuals might receive comparatively less clinical attention or require hospitalization less frequently, as they are less prone to exhibiting high-risk behaviors. Consequently, future research should strive to replicate the current study across diverse clinical settings, including outpatient centers. Another explanation could relate to the relatively lower variance of antagonism observed in this research, which may have impacted the regression analysis. It is plausible that patients might underreport antagonism-related traits, particularly when they possess limited insight, as higher levels of antagonism are often concealed (59). Hence, it is recommended that future studies replicate this investigation by utilizing informant forms of the Personality Inventory for DSM-5 (PID-5). Notably, significant others may provide a more realistic portrayal of the patients' traits and behaviors.
Another notable aspect of the present study is the discernment capability exhibited by negative affectivity and disinhibition in distinguishing BPD patients from non-BPD participants, including subclinical BPD patients and nonclinical participants. These findings hold promise for enhancing the validity of HiTOP in identifying BPD patients. Establishing a cut-point is instrumental in delineating the boundary between disorder and non-disorder, as well as determining severity levels. The insights gained from this study regarding cut points could serve as a foundation for future research aimed at examining more accurate cut points. Further research should also examine the incremental validity of the HiTOP model in BPD patients, with a larger sample comprising clinical, subclinical BPD, and non-BPD patients.
5.1. Strengths and Limitations of the Study
The strength of the current study lies in its utilization of two distinct and adequately sized samples, encompassing both nonclinical and inpatient populations. However, it is imperative to approach the interpretation of these findings with an awareness of the study's limitations. Firstly, the clinical samples included in this study consisted solely of inpatients, many of whom had engaged in high-risk behaviors or exhibited suicidal tendencies. Future research should aim to replicate these findings with samples that represent both BPD inpatient and outpatient populations. Secondly, the assessment of personality pathology traits relied solely on self-report scales. Incorporating alternative forms of personality assessment, such as a Structured Clinical Interview for the DSM-5 alternative model for personality disorders, may yield more precise results. The most notable limitation is the absence of a distinct clinical sample to replicate the obtained results, which would allow for testing the generalizability of the identified cut-point.
5.2. Conclusions
This investigation provides valuable initial evidence suggesting that HiTOP could serve as a valid model for assessing and diagnosing BPD pathology within Iranian samples. Consequently, researchers and practitioners are encouraged to consider the utility of HiTOP and the introduced measures in both research and clinical contexts.