1. Background
According to a World Health Organization (WHO) report (1), a total of 970 million people globally were living with a mental disorder in 2013, and there has been a substantial increase in depressive and anxiety disorders due to the COVID-19 pandemic (2). Moreover, suicide accounts for 1 in 100 deaths globally, with a reported increase in the suicide rate in recent years (3). In Iran, a middle-income country in the Middle East, approximately 24% of adults suffer from one or more mental disorders in a 12-month period (4), and recent surveys have shown a significant increase in prevalence estimates during the COVID-19 pandemic (5). Promoting mental health and suicide prevention is considered an international priority, and there is an urgent need for the provision of available and accessible mental health services for individuals experiencing mental distress, especially during a crisis.
Telephone crisis intervention services or hotlines are widely used for mental health support across different populations (6). Initially, the purpose of establishing crisis hotlines was suicide prevention. Later, many crisis hotlines were frequently contacted by individuals who were not at immediate risk of suicidal attempts but were in acute psychological distress (7).
Crisis hotlines are popular mainly because of their low costs, lack of professional expertise requirements, and accessibility. Although the direct effect of these hotlines on reducing the suicide rate is mixed, many studies agree on their significant impact on decreasing distress, anxiety, confusion, loneliness, anger, and suicidal thoughts (8-10). Moreover, hotlines can significantly reduce medical costs related to mental health problems, psychiatric hospitalization, and family burden (11, 12).
However, psychiatric crisis hotlines are underdeveloped and scarcely studied in low- and middle-income countries (LMICs). To our knowledge, no study has been conducted to evaluate the implementation of a psychiatric crisis hotline in Iran.
2. Objectives
We aimed to establish a crisis hotline in Iran that is freely accessible to people affected by a mental health crisis and evaluate the outcomes of its implementation during the pandemic. The study's specific aims were as follows: (A) To develop and implement a psychiatric crisis hotline in Roozbeh Hospital and (B) to evaluate the implementation and health outcomes, including (1) the change in callers' distress, aggression, suicidal risk, and need for referral between baseline and follow-up call, one to two weeks later; (2) the satisfaction with the service; and (3) the proportion of mental health care utilization one to two weeks after the baseline call.
3. Methods
In service implementation research, we took the following steps to achieve the main aims of the study:
3.1. Development and Implementation
First, we conducted a rapid needs assessment based on available data from surveys and national and international sources. Then, we developed the initial design of the service model based on published studies, guidelines, and feasibility of implementation in our setting. The proposed model underwent review and discussion by a group of psychiatry experts, hospital directors, and service providers, and revisions were made according to their feedback. Several software development companies capable of assisting with call management were evaluated based on factors such as service availability across broad areas of the country, service cost, and the ability to transfer calls to counselors.
The service model included telephone crisis assessment and intervention. Crisis counselors provided techniques such as active listening, empathy, problem-solving, psychoeducation, anger management, relaxation techniques, and reassurance. Callers were advised to seek appropriate health and emergency services if needed. Twelve psychiatry residents from Roozbeh Hospital served as counselors, receiving calls. They underwent training in a workshop covering topics including crisis evaluation and crisis management techniques for telephone crisis response services. Weekly supervision was provided to counselors, a sample of recorded calls was reviewed, and feedback was provided to service providers.
For technical support and call management, we selected a telecommunications company capable of offering the service to a broader range of people across the country at minimal cost, while providing an easily operated and accessible service. The company facilitated call registry, recording, and transferring capabilities for the team.
Several studies have indicated that peak usage in many crisis lines occurs between 2 pm and 12 am (13, 14). Therefore, considering the limited available resources, we designated the working hours of our hotline service from 2 pm to 12 am. The service was entirely free of charge, with callers only responsible for their phone bills. We promoted the hotline to the public through posters and flyers at Roozbeh Hospital and social media platforms.
3.2. Outcome Evaluations
The data collection period for this study spanned six months (January to June 2022), during which all individuals meeting the inclusion criteria were recruited. Inclusion criteria for data collection were: (1) Receiving calls to the hotline for a crisis and (2) providing consent to provide data for evaluation. Exclusion criteria included: (1) Individuals speaking languages other than Farsi, (2) low-quality calls that were incomplete or disconnected before assessment and intervention completion, and (3) calls lasting less than 2 minutes, which did not allow for crisis assessment (15).
For callers who consented to evaluation, counselors recorded the following information immediately after crisis intervention in the baseline call: Age, sex, education, marital status, presence and severity of suicidal ideations, aggression, previous history of psychiatric illnesses, and need for referral. A follow-up evaluation was conducted one to two weeks after the initial call by an independent psychology research assistant, separate from the initial counselors. We opted for an online data collection service (Porsline: https://survey.porsline.ir) to facilitate data collection during both baseline and follow-up calls. The evaluated outcomes are categorized into implementation and health outcomes:
3.3. Implementation Outcomes
An electronic call registry recorded the number of incoming calls daily. Additionally, the number and proportion of calls answered by the receiving counselor and lasting more than 2 minutes were obtained from the registry. Participants' satisfaction was measured using a researcher-developed questionnaire, which included a Likert scale question asking, "Please let us know how satisfied you are with the service you have received?" (ranging from low to high), at the end of the follow-up call.
3.4. Health Outcomes
The severity of callers' distress and their perceived ability to control it were evaluated using the Distress Thermometer tool, employing two Likert scale questions: "To what degree are you upset?" and "To what degree do you feel you can control the situation?" Distress levels were assessed at three points: The beginning and end of the initial call and the follow-up call.
Suicide risk was assessed using modified questions from the IranMHS study (16), and the severity of suicide risk was judged by the counselor (psychiatry residents). This assessment was conducted immediately after the baseline call and during the follow-up call. Similarly, the degree of aggression was evaluated based on questions from the IranMHS and the subjective judgment of the counselor, with reassessment during the follow-up call. Additionally, the utilization of health and emergency services was queried during the follow-up call.
3.5. Data Analysis
Quantitative data were analyzed using STATA (version 14). Descriptive statistics summarized the demographic and clinical characteristics of the outcome evaluation sample. The Wilcoxon single-rank test, suitable for paired ordinal data, was used to compare distress levels at the beginning and end of calls. Linear regression analyses were also conducted to explore factors associated with changes in distress levels. All statistical tests were two-sided, with a significance level set at P < 0.01.
4. Results
4.1. Implementation Outcomes
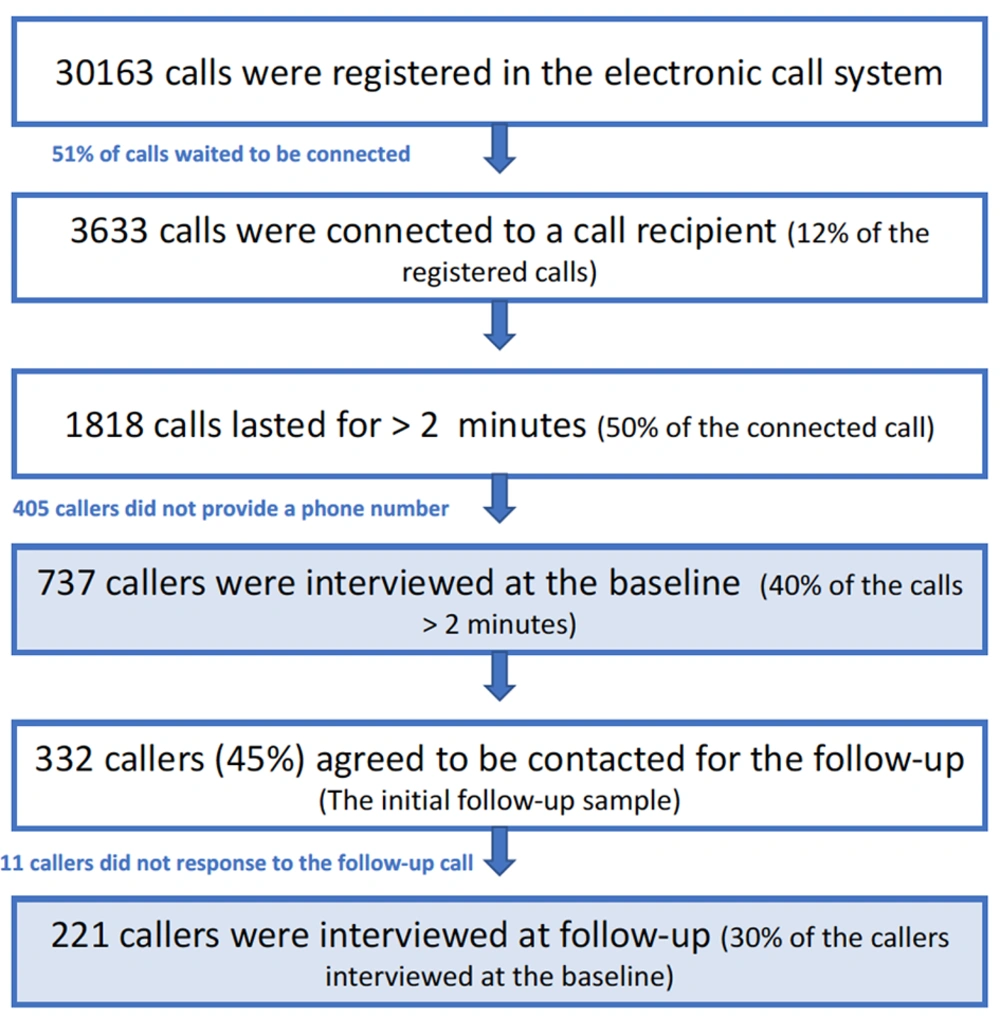
Throughout the 6-month study period, the electronic call system registered 30163 calls. Among these, 3633 calls were connected to a call recipient, and service was provided. Of these, 1818 calls lasted longer than 2 minutes. Refer to Figure 1 for detailed participant numbers at each stage.
Among the subjects interviewed at follow-up (N = 221), 186 (84.2%, 95% CI [78.6, 88.7]) expressed high satisfaction with the hotline service. Of these individuals, 206 (93.2%, 95% CI [89.0, 96.1]) indicated they would recommend the service to others in crisis situations. Nearly two-thirds (67%, 95% CI [63.5, 70.4]) of the callers reported learning about the hotline through social media platforms, specifically Instagram and Telegram.
4.2. Health Outcomes
Out of 737 callers (523 females, age range 11 - 65 years old; mean = 25.1, SD = 9.3) who consented to participate in the research assessments, 332 provided a phone number for the follow-up call (initial follow-up sample). Table 1 presents the demographic and clinical characteristics of the callers at the baseline call. There were no significant differences between the initial follow-up sample and those who refused to provide a phone number (N = 405) across various demographic and mental health variables.
| Variables | Baseline | Successful Follow-up |
|---|---|---|
| Sex (female) | 523 (71.0) | 151 (68.3) |
| Young age group (< 25) | 395 (53.6) | 107 (48.4) |
| Marital status (single) b | 465 (63.1) | 130 (58.8) |
| Education (diploma or less) b | 347 (47.1) | 90 (40.7) |
| Student (high school/university) b | 215 (29.2) | 51 (23.1) |
| Employed b | 105 (14.2) | 35 (15.8) |
| With suicide ideations | 306 (41.5) | 125 (56.6) |
| With moderate-to-severe suicidal risk | 277 (37.5) | 87 (39.3) |
| With aggression | 69 (9.4) | 17 (7.7) |
| History of a psychiatric illness | 281 (38.1) | 97 (43.9) |
| Referred to: | ||
| Outpatient clinic | 491(66.6) | 151 (68.3) |
| Emergency department | 146 (19.8) | 47 (21.3) |
| Crisis management service | 12 (1.6) | 6 (2.7) |
Demographic and Clinical Features of Subjects at Baseline (N = 737) and Follow-Up Calls (N = 221) a
From the initial follow-up sample (N = 332), 111 individuals could not be re-interviewed in the follow-up calls due to: (1) Incorrect phone number (N = 25), (2) failure to answer the phone (N = 79), and (3) refusal to be interviewed over the phone (N = 7). Ultimately, 221 participants were re-interviewed at follow-up. We compared those who were successfully contacted (N = 221) with unsuccessful follow-ups (N = 111) from the initial follow-up sample regarding various demographic and mental health variables. There were no significant differences in these parameters, except for suicidal ideations; the proportion of subjects with suicidal ideation was significantly lower in the group with successful follow-up calls than in the group with unsuccessful follow-up calls (59.2% vs. 71.2%, respectively; X2 (1, N = 221) = 6.66, P = 0.01).
Among the baseline sample, 277 callers (37.5%) (95% CI [34.1, 41.1]) were at moderate-to-high risk of suicide. Most subjects were referred to either an outpatient clinic or an emergency department at baseline and follow-up (Table 1).
At the baseline call, we observed a significant decrease in the level of distress experienced from the beginning to the end of the call, using the Wilcoxon signed-rank test (z = 23.47, P < 0.001). We also noted a significant difference in the level of experienced distress between the beginning of the baseline and the follow-up call (z = 11.51, P < 0.001). Considering the subgroup with suicidal ideation, there was a significant difference between the level of distress experienced at the beginning of the baseline and the beginning of the follow-up calls (z = 9.30, P < 0.001).
We conducted a series of linear regressions to examine the factors associated with the degree of change in distress. Among the sociodemographic and clinical variables, only the caller’s sex was associated with the degree of distress reduction between the beginning and the end of the baseline call, with female callers experiencing a higher degree of distress reduction (beta = 0.49; P = 0.002). Regarding the reduction in distress from baseline to follow-up, suicidal ideation (beta = 1.16; P = 0.003) and moderate-to-high suicide risk (beta = 1.43; P < 0.001) were observed.
We compared the odds of reporting suicidal ideations, moderate-to-high suicide risk, aggression, and the need for referral between the baseline and follow-up calls. All these indicators were significantly lower in the follow-up (Table 2). Among the 204 follow-up subjects referred to outpatient settings, hospitals, or emergency departments during their baseline call, 98 subjects (48%, 95% CI [0.410, 0.551]) completed the referral. The majority of these individuals (N = 80) received a mental health visit at a clinic, while only three were hospitalized.
| Variables | Baseline call | Follow-up call | Z-Value | P-Value |
|---|---|---|---|---|
| Suicidal ideations | 125 (56.6) | 47 (21.3) | 7.38 | < 0.001 |
| Moderate-to-high suicide risk | 87 (39.3) | 32 (14.5) | 5.76 | < 0.001 |
| Aggression | 17 (7.7) | 42 (19) | -3.51 | < 0.001 |
| Referred | 204 (92.3) | 161 (72.8) | 6.14 | < 0.001 |
Odds of Suicidal Ideations, Suicide Risk, Aggression, and Need for a Referral at the Baseline and Follow-Up for the Follow-up Samples (N = 221) a
5. Discussion
In this study, we aimed to develop and evaluate a hotline for psychiatric crisis intervention in Iran. To our knowledge, this is the first mental health crisis hotline studied and available to the general population in Iran. Additionally, this hotline can be considered one of the pioneering studies of hotlines in Southwest Asian countries. Previous research (e.g., (17)) has highlighted crisis hotlines as essential first-line mental health services for many individuals, making them crucial in public health interventions. However, there is a limited body of research on these services in LMICs (13).
Out of the 30,163 calls logged on the hotline, 51% remained on hold awaiting connection, and 3,633 calls were answered. The primary reason for this drop-off may be the limited number of counselors available to handle the overwhelming call volume. Other factors contributing to this dropout include a lack of awareness about the hotline's purpose and technical difficulties. Watson and Spiteri (18) reported a similar observation, with 47% of their received calls being responded to within 90 seconds.
The average age of hotline callers was 25.1 years, with 51.7% falling within the 15 - 24 age range. This age demographic is younger compared to reports from Shaw and Chaing (19) regarding the suicide hotline in Taiwan and the UK Department of Health (20), which noted that individuals under 25 years old were less likely to utilize the hotline. Our findings align with other studies, such as those by Meehan and Broom in South Africa (10, 21). Iran's predominantly young population may account for the youthful age of our hotline callers. It's noteworthy that no specific hotline in Iran caters specifically to teenagers and young adults, although there is a counseling line available for adolescents (Sedaye Yara, https://www.irsprc.org). Importantly, we primarily promoted our hotline through social media platforms like Telegram, Instagram, and Twitter, rather than utilizing television and newspapers. In Iran, the majority of social media users are teenagers and young adults, aligning with the young age composition of our hotline callers, who are more active on social media platforms.
We observed lower levels of distress, suicidal ideation, and aggression in the follow-up calls. Approximately 48% of subjects interviewed during the follow-up session reported adhering to the suggested referral. This finding is consistent with Hoffberg et al.'s (22) observation that 41.9% of callers completed their referrals.
A notable observation among subjects agreeing to follow-up interviews was the lower proportion of suicidal ideation in the subgroup that completed the follow-up. This could be attributed to individuals with suicidal ideation experiencing more severe depressive symptoms, including hopelessness and reduced motivation to respond to follow-up calls. Similar to our findings, Hoffberg et al. (22) noted that most suicidal callers do not follow through with referrals, highlighting the necessity for active follow-up by mental health providers for individuals with suicidal ideations.
The utilization of diverse media plays a crucial role in advancing mental health and suicide interventions (10). The reception of calls from various regions across the country provides evidence of the public's accessibility to the hotline. Despite partial restrictions on internet access, particularly social media, in Iran, many callers reported learning about the hotline through social media platforms.
Financial constraints and insufficient operational resources emerged as the primary barriers to the hotline's development. The unexpectedly high call volume made service planning challenging. While not all callers were in immediate danger of suicide or aggression, many sought information about the hotline. This overwhelming demand for services complicates the timely provision of assistance to individuals at risk. Furthermore, training and retaining skilled counselors presented significant challenges due to the substantial time and resource commitments involved.
This study has several limitations, including its nonrandomized design, lack of a matched control group, modest sample size, and short follow-up intervals. Addressing these limitations underscores the necessity for randomized clinical trials to evaluate hotline implementation outcomes in low- and middle-income countries (LMICs). However, ethical considerations make it challenging to include a control group deprived of care. Additionally, it's important to note that we primarily relied on short, subjective outcomes due to the brevity of calls. Previous studies have employed objective and expert evaluations, such as live monitoring of calls to different hotlines (23).
5.1. Conclusions
In conclusion, despite the barriers, callers positively received the hotline, as evidenced by the high call volume and reported satisfaction. Follow-up calls revealed reductions in experienced distress levels, suicide risk, and the need for further referrals, underscoring the importance of crisis hotlines as primary mental health support services. These findings support the feasibility and acceptability of implementing hotlines in LMICs during pandemics. However, there remains a need for well-designed randomized controlled studies.