1. Background
In childhood, one of the most common mental disorders is attention deficit hyperactivity disorder (ADHD) (1). The ADHD affects 7.6% of children aged 3 to 12 years and 5.6% of adolescents aged 12 to 18 years (2). It is associated with a higher risk of long-term social problems, school dropout, underemployment, drug abuse, and antisocial conduct (1). The typical symptoms of ADHD, such as impulsivity, hyperactivity, and inattention, may interfere with parent-child interactions and make parents of ADHD children feel more stressed (3). Over time, parents may adopt maladaptive and inefficient parenting techniques to cope with these difficulties (4). Since bad parenting is one of the most reliable indications of unfavorable long-term outcomes in children with behavioral disorders, it is imperative to alter these habits successfully (3).
The need for multimodal therapy for ADHD, which includes pharmaceutical and non-pharmacological treatment (parent education and social skills training, for example), has lately been highlighted in several treatment guidelines (5, 6). Parent management training (PMT) has been established as an effective technique for improving core ADHD symptoms by equipping parents with strategies to manage their child’s behavior (7). However, traditional in-person delivery of PMT can face accessibility limitations due to geographical barriers, scheduling conflicts, and cost considerations. Videoconference delivery of PMT presents a promising alternative, potentially increasing accessibility and convenience for families (8, 9). Previous studies demonstrated that network-based education and nursing education for ADHD families increased parents’ better curative effect, which may be an adjuvant therapy impact (9, 10).
2. Objectives
The present study primarily aimed to compare the effectiveness of in-person versus videoconference PMT for children diagnosed with ADHD. Specifically, we aimed to assess the impact of these videoconference PMTs on core ADHD symptoms, conduct, social, anxiety, and psychosomatic problems. By addressing the critical gap in accessibility to PMT due to geographical and logistical barriers, this study pioneers the exploration of videoconference technology to enhance the reach and effectiveness of ADHD management.
3. Methods
3.1. Design
A randomized clinical trial with a parallel design was conducted on 90 parents from September 6, 2022, to October 21, 2022, in Amin and Khorshid hospitals in Isfahan, Iran.
3.2. Inclusion and Exclusion Criteria
Parents with ADHD children between the ages of 3 and 12 who met the diagnostic and statistical manual of mental disorders (DSM-5) standards for ADHD diagnosis (11) were enrolled. All participating parents or family members provided written informed consent. The inclusion criteria for the study were as follows: Undergoing medical treatment for ADHD, not having any concurrent physical illness, having internet access, and expressing willingness to participate. Exclusion criteria included child oppositional defiant disorder (ODD) or conduct problems, incomplete questionnaires, and inability to communicate.
Enrolled parents completed baseline assessments and then participated in the 6-week PMT sessions (in-person or videoconference), after which post-intervention assessments were conducted. Both mothers and fathers were eligible to participate in the study. In cases where both parents were available, we encouraged joint participation. However, in single-parent households or when only one parent was able to commit to the full program, we allowed individual participation. Subsequent follow-up assessments were performed two months after completing the PMT session.
The determination that ADHD patients in the study were not suffering from ODD involved a comprehensive diagnostic assessment conducted by a psychiatrist specializing in child and adolescent mental health, typically encompassing structured clinical interviews, behavioral observations, and the utilization of diagnostic criteria outlined in the DSM-5 to differentiate between ADHD and ODD symptoms (11). Drug treatment was commenced for each participant based on individual clinical indications and was supervised by a qualified healthcare provider specializing in managing ADHD. While the specifics of timing and treatment regimen initiation may have varied among parents, efforts were made to adhere to established clinical protocols and guidelines. It is pertinent to acknowledge that discrepancies in this aspect could potentially introduce bias and influence the outcomes of the two study groups. Therefore, meticulous documentation of the timing and regimen of drug treatment initiation was maintained, and statistical analyses may incorporate adjustments to address any discrepancies between groups in this regard.
3.3. Ethical Statement
The present study was approved by the Ethics Committee of Isfahan University of Medical Sciences (IR.MUI.MED.REC.1401.194) and the Iranian Registry of Clinical Trials (IRCT) code is IRCT20211004052670N4. Prior to their involvement in the research, every subject provided informed permission subsequent to acquiring a comprehensive understanding of the methods. The experiment adhered to the revised rules of the Declaration of Helsinki. The trial was devoid of any commercial influence.
3.4. Videoconference Parent Management Training
The videoconference PMT group comprised parents who attended videoconference classes. The subject of the course was PMT. The six weekly 90-minute sessions of this course were held. The first session covered children’s psychology and familiarization with ADHD, its etiology, prognosis, and treatments. The second session focused on how to instruct the child. The third session aimed at strengthening communication with the child to achieve better obedience. The fourth and fifth sessions were about types of encouragement and discipline, respectively. The sixth session addressed the negative impact of certain situations on a child’s misbehavior (e.g., hunger and peer effect). At the beginning of each session, parents could ask questions about the previous sessions, and at the end of the session, they were guided on specific homework that they were supposed to send to the instructor for review.
Skype software (Skype Communications SARL), a web videoconferencing platform, provided the sessions. Parents were requested to download the application onto their laptops, desktop computers, and mobile devices, including tablets and smartphones. Parents logged on with the login information that the investigators had sent them. Parents were connected to several service providers’ Wi-Fi, 3G, and 4G mobile networks. Video conferencing and screen sharing were the information and communication technology modes employed. The latter was used to distribute multimedia files and PowerPoint presentations related to instructional materials and particular assignments like behavior charts. A messaging platform was used to create a messaging group. Every week, parents received reminders about upcoming sessions and homework assignments. They were also asked to share the home tasks with the group. Parents continued to receive routine care, visiting the hospital every four to eight weeks.
3.5. In-person Parent Management Training
The in-person PMT group comprised parents who attended face-to-face classes. The subject of the course was PMT. The six 90-minute sessions of this course were held once a week and covered the same topics as the videoconference classes. The sessions were held in Amin and Khorshid Hospital psychiatric clinics in Isfahan, Iran. The meetings were conducted by psychiatrists specializing in child and adolescent mental health following established guidelines outlined in evidence-based protocols (12, 13). Specifically, PMT sessions were likely facilitated by licensed psychologists, psychiatrists, or other qualified clinicians specializing in child and adolescent mental health. These professionals would have been trained in delivering PMT interventions according to recognized guidelines, such as those outlined in manuals or treatment protocols developed for PMT programs (12).
3.6. Randomization and Blinding
While this study was not conducted as a double-blind trial, measures were implemented to minimize potential bias and enhance the rigor of outcome assessment. Randomization was achieved using a computer-generated schedule with block randomization in a permuted block design, ensuring balanced assignment to the in-person and videoconference PMT groups. To further reduce bias, the therapists delivering the interventions were not involved in data analysis, and the statisticians analyzing the data remained blinded to participant group assignments. Given the use of parent-reported outcomes, standardized tools such as the Conners’ Parent Rating Scale (CPRS-48) and the Swanson, Nolan, and Pelham (SNAP-IV) Questionnaire were employed to structure and guide symptom assessment, aiming to minimize subjectivity in parental reports. These procedural steps contribute to the objectivity and reliability of the findings, addressing potential sources of bias inherent in non-double-blind designs.
3.7. Sample Size Estimation
The sample size for this study was estimated based on previous research by Chacko et al. (14), which examined the efficacy of parent training programs for children with ADHD. In their study, groups of 40 participants were sufficient to detect significant differences between intervention types. This sample size was calculated to provide 80% power to detect a medium effect size (Cohen’s d = 0.5) between the two groups, with a two-sided significance level of 0.05. Considering potential differences in effect sizes between in-person and videoconference delivery methods and accounting for an anticipated dropout rate of 10%, we determined a total targeted sample size of 90 participants (45 per group).
3.8. Measures
3.8.1. Conners’ Parent Rating Scale
The Persian version of the CPRS-48 was used to evaluate children’s behavioral issues. Conduct, social, psychosomatic, and anxiety problems are among the four categories it assesses. Every item was measured on a Likert scale of one to four, with 0 indicating never, 1 indicating sometimes, 2 indicating often, and 3 indicating very frequently. The final score of each type of behavioral issue was computed by averaging the scores of the related items. An anomaly was characterized as a score > 90th percentile for each dimension. In the psychometric properties of Persian ADHD diagnostics study, Cronbach’s alpha for the 48-item CPRS-48 was 91% (15).
3.8.2. Swanson, Nolan, and Pelham Questionnaire
The Persian version of SNAP-IV has 18 items graded on a 0 - 3 scale (16). The items are broken into two subscales: Attention deficit disorder (ADD) (nine items) and hyperactivity disorder (HD) (nine items). Calculating the subject’s score after the implementation is as follows: Each question is scored from 0 to 3, then the parent’s total score is divided by 18, and their score in each subtype is divided by 9. Inattention and hyperactivity/impulsivity items can be combined to get a “combined ADHD” score. While there are no universally agreed-upon cutoff scores for ADHD diagnosis, elevated scores on the inattention and hyperactivity/impulsivity scales, as well as on the total ADHD symptoms scale, may indicate a need for further assessment. Higher scores represent more troublesome symptoms (16). This tool was validated in Persian for the diagnosis of ADHD/hyperactivity in children aged 7 to 12. The total Cronbach’s alpha reliability calculation of 0.9 (16) revealed the questionnaire’s reliability.
3.9. Data Collection
Questionnaires were administered to the parents at three time points:
- Baseline: Prior to the start of the PMT program,
- Post-parent management training: Immediately after completing the 6-week PMT program,
- Follow-up: Two months after completing the PMT program.
For both the in-person and videoconference groups, parents completed the questionnaires (CPRS-48 and SNAP-IV) during scheduled assessment sessions. These sessions were facilitated by research team members who were blinded to group assignments. Parents filled out paper questionnaires during their clinic visits for the in-person group. For the videoconference group, electronic versions of the questionnaires were sent via a secure online platform, which parents completed during a scheduled video call with a research team member available to answer any questions.
3.10. Statistical Analysis
SPSS statistics software (IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp) was used for statistical analyses. The descriptive statistics of continuous data were reported as mean ± SD, and categorical variables were reported as count and percentages. The categorical variables were compared using the chi-square test. The normality assumption of each variable was assessed using various methods, including the Shapiro-Wilk tests and an examination of skewness and kurtosis. Based on the results of the Shapiro-Wilk tests (non-significant P-values) or the evaluation of skewness and kurtosis (absolute values of skewness < 2 and absolute values of kurtosis < 7), determinations were made regarding the normality distribution of each variable (17). The independent samples t-test was used to compare continuous variables between the videoconference PMT and in-person PMT groups (between-group comparisons). We employed a repeated measures analysis of variance to analyze the changes in each parameter within and between the groups over the study period (baseline, post-intervention, and 2-month follow-up).
4. Results
4.1. Participant Demographics
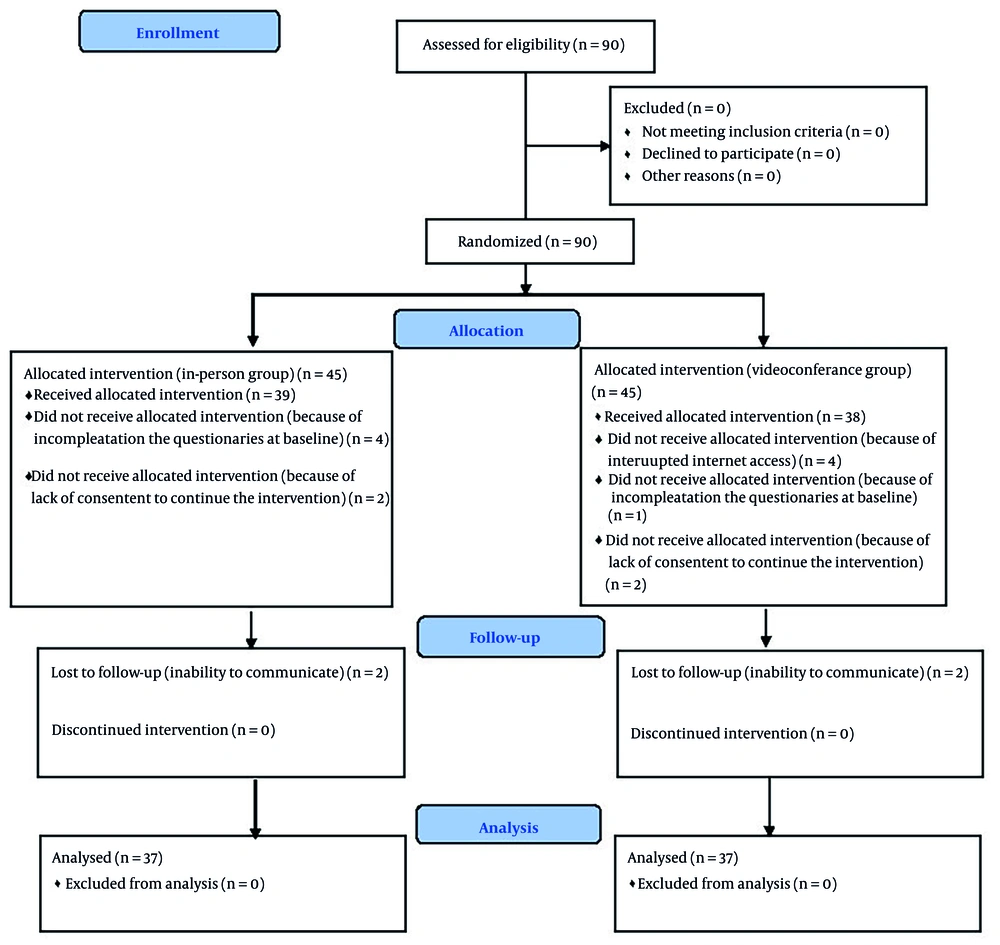
Initially, 90 parents enrolled; 16 were excluded because of interrupted internet access, incompletion of the questionnaires at baseline, lack of consent, and lost follow-up. Finally, seventy-four parents were enrolled in the analysis. To assess the adequacy of our statistical power with the final sample size (37 participants per group), we conducted post-hoc power analyses. For the in-person PMT group, the analysis revealed an observed power of 0.999. The videoconference PMT group demonstrated an observed power of 0.832. Both measures exceeded the conventional 0.80 threshold for adequate statistical power, indicating that the study maintained sufficient power to detect significant effects despite the smaller-than-planned sample size. The high observed power values, combined with significant effects and substantial effect sizes, support the robustness of our statistical findings.
Among enrolled participants, 63 (85.1%) were females and 11 (14.9%) were males. There was no significant difference in parental participation patterns between the in-person and videoconference groups (P = 0.6). The mean ± SD age of parents was 8.92 ± 1.57 for the in-person PMT and 8.76 ± 1.79 for the videoconference PMT group. There were no significant differences regarding age between the two groups (P = 0.68). Also, the two groups had no significant differences in father’s (P = 0.22) and mother’s ages (P = 0.67) (Table 1). The study’s flowchart is shown in Figure 1.
| Variables | Training Type | P-Value | |
|---|---|---|---|
| In-person | Videoconference | ||
| Participated parents | 0.6 b | ||
| Both father and mother | 11 (30) | 8 (22) | |
| Only mother | 26 (70) | 29 (78) | |
| Only father | 0 | 0 | |
| Age | 8.92 ± 1.57 | 8.76 ± 1.79 | 0.68 c |
| Father’s age | 41.97 ± 3.99 | 40.84 ± 3.85 | 0.22 c |
| Mother’s age | 36.7 ± 3.36 | 36.38 ± 3.15 | 0.67 c |
| Father’s education | 0.12 b | ||
| Below diploma | 11 (29.7) | 4 (10.8) | |
| Diploma | 9 (24.3) | 10 (27) | |
| Higher than a diploma | 17 (45.9) | 23 (62.2) | |
| Mother’s education | 0.03 b | ||
| Below diploma | 7 (18.9) | 3 (8.1) | |
| Diploma | 14 (37.8) | 7 (18.9) | |
| Higher than a diploma | 16 (43.2) | 27 (73) | |
a Values are expressed as No. (%) or mean ± SD.
b P-value is according to the chi-square test.
c P-value is according to the t-test.
4.2. Effectiveness of Parent Management Training on the Conner’s Parent Rating Scale Scores
4.2.1. Conduct Problem
The in-person and videoconference PMT groups showed comparable mean scores at baseline (P = 0.464). While the in-person group demonstrated a decrease in mean scores post-PMT and at follow-up, these changes were not statistically significant compared to the videoconference group (P > 0.05). Significant within-group changes were observed over time for in-person (P < 0.001, effect size = 0.48) and videoconference PMT (P < 0.001, effect size = 0.35) groups, with a significant interaction between time and group effects (P < 0.001, effect size = 0.12).
4.2.2. Social Functioning Problem
Baseline mean scores were similar between the groups (P = 0.384). However, significantly greater improvements were observed in post-PMT (P = 0.021, effect size = 0.55) and follow-up (P = 0.009, effect size = 0.63) assessments for the in-person group compared to the videoconference group. Significant within-group changes occurred over time only for in-person PMT (P < 0.001, effect size = 0.39). Also, time and group have a significant interaction effect (P < 0.001, effect size = 0.17).
4.2.3. Psychosomatic Problem
No significant difference in baseline scores was observed between the groups (P = 0.197). Significant differences favoring the in-person compared to videoconference PMT emerged at follow-up (P = 0.020, effect size = 0.55). Significant within-group changes occurred over time only for in-person PMT (P < 0.001, effect size = 0.45). The interaction between time and group was significant (P < 0.001, effect size = 0.18).
4.2.4. Anxiety Problem
Baseline scores were comparable between groups (P = 0.156). Post-PMT and follow-up assessments did not reveal significant differences in mean scores between groups (P > 0.05). Significant within-group changes were observed over time for in-person (P < 0.001, effect size = 0.30) and videoconference PMT (P = 0.036, effect size = 0.09) groups, with no significant interaction effect between time and group (P = 0.014, effect size = 0.06).
4.2.5. Total Scores
The in-person group exhibited significantly lower total scores at post-PMT (P = 0.045, effect size = 0.48) and follow-up (P = 0.017, effect size = 0.57) compared to the videoconference group. Only the videoconference PMT group demonstrated significant within-group changes over time (P = 0.004, effect size = 0.14). There was no significant interaction effect between time and group (P = 0.655, effect size = 0.01) (Table 2).
| Scales | In-person | Videoconference | P-Value (Effect Size) b | P-Value (Effect Size) c |
|---|---|---|---|---|
| Conduct, baseline | 61.62 ± 10.29 | 59.78 ± 11.18 | 0.464 (0.17) | < 0.001 (0.12) |
| Conduct, post-PMT | 55.24 ± 5.48 | 58.92 ± 11.95 | 0.095 (0.39) | |
| Conduct, follow up | 51.19 ± 8.07 | 55.27 ± 9.45 | 0.05 (0.46) | |
| P-value (effect size) d | < 0.001 (0.48) | < 0.001 (0.35) | ||
| Social, baseline | 71.46 ± 14.11 | 68.65 ± 13.49 | 0.384 (0.20) | < 0.001 (0.17) |
| Social, post-PMT | 61.78 ± 8.52 | 67.97 ± 13.48 | 0.021 (0.55) | |
| Social, follow up | 60.59 ± 10.74 | 67.92 ± 12.49 | 0.009 (0.63) | |
| P-value (effect size) d | < 0.001 (0.39) | 0.638 (0.01) | ||
| Psychosomatic, baseline | 67.92 ± 14.68 | 64.08 ± 10.28 | 0.197 (0.16) | < 0.001 (0.18) |
| Psychosomatic, post-PMT | 58.73 ± 9.43 | 62.68 ± 9.79 | 0.082 (0.41) | |
| Psychosomatic, follow up | 56.73 ± 10.77 | 62.86 ± 11.39 | 0.02 (0.55) | |
| P-value (effect size) d | < 0.001 (0.45) | 0.282 (0.03) | ||
| Anxiety, baseline | 56.19 ± 8.76 | 53.32 ± 8.42 | 0.156 (0.33) | 0.014 (0.06) |
| Anxiety, post-PMT | 51.27 ± 5.65 | 51.54 ± 7.84 | 0.865 (0.04) | |
| Anxiety, follow up | 49.59 ± 8.09 | 51.05 ± 9.17 | 0.47 (0.17) | |
| P-value (effect size) d | < 0.001 (0.30) | 0.036 (0.09) | ||
| Total, baseline | 57.3 ± 8.45 | 62.89 ± 11.71 | 0.021 (0.55) | 0.655 (0.01) |
| Total, post-PMT | 56.89 ± 7.34 | 61.65 ± 12.04 | 0.045 (0.48) | |
| Total, follow up | 54.35 ± 9.83 | 60.54 ± 11.88 | 0.017 (0.57) | |
| P-value (effect size) d | 0.118 (0.06) | 0.004 (0.14) |
Abbreviation: PMT, parent management training.
a Values are expressed as No. (%) or mean ± SD.
b P-value is derived from the t-test for testing between-group effects, and the effect size is based on Cohen’s d.
c P-value is derived from the repeated measures model for the interaction of time and group effect, and the effect size is calculated using partial eta squared.
d P-value is derived from the repeated measures model for testing within-group effects, and the effect size is calculated using partial eta squared.
4.3. Effectiveness of Parent Management Training on the Swanson, Nolan, and Pelham Questionnaire Scores
4.3.1. Attention Deficit Disorder
Baseline mean scores for ADD were similar between the in-person and videoconference groups (P = 0.47). There were no significant differences in mean scores between the post-PMT and follow-up groups (P > 0.05). Significant within-group changes were observed over time for in-person (P < 0.001, effect size = 0.38) and videoconference PMT (P < 0.001, effect size = 0.39) groups, with no significant interaction effect between time and group (P = 0.987, effect size = 0.0).
4.3.2. Hyperactivity Disorder
Baseline mean scores for HD were significantly lower in the in-person group (7.73 ± 3.61) compared to the videoconference group (9.51 ± 3.71) (P = 0.04). Significant differences between the in-person group compared to videoconference PMT were observed only at follow-up (5.3 ± 2.9 vs. 7.03 ± 3.18, P = 0.017, effect size = 0.57). Since the in-person group had a lower mean HD score compared to the videoconferencing group at baseline, it is possible that this initial difference, rather than the intervention itself, contributed to the observed superior outcomes for the in-person group at the follow-up assessment. Also, considering effect size, the superiority of in-person PMT is notable in post-follow-up time. However, caution should be taken when interpreting the study’s findings. Significant within-group changes were observed over time for in-person (P < 0.001, effect size = 0.37) and videoconference PMT (P < 0.001, effect size = 0.28) groups, with no significant interaction effect between time and group (P = 0.851, effect size = 0.01).
4.3.3. Attention Deficit Hyperactivity Disorder
Baseline mean scores for ADHD were similar between the in-person and videoconference PMT groups (P = 0.764). There were no significant differences in mean scores between the groups post-PMT and at follow-up (P > 0.05). Significant within-group changes were observed over time for in-person (P < 0.001, effect size = 0.29) and videoconference PMT (P = 0.01, effect size = 0.13) groups, with no significant interaction effect between time and group (P = 0.467, effect size = 0.01) (Table 3).
| Variables | In-person | Videoconference | P-Value (Effect Size) b | P-Value (Effect Size) c |
|---|---|---|---|---|
| ADD, baseline | 15.32 ± 5.6 | 16.3 ± 5.91 | 0.47 (0.17) | 0.987 (0.00) |
| ADD, post-PMT | 13.73 ± 5.29 | 14.76 ± 5.9 | 0.433 (0.18) | |
| ADD, follow up | 12.11 ± 4.91 | 13.19 ± 5.13 | 0.357 (0.21) | |
| P-value (effect size) d | < 0.001 (0.38) | < 0.001 (0.39) | ||
| HD, baseline | 7.73 ± 3.61 | 9.51 ± 3.71 | 0.04 (0.49) | 0.851 (0.01) |
| HD, post-PMT | 7 ± 3.37 | 8.49 ± 3.59 | 0.071 (0.43) | |
| HD, follow up | 5.3 ± 2.9 | 7.03 ± 3.18 | 0.017 (0.57) | |
| P-value (effect size) d | < 0.001 (0.37) | < 0.001 (0.28) | ||
| ADHD, baseline | 4.43 ± 3.03 | 4.65 ± 3.15 | 0.764 (0.07) | 0.467 (0.01) |
| ADHD, post-PMT | 3.68 ± 2.51 | 4.27 ± 2.92 | 0.351 (0.22) | |
| ADHD, follow up | 3.22 ± 2.58 | 3.78 ± 2.8 | 0.368 (0.67) | |
| P-value (effect size) d | < 0.001 (0.29) | 0.01 (0.13) |
Abbreviations: ADD, attention deficit disorder; PMT, parent management training; HD, hyperactivity disorder; ADHD, attention deficit hyperactivity disorder.
a Values are expressed as No. (%) or mean ± SD.
b P-value is derived from the t-test for testing between-group effects, and the effect size is based on Cohen’s d.
c P-value is derived from the repeated measures model for the interaction of time and group effect, and the effect size is calculated using partial eta squared.
d P-value is derived from the repeated measures model for testing within-group effects, and the effect size is calculated using partial eta squared.
Overall, both in-person and videoconference PMT modalities showed comparable effectiveness in addressing ADD and ADHD, while in-person PMT demonstrated superior outcomes in managing HD, particularly at the follow-up assessment.
5. Discussion
The comparison between in-person and videoconference PMT revealed several key findings. While both modalities demonstrated comparable effectiveness in addressing ADD and ADHD, in-person PMT exhibited superior outcomes in managing HD, particularly at follow-up assessments. Additionally, the in-person group showed significantly greater improvements post-PMT and at follow-up compared to the videoconference group in terms of social problems. However, there were no significant differences between the two modalities in managing conduct problems, psychosomatic issues, and anxiety. Overall, in-person PMT appeared to offer advantages in certain areas, emphasizing the importance of considering delivery methods when implementing behavioral interventions. Also, the observed similarities in symptom improvement between in-person and videoconference PMT emphasize the importance of tailoring educational approaches to the individual needs of ADHD children. The flexibility of videoconference education may offer benefits in accommodating different learning styles and preferences, while the structure of in-person education may provide essential environmental cues and immediate feedback (18).
Based on research conducted on a web portal videoconference PMT for ADHD care, it was found that providing network-based education and nursing education to families with ADHD children resulted in significant improvement in symptom ratings from parents. Another research discovered that the combination of network-based education, nursing education, and pharmacological therapy for ADHD families resulted in a more favorable therapeutic outcome in terms of the attention report of ADHD children’s parents compared to families without remote assistance (9, 10). Our study results were consistent with the previous study on the same topic, which demonstrated that videoconferencing had the same effect as face-to-face groups in improving scores on the Vanderbilt Rating Scale for inattentive, hyperactive, oppositional, behavior, and anxiety symptoms (19). Similarly, in another study comparing telegroup versus in-person parent behavior management training for ADHD children, there were no significant differences in improving the inattention symptoms (parent) and hyperactivity/impulsivity (parent) symptoms throughout the study between the two groups. Also, similar to our study, parents in telegroup had a significantly higher education than those in the in-person group (8). Furthermore, research evaluating the impact of online parent training (OPT) on school-aged children diagnosed with ADHD discovered that the OPT program yielded positive results in reducing inattentive symptoms, enhancing executive function, addressing learning difficulties, and alleviating parental concerns (20). Another study on disruptive behavior symptoms in ADHD children in line with our study results demonstrated that parent training, whether provided in-person or virtually, was successful in lowering ADHD symptoms (21).
Our study aligns with previous research, highlighting the comparable effectiveness of videoconference education through videoconferencing and telegroup sessions to traditional face-to-face videoconference PMTs. This consistency across studies reinforces the notion that videoconference education, when properly implemented, can be a valuable and accessible tool for parents seeking support in managing ADHD-related challenges.
Several limitations must be acknowledged in the interpretation of our findings. The post-hoc power analysis indicated that the study lacked sufficient power to detect between-group differences, with achieved power varying from 0.49 to 0.73 for significant outcome measures. To attain sufficient statistical power (80%), sample sizes ranging from 90 to 150 participants would have been necessary, contingent upon the specific outcome measure. This limitation may have hindered our capacity to identify potentially significant differences among intervention modalities. The study’s generalizability may be constrained by its execution in a specific geographical area (Isfahan, Iran) characterized by distinct healthcare infrastructure and cultural context. Third, reliance on parent-reported outcome measures may introduce measurement bias, given that parents were not blinded to their intervention group assignment. The follow-up period of two months may be insufficient to assess long-term treatment effects or the sustainability of improvements. Fifth, variability in adherence to videoconference sessions, quality of internet connectivity, and technical proficiency among participants may have affected treatment fidelity and outcomes in the videoconference group. Sixth, although randomization was employed, the initial disparity in hyperactivity scores between groups may have impacted our results in this area. The exclusion of children with comorbid ODD or conduct problems may restrict the generalizability of our findings to the wider ADHD population, in which these comorbidities are prevalent. Future research must address these limitations by utilizing larger sample sizes, extending follow-up periods, employing objective outcome measures, and incorporating more diverse populations to enhance the evidence base for videoconference-delivered PMT interventions.
5.1. Conclusions
This study demonstrates the comparable efficacy of in-person and videoconference PMT in addressing various ADHD-related challenges. While both modalities show significant improvements, the nuanced strengths of each underscore the importance of tailored approaches. These findings advocate for a blended strategy, combining the flexibility of videoconference education with the structured environment of in-person sessions for optimal support in managing ADHD symptoms. Future research should explore the mechanisms underlying the superior outcomes of in-person PMT for managing HD and investigate potential moderators of treatment effectiveness. Longitudinal studies with extended follow-up periods and comparative effectiveness research on different PMT delivery formats could provide valuable insights into optimizing videoconference PMT strategies for ADHD management.