1. Background
Body dysmorphic disorder (BDD) is a debilitating mental health disorder characterized by an intense preoccupation with perceived deficiencies or defects in a person's physical appearance (1). To reduce distress due to these concerns, patients engage in excessive and repetitive mental behaviors and/or acts (1). These behaviors often include comparing one's appearance to others, repeatedly checking for imaginary defects in mirrors or other reflective surfaces, excessively handling one's appearance, encouraging others to notice imaginary defects, touching disliked areas to check them, and seeking plastic surgery (1). The BDD usually begins during adolescence (2); however, it is often not diagnosed or is misdiagnosed (3). The point prevalence of BDD in the general population ranges from 1.7% to 2.9%, 11% to 13% in dermatology clinic patients, 13% to 15% in patients referred to plastic surgery clinics, and 20% in patients undergoing rhinoplasty (4). Alavi et al. found that the prevalence of BDD in patients visiting beauty clinics in Iran is 24.5% (5). Concerns about appearance defects that do not exist, or are mild if present, and compulsive rituals are usually associated with impairment in social, occupational, or other roles, decreased quality of life, and increased rates of associated psychiatric illnesses (6).
For a reliable and valid way to measure or diagnose BDD or related symptoms, especially in cosmetic surgery, the Cosmetic Procedure Screening Questionnaire (COPS) was structured by Veale et al. in 2012. This questionnaire comprises 9 items and helps predict dissatisfaction with a cosmetic procedure or no change or deterioration in overall symptoms of BDD, and it may be sensitive to change after intervention (7). In Iran, several tools to evaluate this disorder have been validated, such as the Body Dysmorphic Disorder Questionnaire-Aesthetic Surgery (BDDQ-AS) (8). Another questionnaire is the Dysmorphic Concern Questionnaire (DCQ), validated in Iranian students (9). The Body Appreciation Scale (BAS) has been validated in university students (10). The Yale-Brown Obsessive-Compulsive Scale modified for BDD was investigated in Iran to screen the severity of symptoms in patients with this disorder (11). All these scales tend to measure predominantly the “output”—in particular, the degree of preoccupation, distress, and interference in a person’s life. However, there are no scales that measure factors that may mediate response to treatment. Even COPS can evaluate changes after treatment, not processes and factors that mediate interventions.
Among all available instruments, the Appearance Anxiety Inventory (AAI) may interest clinicians due to its good face validity, easily interpretable items, and quick administration (12). This questionnaire was designed by Veale et al. in 2014. Its background is based on meta-diagnostic models in planning and treatment. In this model, distorted imagery and shame related to one's own experience are considered central to the disorder process. The AAI is a 10-item self-report scale that focuses on cognitive processes and safety-seeking behaviors that characterize responses to distorted body image and associated shame. The goal is to create a scale that is brief, sensitive to changes during treatment, and suitable for weekly assessment. The purpose of this scale is to determine whether theorized cognitive and behavioral processes mediate change. It also seeks to help clinicians and clients determine which processes to target during treatment (13-15).
To investigate BDD, particularly in a treatment setting, we need to validate a tool that measures its symptoms and severity and can investigate processes and mediating factors (13). Due to the advantages of this tool compared to others, two studies have been conducted to evaluate its psychometric properties. In one study of 139 people diagnosed with BDD, exploratory factor analysis results showed two factors (avoidance and threat monitoring), with six items loading onto the first factor (avoidance) and four on the second factor (threat monitoring). Furthermore, the results showed that the instrument was sensitive to change and that BDD participants' scores decreased after cognitive behavioral therapy (14). In the second study, the results of factor analysis on people with high levels of appearance concern confirmed a two-factor structure (14). Roberts et al., in a study of a large sample of students using exploratory and confirmatory analysis, showed that 9 items of the AAI loaded onto a factor (13). While most plastic surgeons consider patients fit for surgery, they have found that the patient has BDD after surgery (16). Yurtsever et al. validated the AAI in a Polish sample. Twenty-eight females and 21 males completed the questionnaire twice with a 3 - 6 day interval. Their results demonstrated that the Polish version has very good internal consistency and reliability (15). Because most patients with BDD have low levels of satisfaction after surgery, their symptoms worsen, and they may even become aggressive and harsh toward themselves or their surgeon (17). Therefore, considering the problematic effects of BDD, the lack of a reliable measurement tool for this problem that is reliable and valid according to Iranian culture and the Persian language, and the need to standardize tools in different cultures (18, 19), studies have demonstrated that one of the treatments that can influence BDD is cognitive behavioral therapy (20). However, there is a need for a tool that can investigate symptoms, factors mediating intervention, and consequences of treatment. As mentioned, the AAI helps therapists and researchers with this problem and can fill this gap (14). Therefore, it is necessary to investigate the properties of instrumental psychometrics to fill these gaps in Iranian society.
The primary outcome of the study was establishing the psychometric properties (validity, reliability, factor structure) of the Persian version of the AAI. Secondary outcomes were specific relationships of the AAI with other constructs measured by body compassion, body image shame, dysmorphic concern, and the form of self-criticizing/attacking & self-reassuring scales.
2. Objectives
The purpose of this study is to examine the psychometric properties of the Persian version of the AAI in referrals to cosmetic surgery clinics.
3. Methods
3.1. Participants and Methods Sample
This psychometric study followed a quantitative correlational approach. The statistical population of this study included individuals who attended plastic surgery clinics in Tehran between 2020 and 2021. The number of samples needed for statistical analysis and confirmatory factor analysis, based on Kline, is approximately 200 (21). To reach this reliable cut point, this study selected 334 individuals through convenience sampling. The inclusion criteria for participants in this study were: Age between 15 and 50 years and literacy (ability to read and write). Exclusion criteria included having significant physical or psychological disorders, being under any form of pharmacological or psychological treatment, and a lack of willingness to participate in the study.
To evaluate the psychometric properties of the AAI, the inventory was first prepared in line with cross-cultural adaptation guidelines (22, 23). The original version of the AAI was translated from English into Persian by four psychologists and then back-translated into English by two psychologists fluent in both English and Persian. The authors then analyzed the understandability of the final translated version of the AAI. To begin with, and to check the comprehensibility of the questions, the Persian version of the instrument was piloted with a sample of 25 patients referred to cosmetic surgery clinics. Errors identified in the pilot study were discussed and corrected. Finally, the researchers approved the final version of the questionnaire.
After fulfilling the inclusion criteria, informed consent was obtained, and participants completed the survey, including the AAI, Body Compassion Scale (BCS), Body Image Shame Scale (BISS), Dysmorphic Concern Questionnaire, and the Form of Self-criticizing/Attacking & Self-reassuring Scale. The study controlled for confounders by excluding participants with significant psychological or physical disorders and medical treatments, which could affect appearance-related anxiety.
3.2. Measures
3.2.1. Appearance Anxiety Inventory
The AAI is a 10-item self-report instrument that measures cognitive processes and safety-seeking behavior in individuals with BDD. The inventory includes two dimensions: Avoidance and threat monitoring. Each question is scored on a scale from 0 (absolutely) to 4 (always). The total score ranges from 0 to 40, with scores of 19 or higher indicating the probability of BDD (14).
3.2.2. Body Compassion Scale
The BCS is a 23-item measure designed to evaluate individuals’ attitudes toward their bodies in terms of defusion, common humanity, and acceptance. Participants respond to each item using a 5-point Likert scale, ranging from 1 ("almost never") to 5 ("almost always"). Negatively worded items are reverse-scored to ensure accuracy. Higher scores indicate a greater degree of body compassion. The total score is calculated by summing the responses to all items, yielding a range of 23 to 115. In addition to the overall score, the BCS includes three distinct subscales: Defusion, common humanity, and acceptance. Cronbach's alpha for the whole scale is 0.92, and the use of the total score is recommended (24). Khanjani et al. demonstrated that this instrument, similar to its original version, has a three-factor structure, with Cronbach's alpha for the subscales of defusion, common humanity, acceptance, and the total score of the BCS reported as 0.83, 0.84, 0.69, and 0.88, respectively (25).
3.2.3. Body Image Shame Scale
This scale has 14 items that measure the shame of body image. Participants respond to each item using a 5-point Likert scale (ranging from 0 = never to 4 = almost always), according to how often they experience embarrassment about body image. Temporary stability and internal consistency have been reported to be high, with Cronbach's alpha for the total score at 0.96 (26). Recent research in Iran has reported a good fit for the two-factor structure of the BISS (27).
3.2.4. Dysmorphic Concern Questionnaire
The DCQ is a 7-item questionnaire that measures the extent of concern about physical appearance. Responses are rated using a 4-point Likert scale (0 - 3), with 3 indicating the highest level of concern for each item (28). In Iran, previous research has approved the DCQ's single-factor structure, with a Cronbach's alpha coefficient of 0.78 (29).
3.2.5. Form of Self-criticizing/Attacking and Self-reassuring Scale (FSCRS)
This scale is a 22-item self-report tool that assesses how people think and react in the face of failure. It measures two dimensions: Self-criticism and self-confidence capacity. Participants are asked to choose the extent to which each question applies to their experiences on a 5-point Likert scale (from 0 = not at all like me to 4 = quite like me). Cronbach's alpha was 0.90 for self-sufficiency and 0.86 for self-confidence (30).
3.3. Statistical Analysis
Data were screened using SPSS software version 26 for descriptive statistics. Divergent and convergent validity was assessed using the Pearson correlation test between the AAI and the BCS, BISS, DCQ, Form of Self-Criticising/Attacking & Self-Reassuring Scale (FSCRS), and the Acceptance and Action Questionnaire-Body Image (AAQ-BI) scores. Internal consistency and test-retest reliability (with a 4-week interval between two measurements with 30 participants) were used to assess the reliability of the scale. Cronbach's alpha was used to calculate the internal consistency of the scale, and the intraclass correlation coefficient was calculated for the reliability of retesting the AAI.
LISREL version 8.80 was used for confirmatory factor analysis (CFA). The CFA was selected to evaluate the fit of the one-factor and two-factor models. To fit the model, the normal chi-square, goodness of Fit Index (GFI), normed fit index (NFI), standardized root mean square residual (SRMR), non-normed fit index (NNFI), incremental fit index (IFI), adjusted GFI (AGFI), and root mean square error of approximation (RMSEA) were used. An RMSEA coefficient less than 0.08, SRMR less than 0.10, and fit indices for CFI, GFI, AGFI, IFI, RFI, NFI, and NNFI above 0.90, with AGFI above 0.85, indicate acceptable fit indices for confirmatory factor analysis (31, 32).
3.4. Ethical Consideration
The ethics code for the present study is IR.IUMS.REC.1398.1206, approved in 1398 by the Iran University of Medical Sciences. The informed consent form emphasized the voluntary nature of participation, as well as the confidentiality and anonymity of the collected information.
4. Results
A total of 334 patients referred to cosmetic surgery clinics, aged 15 - 54 years, with a mean age of 25.88 ± 5.42 years, participated in this study. Among these participants, 124 were male (37.1%) and 210 were female (62.9%). Of the participants, 285 (85.3%) were single and 49 (14.7%) were married. Regarding the educational qualifications of the research participants, 38 individuals (11.4%) were below diploma level, 112 (33.5%) had a diploma, 146 (43.7%) had a bachelor's degree, and 38 (11.4%) had a master's degree.
4.1. Item-Total Correlations and Inter-Item Correlations of Appearance Anxiety Inventory
Table 1 shows the item-total correlations and inter-item correlations for the AAI. The item-total correlations for the Avoidance and Threat Monitoring scales were high, with values of 0.95 and 0.85, respectively, indicating that these scales are strong indicators of their respective constructs. Inter-item correlations varied across items, ranging from 0.12 to 0.50, with some items showing high correlations with others, suggesting they measure similar aspects of the constructs. Items with high item-total correlations and inter-item correlations are considered strong indicators, whereas items with lower correlations may capture different aspects or be less related to the overall constructs. The significance levels for all correlations were generally at the 0.05 level, indicating strong statistical significance.
| DCQ | Item-Total Correlation | Inter-Item Correlation | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | Item 6 | Item 7 | Item 8 | Item 9 | Item 10 | ||
| Avoidance | 0.95 a | ||||||||||
| Threat monitoring | 0.85 a | ||||||||||
| Item 1 | 0.46 a | ||||||||||
| Item 2 | 0.62 a | 0.43 a | |||||||||
| Item 3 | 0.71 a | 0.20 a | 0.35 a | ||||||||
| Item 4 | 0.74 a | 0.32 a | 0.42 a | 0.50 a | |||||||
| Item 5 | 0.51 a | 0.12 b | 0.12 a | 0.31 b | 0.32 a | ||||||
| Item 6 | 0.68 a | 0.26 a | 0.41 a | 0.46 a | 0.49 a | 0.26 a | |||||
| Item 7 | 0.61 a | 0.12 b | 0.23 a | 0.43 b | 0.34 a | 0.30 a | 0.26 a | ||||
| Item 8 | 0.64 a | 0.25 a | 0.36 a | 0.43 a | 0.45 a | 0.17 a | 0.36 a | 0.32 a | |||
| Item 9 | 0.49 a | 0.13 b | 0.26 a | 0.24 a | 0.22 a | 0.22 a | 0.24 a | 0.28 a | 0.23 a | ||
| Item10 | 0.68 a | 0.15 a | 0.25 a | 0.43 a | 0.49 a | 0.31 a | 0.39 a | 0.50 a | 0.40 a | 0.23 a | - |
Item-Total Correlations and Inter-Item Correlations of Appearance Anxiety Inventory
4.2. Reliability
Internal consistency was assessed using Cronbach's alpha coefficient for the AAI and its subscales: Avoidance and threat monitoring. The coefficients were 0.81 for the total AAI, 0.77 for the avoidance subscale, and 0.63 for the threat monitoring subscale. McDonald's omega coefficients were calculated as follows: 0.77 for avoidance, 0.52 for threat monitoring, and 0.81 for the total score. Test-retest reliability, with a 4-week interval between two measurements, was evaluated by calculating the intraclass correlation coefficient (ICC) for the AAI and its subscales, yielding values of 0.89 for the total AAI, 0.91 for avoidance, and 0.78 for threat monitoring.
4.3. Validity
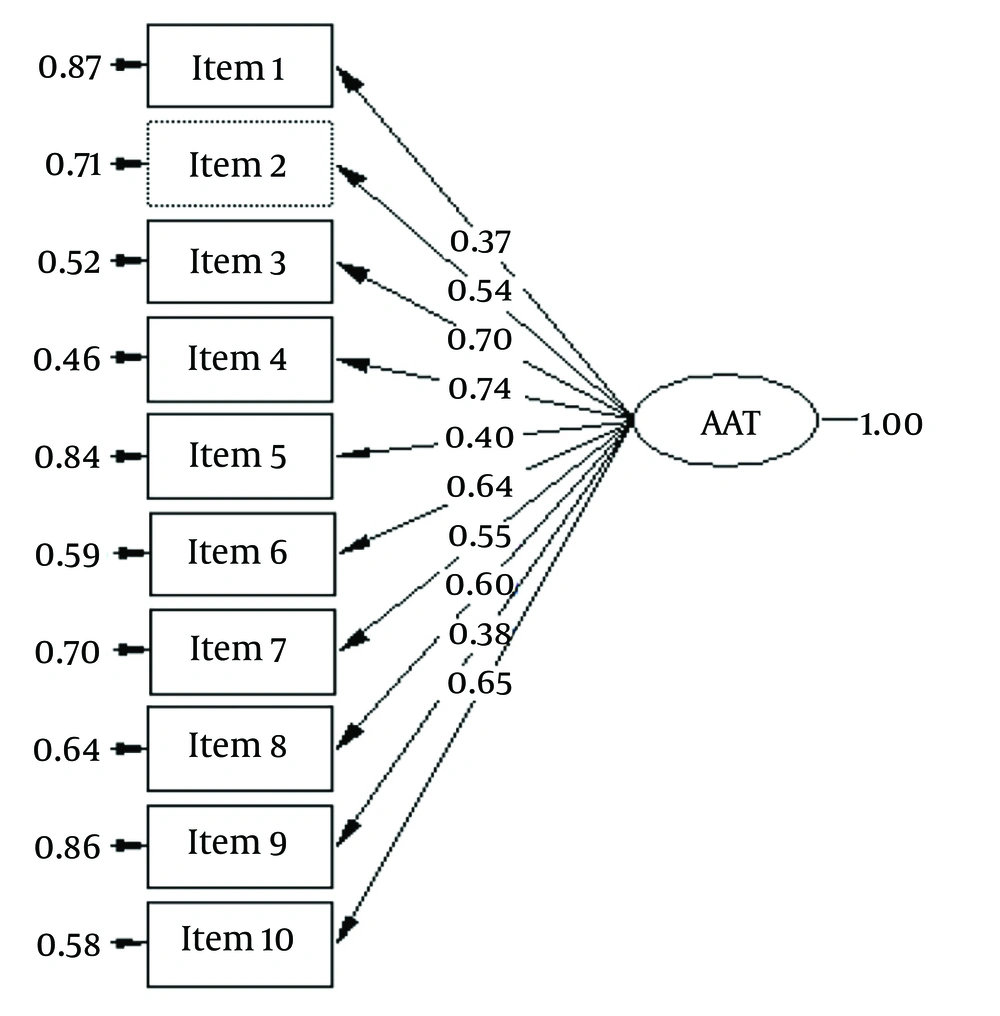
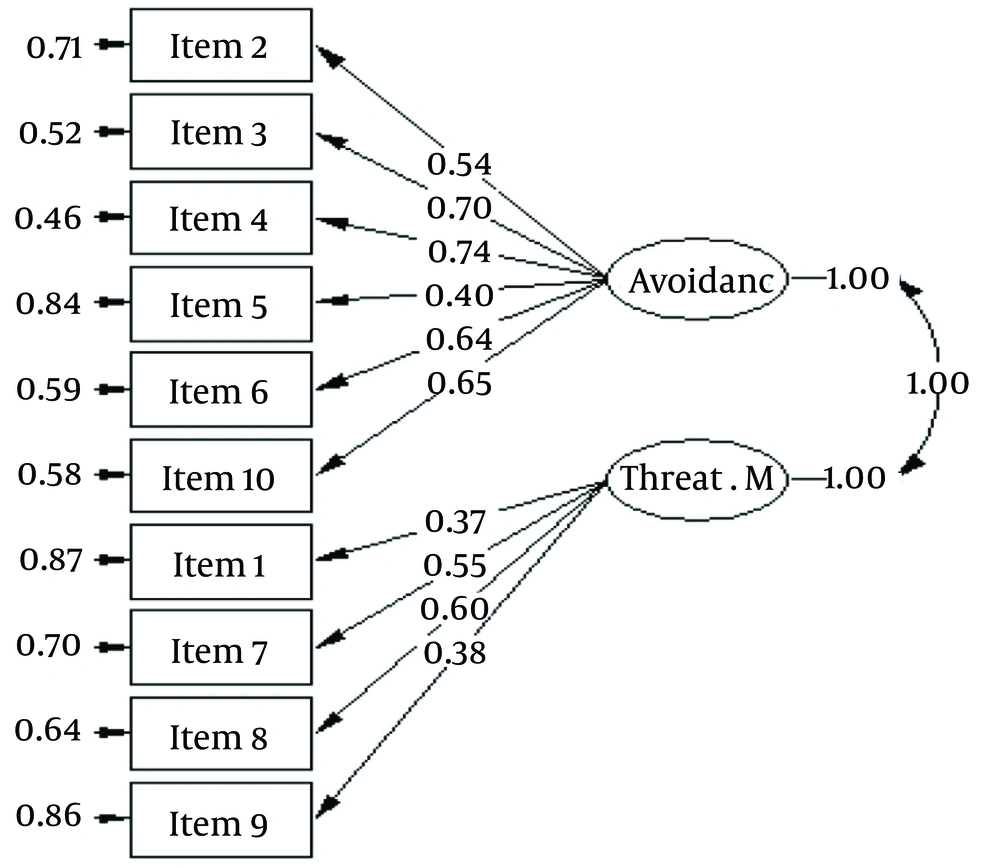
We used two methods to assess the validity of the AAI. Figure 1 (single-factor solution of AAI) illustrates how multiple observed variables (items) are hypothesized to load onto a single underlying latent factor, representing appearance anxiety. Figure 2 (two-factor solution of AAI) shows how observed variables (items) are hypothesized to load onto two distinct latent factors (avoidance and threat monitoring), representing different dimensions of appearance anxiety. The results of fitting the indices of the two models are shown in Table 2.
| Fit Indexes | χ2 | P | χ2/df | SRMR | GFI | IFI | CFI | AGFI | NNFI | NFI | RMSEA |
|---|---|---|---|---|---|---|---|---|---|---|---|
| One-Factor | 131.91 | 0.001 | 3.77 | 0.06 | 0.93 | 0.95 | 0.95 | 0.88 | 0.93 | .093 | 0.09 |
| Two-Factor | 131.89 | 0.001 | 3.88 | 0.06 | 0.93 | 0.95 | 0.95 | 0.88 | 0.93 | 0.93 | 0.09 |
Fit Indexes for Appearance Anxiety Inventory
As shown in the table, the one-factor CFA solution demonstrated a good fit with a χ2 value of 131.91 (df = 35), a χ2/df ratio of 3.77, CFI of 0.95, IFI of 0.95, GFI of 0.93, NFI of 0.93, NNFI of 0.93, RMSEA of 0.09, and SRMR of 0.06, indicating it adequately represents the data. Similarly, the two-factor CFA solution demonstrated a good fit with a χ2 value of 131.89 (df = 34), a χ2/df ratio of 3.88, CFI of 0.95, IFI of 0.95, GFI of 0.93, NFI of 0.93, NNFI of 0.93, RMSEA of 0.09, and SRMR of 0.06, indicating a good fit to the data.
Overall, both the one-factor and two-factor models demonstrate acceptable fit across most of the indices, with only slight variations. The fit indices do not strongly favor one model over the other, suggesting that the choice between the one-factor and two-factor models should be guided by theoretical considerations or other criteria not captured by these statistics.
4.4. Convergent and Divergent Validity
As shown in Table 3, the AAI and its subscales had a positive and significant relationship with concern about BDD (r = 0.47), body image shame (r = 0.70), and self-criticism (r = 0.58), indicating appropriate convergent validity of the scale. The AAI and its subscales were significantly and negatively correlated with body compassion (r = -0.60) and acceptance and action of body image (r = -0.58), indicating that the scale has significant divergent validity.
5. Discussion
The AAI is a widely used tool in clinical research to assess the severity of BDD and response to treatment in adolescent and adult samples (33). This study aimed to evaluate the validity and reliability of the AAI in individuals visiting cosmetic surgery clinics. The results of our research supported the two-factor structure of this inventory. The first factor indicated avoidance and camouflage, and the second factor was threat monitoring. Items in the avoidance factor include avoiding cues that cause negative self-assessment or others, as well as attempting to camouflage and cover up perceived flaws. Items in the threat monitoring factor include focusing excessively on oneself and comparing one's internal image to what is seen in the mirror or on flat surfaces. Rumination and questioning others may occur in response to a memory of an image, in an attempt to closely examine one's appearance and solve perceived problems.
This finding is consistent with the study by Veale et al., which confirmed the two-factor structure of the appearance anxiety questionnaire in a clinical population (14). Additionally, the results showed that the one-factor structure of the AAI in Iranian society is confirmed, consistent with previous research (13, 14). This finding aligns with the study by Roberts et al., except that their sample consisted of students, and exploratory and confirmatory factor analysis results showed that nine items loaded onto one factor (13). Furthermore, a study conducted by Veale et al. on a nonclinical population supported the one-factor structure (14). A study conducted in Sweden reached similar results to ours, with the difference that their sample group was young people with BDD (12).
The AAI in our study showed good internal consistency and good retest reliability. Our results on the reliability of the Appearance Anxiety Questionnaire are consistent with previous research (13, 14).
To assess the divergent validity of the AAI, the Compassion for Body and Acceptance and Action Questionnaire was used. The results showed a negative correlation between appearance anxiety and compassion for the body and acceptance and practice of body image, which is consistent with previous research (29, 34, 35). Foroughi et al. demonstrated that compassion itself plays a protective role against concerns about body image (34). Allen et al. also reported that high self-compassion is associated with lower levels of body dysmorphic symptoms (35).
To assess the convergent validity of the AAI, the Concern about Body Dysmorphic, Shame of Body Image, and the self-criticism dimension of the FSCRS were used. Findings showed good convergent validity results, consistent with previous research (27, 34, 36-38). Khanjani et al. examined body image shame psychometrically and found a significant relationship between appearance anxiety and body image shame and self-criticism (27). Weingarden et al. showed a significant relationship between general shame, body shame, and BDD (36).
The results of our research support the one-factor and two-factor structure of the AAI and also demonstrate that the AAI has convergent and divergent validity, internal consistency, and reliability, as well as good retest reliability. The strength of the study was the large sample size of individuals visiting cosmetic surgery clinics, which can help surgeons and therapists evaluate their interventions and the consequences thereof.
5.1. Limitations
This study had some limitations that future research should address: First, the findings of the present study did not include a clinical diagnosis of individuals referring to cosmetic surgery clinics, so the results might not be generalizable to individuals with a clinical picture of BDD. Second, obtaining information from self-reporting tools introduces the possibility of response bias and socially desirable responses, which may lead to underreporting of BDD symptoms. Third, most participants in this study were women and single, which could limit the generalizability of the findings to men and married individuals. Fourth, the AAI does not focus on experiencing body image or distorted feelings and metacognitive beliefs about body image.
5.2. Conclusions
The present study contributes to the existing literature on the measurement of behavioral symptoms and cognitive processes associated with the distorted body image characteristic of BDD. This study enhances the cross-cultural literature on the AAI. Based on the results of this study, the Appearance Anxiety Questionnaire is an appropriate tool for research and clinical work in cosmetic surgery applicants.