1. Background
Mental health issues are rising among global healthcare professionals due to factors such as high workloads, long shifts, emotional investment, competitive environments, and high-stress conditions (1, 2). Medical, dental, and pharmacy students are particularly affected, with high rates of mental health problems reported worldwide (2-5).
Symptoms of depression and anxiety are prevalent among these students:
• Approximately 27.2% of medical students exhibit symptoms of depression, and 25.7% suffer from anxiety (4).
• During the COVID-19 pandemic, 37% of dental students experienced depression (6).
• Anxiety and depression were reported among 30% and 22% of pharmacy students, respectively (2, 5).
Suicide attempts are a significant concern, with the risk among medical doctors being 5 to 7 times higher than that of the general population (7-9). Suicidal thoughts and attempts are reported in 17% and 1% of medical doctors, respectively (8).
In Iran, although limited studies have been conducted, high levels of stress, anxiety, depression, and suicidal thoughts have been reported among medical, dental, and pharmacy students (10-12). Reasons for suicides among young medical students and residents include long working hours, lack of sleep, difficult exams, low income, financial problems, and being away from families (13, 14). Despite the urgent need for interventions, due to the social stigma stemming from Iranian culture, medical students often avoid seeking help, especially from mental health professionals (13, 14).
2. Objectives
This study aims to estimate the prevalence of stress, anxiety, depression, and suicide-related thoughts and behaviors, and identify related risk factors among medical, dental, and pharmacy students at Shiraz University of Medical Sciences (SUMS), one of the largest and most important medical universities in the southwest of Iran, using an online survey-based approach. Chi-square and linear regression models were used to analyze the data.
3. Methods
3.1. Study Design and Participants
This cross-sectional study was conducted from November 2022 to December 2022. The study population consisted of medical, dental, and pharmacy students. Students who were willing to participate were included. Data were collected via a web-based structured questionnaire designed by a software engineer. The online version of the questionnaire was distributed to the social network groups of all semesters of medical, dental, and pharmacy students, and data collection continued until students from different majors and semesters had completed the questionnaire to ensure the representativeness of the study. In total, 292 students participated in the study. On the first page of the questionnaire, the aims of the study, as well as data protection and confidentiality, were outlined. All participants provided their consent to participate in the study by clicking a specific tab before responding to the questions. Participants who agreed to take part consented to anonymous data collection. Questionnaires that were filled out incompletely or by individuals who were no longer students at SUMS were excluded from the study. This study was reviewed and approved by the ethics committee under code number IR.SUMS.REC.1401.687.
3.2. Instruments
Background Information: Data on gender, age, field of study, semester, marital status, and place of residence were collected. Students were asked to rate their interest in courses and the perceived difficulty of courses on a scale from one to ten. Additionally, data on the average hours spent in academic or clinical settings during the past month, visits to mental healthcare providers during the past year, history of previously diagnosed psychiatric illness, history of chronic medical conditions, and family history of psychiatric illness were also collected.
Socioeconomic Status (SES) Questionnaire: The standard SES Questionnaire was used in this study. This questionnaire assesses socioeconomic status by evaluating the tools available in the household (including television, washing machine, etc.) as well as the level of infrastructure of the household's place of residence for each person in the family. The SES Questionnaire categorizes socioeconomic status into five categories, ranging from 'very low' to 'very high.' The validity and reliability of the SES questionnaire have been previously confirmed by Sartipi et al. in the Iranian population, with an acceptable intraclass correlation coefficient of 0.87 (15).
3.2.1. Depression, Anxiety, and Stress Scales-21
The Depression, Anxiety, and Stress Scales-21 (DASS-21) questionnaire is a self-report tool with 21 questions that measures stress, anxiety, and depression in students. It has three sections: Depression (assessing mood, motivation, and self-esteem), stress (measuring nervous tension and irritability), and anxiety (focusing on arousal, panic, and fear) (16). Each section contains seven questions, which are answered on a Likert scale. The severity of stress, anxiety, and depression is determined based on the work of Lovibond, S and Lovibond, P (16). The Farsi version of the DASS-21 used in Iran has confirmed reliability, with Cronbach’s α of 0.79 for anxiety, 0.91 for stress, and 0.93 for depression (17).
3.2.2. Beck Scale for Suicidal Thoughts
The Beck Scale for suicidal thoughts (BSSI) questionnaire, consisting of 19 questions, measures the intensity of suicidal thoughts by assessing factors such as the desire to live or die, the frequency and control of suicidal thoughts, and suicide attempts (18). Each item of the BSSI questionnaire is graded on a scale from 0 to 2 (18, 19). Scores range from 0 to 38, with higher scores indicating a higher risk of suicide. A score of 0 - 3 indicates low risk, 4 - 11 indicates medium risk, and 12 or more indicates high risk. The Farsi version of the BSSI is valid and reliable, with a Cronbach’s α of 0.827 (19).
3.3. Statistical Analysis
As mentioned in the objectives, our first goal was to estimate the prevalence of mental health disorders among medical sciences students. In this study, the sample size was calculated based on the Cochrane formula. According to the results of Lin's study (20), the global prevalence of mental disorders in medical students was reported to be 48%, and considering an error of 0.12 (d = 0.12 p), the sample size was estimated to be 290.
In this cross-sectional study, qualitative variables were presented as numbers and percentages, while quantitative variables were reported as means ± standard deviation. The chi-square test was used to determine the relationship between the levels of depression, stress, and anxiety and the intensity of suicidal thoughts. Additionally, the relationship between the levels of depression, stress, anxiety, and intensity of suicidal thoughts with the field of study was assessed using the chi-square test. Linear regression was employed to identify the factors associated with depression, stress, and anxiety (considered as quantitative variables). Simple and multivariate linear regressions were also used to determine the factors related to suicidal thoughts. Variables with a p-value less than 0.2 in the simple linear regression model were included in the multivariate analysis. The significance level in this study was set at less than 0.05. Data were analyzed using SPSS Statistics software version 22 and Stata software version 14.
4. Results
4.1. Prevalence of Mental Health Issues
A total of 292 students (190 medical, 53 dental, and 49 pharmacy students) participated in the study. The majority of students (46.6%) resided in dormitories, and 71 students (24.3%) had a history of diagnosed psychiatric illness. The prevalence of high-risk suicidal thoughts among all students was 6.5%, with 3.3% of men and 8.8% of women reporting suicidal thoughts. Furthermore, the prevalence of high-risk suicidal thoughts among medical, dental, and pharmacy students was 6.8%, 3.8%, and 8.2%, respectively. Other demographic and behavioral variables based on the intensity of suicidal thoughts are presented in Table 1.
| Variables | Total (n = 292) | Suicidal Thoughts | P-Value | ||
|---|---|---|---|---|---|
| Low Risk [126 (43.2)] | Medium Risk [147 (50.3)] | High Risk [19 (6.5)] | |||
| Age (y) | 22.90 ± 3.11 | 23.29 ± 3.67 | 22.62 ± 2.60 | 22.47 ± 2.52 | 0.176 |
| Sex | 0.155 | ||||
| Male | 122 (41.8) | 56 (45.9) | 62 (50.8) | 4 (3.3) | |
| Female | 170 (58.2) | 70 (41.2) | 85 (50.0) | 15 (8.8) | |
| Field of study | 0.913 | ||||
| Medicine | 190 (65.0) | 82 (43.2) | 95 (50.0) | 13 (6.8) | |
| Dentistry | 53 (18.2) | 24 (45.3) | 27 (50.9) | 2 (3.8) | |
| Pharmacy | 49 (16.8) | 20 (40.8) | 25 (51.0) | 4 (8.2) | |
| Current semester | 7 (5, 11) | 7 (5, 11) | 7 (5, 11) | 6 (4, 9) | 0.255 |
| Attendance hours at the university per day | 4 (6, 8) | 4 (6, 8) | 4 (6, 8) | 4 (6, 8) | 0.738 |
| Perceived difficulty of the courses | 8 (7, 9) | 8 (7, 9) | 8 (7, 9) | 8 (8, 9) | 0.230 |
| Interest in the courses | 7 (6, 9) | 8 (6, 9) | 7 (5, 9) | 6 (4, 8) | 0.001 b |
| Marital status | 0.058 | ||||
| Single | 265 (90.8) | 109 (86.5) | 137 (93.2) | 19 (100) | |
| Married | 27 (9.2) | 17 (13.5) | 10 (6.8) | 0 (0.0) | |
| Previous mental healthcare provider visit | 93 (31.8) | 33 (26.2) | 46 (31.3) | 14 (73.7) | 0.001 b |
| Positive history of psychiatric illness | 71 (24.3) | 19 (15.1) | 37 (25.2) | 15 (78.9) | 0.001 b |
| Positive history of chronic medical conditions | 27 (9.2) | 6 (4.8) | 16 (10.9) | 5 (26.3) | 0.006 b |
| Positive family history of psychiatric illness | 84 (28.8) | 33 (26.2) | 41 (27.9) | 10 (52.6) | 0.057 |
| Socioeconomic status | 0.262 | ||||
| Very low | 59 (20.2) | 24 (19.0) | 31 (21.1) | 4 (21.1) | |
| Low | 58 (19.9) | 27 (21.4) | 30 (20.4) | 1 (5.3) | |
| Middle | 59 (20.2) | 24 (19.0) | 32 (21.8) | 3 (15.8) | |
| High | 57 (19.5) | 25 (19.8) | 27 (18.4) | 5 (26.3) | |
| Very high | 59 (20.2) | 26 (20.6) | 27 (18.4) | 6 (31.6) | |
| Residence status | 0.195 | ||||
| Living with family | 138 (47.3) | 62 (49.2) | 71 (48.3) | 5 (26.3) | |
| Living in dormitory | 117 (40.1) | 48 (38.1) | 59 (40.1) | 10 (52.6) | |
| Living with roommates outside dormitory | 13 (4.5) | 5 (4.0) | 8 (5.4) | 0 (0.0) | |
| Living alone, not in the same city as family | 24 (8.2) | 11 (8.7) | 9 (6.1) | 4 (21.1) | |
Demographic and Characteristic Factors of the Participants a
The prevalence of extremely severe depression, anxiety, and stress among all students was 19.2%, 14.0%, and 8.6%, respectively. Among students with high-risk suicidal thoughts, 89.5%, 68.4%, and 73.6% reported high levels (severe and extremely severe) of depression, anxiety, and stress, respectively. As shown in Table 2, statistically significant associations were observed between the severity of stress, anxiety, and depression and the severity of suicidal thoughts (P-value < 0.001).
| Variables | Total | Suicidal Thoughts | P-Value | ||
|---|---|---|---|---|---|
| Low Risk | Medium Risk | High Risk | |||
| Depression | < 0.001 b | ||||
| Normal | 94 (32.2) | 70 (55.6) | 24 (16.3) | 0 (0.0) | |
| Mild | 50 (17.1) | 26 (20.6) | 23 (15.6) | 1 (5.3) | |
| Moderate | 61 (20.9) | 20 (15.9) | 40 (27.2) | 1 (5.3) | |
| Severe | 31 (10.6) | 6 (4.8) | 24 (16.3) | 1 (5.3) | |
| Extremely severe | 56 (19.2) | 4 (3.2) | 36 (24.5) | 16 (84.1) | |
| Anxiety | < 0.001 b | ||||
| Normal | 134 (45.9) | 86 (68.3) | 48 (32.7) | 0 (0.0) | |
| Mild | 31 (10.6) | 12 (9.5) | 18 (12.2) | 1 (5.3) | |
| Moderate | 58 (19.9) | 15 (11.9) | 38 (25.9) | 5 (26.3) | |
| Severe | 28 (9.6) | 5 (4.0) | 20 (13.6) | 3 (15.8) | |
| Extremely severe | 41 (14.0) | 8 (6.3) | 23 (15.6) | 10 (52.6) | |
| Stress | < 0.001 b | ||||
| Normal | 116 (39.7) | 74 (58.7) | 40 (27.2) | 2 (10.5) | |
| Mild | 41 (14.0) | 18 (14.3) | 23 (15.6) | 0 (0.0) | |
| Moderate | 61 (20.9) | 19 (15.1) | 39 (26.5) | 3 (15.8) | |
| Severe | 49 (16.8) | 12 (9.5) | 30 (20.4) | 7 (36.8) | |
| Extremely severe | 25 (8.6) | 3 (2.4) | 15 (10.2) | 7 (36.8) | |
Depression, Anxiety and Stress Based on the Level of Suicidal Thoughts a
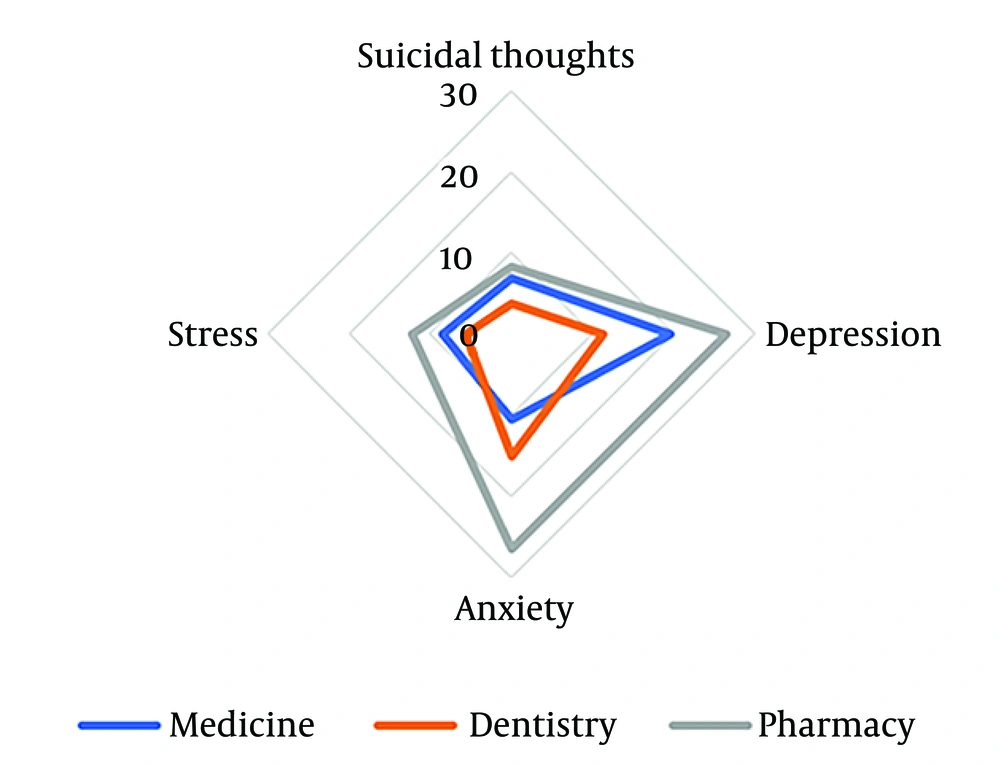
The severity of depression, anxiety, stress, and suicidal thoughts among students, based on their field of study, is reported in Table 3. A statistically significant association was found between the severity of anxiety and the field of study (P-value < 0.046). The extremely severe levels of depression, anxiety, and stress, as well as the high-risk level of suicidal thoughts based on the field of study, are presented in Figure 1. The prevalence of extremely severe depression, anxiety, and stress, as well as high-risk suicidal thoughts, was higher among pharmacy students than among medical and dental students.
| Variables | Field of Study | P-Value | ||
|---|---|---|---|---|
| Medicine | Dentistry | Pharmacy | ||
| Depression | 0.427 | |||
| Normal | 63 (33.2) | 18 (34.0) | 13 (26.5) | |
| Mild | 31 (16.3) | 8 (15.1) | 11 (22.4) | |
| Moderate | 40 (21.1) | 15 (28.3) | 6 (12.2) | |
| Severe | 19 (10.0) | 6 (11.3) | 6 (12.2) | |
| Extremely severe | 37 (19.5) | 6 (11.3) | 13 (26.5) | |
| Anxiety | 0.046 b | |||
| Normal | 91 (47.9) | 29 (54.7) | 14 (28.4) | |
| Mild | 19 (10.0) | 6 (11.3) | 6 (12.2) | |
| Moderate | 43 (22.6) | 5 (9.4) | 10 (20.4) | |
| Severe | 17 (8.9) | 5 (9.4) | 6 (12.2) | |
| Extremely severe | 20 (10.5) | 8 (15.1) | 13 (26.5) | |
| Stress | 0.798 | |||
| Normal | 77 (40.5) | 23 (43.4) | 16 (32.7) | |
| Mild | 27 (14.2) | 5 (9.4) | 9 (18.4) | |
| Moderate | 41 (21.6) | 11 (20.8) | 9 (18.4) | |
| Severe | 29 (15.3) | 11 (20.8) | 9 (18.4) | |
| Extremely severe | 16 (8.4) | 3 (5.7) | 6 (12.2) | |
| Suicidal thoughts | 0.913 | |||
| Low risk | 82 (43.2) | 24 (45.3) | 20 (40.8) | |
| Risky | 96 (50.0) | 27 (50.9) | 25 (51.0) | |
| High risk | 13 (6.8) | 2 (3.8) | 4 (8.2) | |
Depression, Anxiety, Stress, and Suicidal Thoughts Based on the Field of Study a
4.2. Factors Associated with Mental Health Outcomes
Higher age (β = -0.45; P-value = 0.027), higher academic semester (β = -0.39; P-value = 0.022), and greater interest in the courses (β = -1.41; P-value = 0.001) were significantly associated with a decrease in depression scores, while a history of psychiatric illness (β = 6.96; P-value = 0.001) was significantly associated with an increase in depression scores. Female gender (β = 2.03; P-value = 0.043), a history of psychiatric illness (β = 3.99; P-value = 0.001), a history of chronic medical conditions (β = 4.10; P-value = 0.016), and a positive family history of psychiatric illness (β = 2.27; P-value = 0.038) were significantly associated with an increase in anxiety scores. However, a higher academic semester (β = -0.28; P-value = 0.032) and greater interest in the courses (β = -0.50; P-value = 0.021) were significantly associated with a decrease in anxiety scores. Additionally, higher age (β = -0.36; P-value = 0.036), female gender (β = 3.12; P-value = 0.005), and greater interest in the courses (β = -0.86; P-value = 0.001) were significantly associated with a decrease in stress scores, while a history of psychiatric illness (β = 4.71; P-value = 0.001), a history of chronic medical conditions (β = 5.30; P-value = 0.005), and a positive family history of psychiatric illness (β = 3.04; P-value = 0.011) were significantly associated with an increase in stress scores.
4.3. Factors Associated with Suicidal Thoughts
According to the simple linear regression model, female gender (β = 1.58; P-value = 0.036), a positive history of psychiatric illness (β = 4.75; P-value = 0.001), a positive history of chronic medical conditions (β = 5.54; P-value = 0.001), and higher scores of stress (β = 0.33; P-value = 0.001), depression (β = 0.37; P-value = 0.001), and anxiety (β = 0.36; P-value = 0.001) were significantly associated with an increase in the suicidal thoughts score. However, a higher academic semester (β = -0.23; P-value = 0.018) and being married (β = -3.23; P-value = 0.012) were significantly associated with a decrease in the suicidal thoughts score (Table 4).
| Variables | β | CI for β | SE | P-Value |
|---|---|---|---|---|
| Age | -0.21 | -0.45 to 0.02 | 0.120 | 0.072 |
| Sex | ||||
| Male | Ref. | - | - | - |
| Female | 1.58 | 0.10 to 3.07 | 0.754 | 0.036 a |
| Current semester | -0.23 | -0.43 to -0.04 | 0.100 | 0.018 a |
| Perceived difficulty of the courses | 0.43 | -0.09 to 0.95 | 0.268 | 0.111 |
| Interest in the courses | -0.57 | -0.89 to -0.25 | 0.161 | < 0.001 a |
| Attendance hours at the university per day | 0.01 | -0.02 to 0.01 | 0.01 | 0.672 |
| Marital status | ||||
| Single | Ref. | - | - | - |
| Married | -3.23 | -5.74 to -0.71 | 1.279 | 0.012 a |
| Positive history of psychiatric illness | 4.75 | 3.12 to 6.31 | 0.827 | < 0.001 a |
| Positive history of chronic medical conditions | 5.54 | 3.08 to 8.01 | 1.251 | < 0.001 a |
| Positive family history of psychiatric illness | 1.46 | -0.16 to 3.08 | 0.823 | 0.077 |
| Socioeconomic status | 0.14 | -0.37 to 0.66 | 0.265 | 0.588 |
| Stress | 0.33 | 0.25 to 0.39 | 0.035 | < 0.001 a |
| Depression | 0.37 | 0.28 to 0.43 | 0.026 | < 0.00 a |
| Anxiety | 0.36 | 0.32 to 0.42 | 0.039 | < 0.001 a |
Factors Associated with Suicidal Thoughts Assessed Using Simple Linear Regression Model
In the multiple linear regression model, being single (β = -2.11; P-value = 0.034), having a positive history of psychiatric illness (β = 2.64; P-value = 0.001), and having a positive history of chronic medical conditions (β = 4.23; P-value = 0.001), as well as higher scores of depression (β = 1.97; P-value = 0.001) and anxiety (β = 0.49; P-value = 0.042), were significantly associated with suicidal thoughts (Table 5).
| Variables | β | CI for β | SE | P-Value |
|---|---|---|---|---|
| Marital status | ||||
| Single | Ref. | - | - | - |
| Married | -2.11 | -4.05 to -0.16 | 0.989 | 0.034 a |
| Positive history of psychiatric illness | 2.65 | 1.32 to 3.97 | 0.674 | < 0.001 a |
| Positive history of chronic medical conditions | 4.23 | 2.32 to 6.14 | 0.971 | < 0.001 a |
| Depression | 1.97 | 1.49 to 2.45 | 0.245 | < 0.001 a |
| Anxiety | 0.49 | 0.02 to 0.97 | 0.243 | 0.042 a |
Factors Associated with Suicidal Thoughts Assessed Using Multiple Linear Regression Model
5. Discussion
In this cross-sectional study, 66.8%, 59.5%, and 52.1% of all students experienced mild to extremely severe levels of depression, stress, and anxiety, respectively. Additionally, 56.8% of medical, dental, and pharmacy students exhibited medium to high-risk suicidal thoughts.
Moreover, interest in the courses was found to be positively associated with better mental health among students, while a diagnosed psychiatric illness was consistently linked to more severe depression, anxiety, stress, and suicidal thoughts. It is important to note that 24.3% of all students had a history of diagnosed psychiatric illness by a mental health professional. Furthermore, a history of psychiatric illness and chronic medical conditions, along with higher scores of depression and anxiety, were consistently associated with high-risk suicidal thoughts.
5.1. Prevalence of Mental Disorders
In this study, only 32.2% of students were found to be free from depression, while severe depression was observed in 19.2% of students. This is concerning when compared to a systematic review that reported a 40% prevalence of depression among medical students globally (21). A previous systematic review estimated the prevalence of anxiety among medical students at 28% (22). However, 52.1% of SUMS students are experiencing anxiety, with 14.1% reporting severe anxiety. Pharmacy students also exhibit higher levels of anxiety compared to medical and dental students, which highlights the need for further research to explore these field-specific differences. About 59.5% of SUMS students are experiencing stress, with 8.6% experiencing severe stress, which is higher than the global average of 39% stress prevalence among medical students, as estimated by studies using the DASS-21 questionnaire (21). The increase in mental health issues may be influenced by post-COVID-19 conditions, warranting further studies for evaluation.
5.2. Factors Associated with Mental Disorders
Our study found that being female was linked to higher levels of depression and anxiety, consistent with prior research (23). No association was found between students’ residence or socio-economic status and their mental health. Higher academic semesters and older age were associated with lower levels of depression, anxiety, and stress, which is consistent with previous studies (24, 25). These findings suggest that older students tend to have better mental health outcomes, possibly due to the challenges associated with the basic sciences semesters and the difficulty of transitioning from high school to the university environment, which may impact younger students.
A history of chronic or psychiatric illness, either personal or in a first-degree family member, is associated with higher levels of stress and anxiety. However, interest in courses correlates with reduced depression, anxiety, and stress. This is in line with previous studies that highlight the importance of motivation and satisfaction in student mental health (26).
5.3. Prevalence of Suicidal Thoughts
In our study, we found that a substantial 56.8% of students reported having suicidal thoughts of medium to high risk. This is notably higher than the 32% prevalence found in a similar study conducted at Tehran Medical University during the COVID-19 pandemic (27). The difference in these percentages could be attributed to the distinct data collection tools used in each study. Prior to the pandemic, international studies estimated the prevalence of suicidal thoughts to be between 7.4% and 35.6% (28, 29). This suggests that the rates of suicidal thoughts can vary significantly across different studies and contexts and may, in part, be influenced by the COVID-19 pandemic and the subsequent social distancing measures.
5.4. Factors Associated with Suicidal Thoughts
Our study found that suicidal thoughts are significantly more prevalent among female students and those with a history of psychiatric or chronic medical illness. While the gender difference in suicidal thoughts is not always consistent in the literature, when present, it is usually higher among female students (28, 30, 31). Some studies also associate being female with an increased risk of suicide attempts (31, 32). A diagnosed psychiatric condition is a significant risk factor for suicidal thoughts (29, 30, 33). However, our study found no significant correlation between suicidal thoughts and a family history of mental illness or financial issues.
On the other hand, suicidal thoughts were found to be less severe in married students. Research suggests that living alone or away from home and a lack of social support puts students at higher risk of suicidal thoughts (28, 30). Additionally, satisfaction with the field of study and being in higher semesters were negatively associated with suicidal thoughts. This finding is consistent with previous research (27, 28). As medical students progress, they tend to balance their personal and professional lives better, which may contribute to improved mental health (34). Further qualitative studies could provide more insight into these observations.
Higher intensity of depression and anxiety were positively correlated with suicidal thoughts. This correlation has also been observed in previous studies. According to a recent meta-analysis, depression is one of the most important risk factors for suicidal thoughts in medical students (30). About 31.8% of students have sought help from mental health providers, and this frequency increases with the risk of suicide, as evidenced by 73.7% of those at the highest risk reporting at least one visit. At this university, free counseling services are provided at multiple centers around the city. Most students seek counseling services at advanced stages of mental health issues. Barriers to these services, such as self-reliance, high costs, and reliance on informal support networks, need further exploration, as they significantly influence service utilization (35).
5.5. Conclusions
This study offers valuable insights into the mental health of medical, dental, and pharmacy students, revealing a significant prevalence of mental disorders and suicidal thoughts. However, its cross-sectional design and single-center focus limit the generalizability of the results and prevent the establishment of causal relationships. The data also lacked detailed information about students' interactions with mental health professionals. Although measures were taken to reduce its impact, the convenience sampling in this study could also be a source of bias. Despite these limitations, the study highlights the urgent need for interventions to promote mental health in this population. Potential policies to address these issues include periodic screening, targeted access to counseling for those at higher risk of mental health issues, stress management programs, and curriculum modifications to reduce academic pressure.