1. Background
The COVID-19 pandemic, recognized as one of the major healthcare crises of this century, has profoundly impacted healthcare services and led to significant morbidity and mortality among both the public and healthcare professionals (HCPs) worldwide (1). Beyond its socio-economic consequences, the pandemic has severely affected the mental health of people globally (1, 2). This crisis has brought moral injury back into focus, as HCPs were often required to perform medical interventions in challenging and complex situations (3).
Healthcare professionals have been working tirelessly, enduring long hours under immense pressure and facing numerous difficulties every day (4). They have also been confronted with difficult moral and ethical decisions, such as determining which patients should receive medical support in the event of a shortage of resources. Such decisions can lead to moral injury (5). For many healthcare workers, who entered the profession with the goal of saving lives and helping people, having to decide who receives treatment and who does not can be a severe blow to their core values. This is particularly true for those who are unprepared, inexperienced, and lacking adequate support (3).
Moral injury is described as psychological distress resulting from events that violate one's moral conscience and values, causing deep feelings of guilt or shame (6). In some cases, it can lead to feelings of betrayal, anger towards colleagues, leaders, organizations, politics, or society at large-moral disorientation and social alienation (7). In the medical field, doctors may experience moral injury if they are unable to uphold their oath to provide the best possible care and prioritize their patients' interests (8). While moral injury is not classified as a mental illness, it often leads to pessimistic thoughts about others and oneself, which can result in mental health issues. Given that certain healthcare workers may face circumstances that hinder them from maintaining their moral or ethical standards, moral injury has become a significant and widespread concern during the COVID-19 pandemic (9).
The impacts of moral injury on individuals are not always immediately recognizable, but the psychological damage it causes can result in long-lasting emotional, behavioral, and social problems, such as anger, depression, anxiety, post-traumatic stress disorder, burnout, compassion fatigue, and even suicidal ideation (3). It is crucial to support HCPs in improving their mental health and attitudes during these unprecedented times, as this will benefit both their well-being and the public's recovery. To develop effective strategies for aiding HCPs, it is essential to assess their current status. Post-pandemic, addressing ethical damage among HCPs must be a primary objective.
2. Objectives
Few studies have investigated the prevalence of moral injury among healthcare professionals and its relation to psychological damage. This study was designed and conducted to evaluate moral injury among healthcare professionals during the COVID-19 pandemic.
3. Methods
3.1. Study Design
This cross-sectional survey was conducted with 333 HCPs between December 2020 and January 2021 at educational hospitals affiliated with Shiraz University of Medical Sciences, Shiraz, Iran.
3.2. Sample Size and Sampling Method
The estimated size of the statistical population was around 3,000 people. According to the type of study, the sample size was determined to be at least 300 people, based on the Krejcie and Morgan table, which is used to estimate sample sizes for descriptive studies (10). The sampling method employed was chain-referral sampling, also known as snowball sampling. This process began with an initial group of nurses, medical interns, and residents who were invited to participate in the study. Subsequently, these initial participants were asked to distribute the online questionnaire among their colleagues. This procedure continued until the study reached the desired sample size.
3.3. Inclusion and Exclusion Criteria
Medical interns, residents, and nurses working in educational hospitals affiliated with Shiraz University of Medical Sciences, who were 18 years old or older and willing to participate, were included in the study. Participants who did not complete the survey, provided incomplete responses, or did not give their informed consent were excluded from the study.
3.4. Questionnaires
The HCPs were invited to participate in the study via social media platforms, and an online platform was used to collect the surveys. The questionnaire consisted of three main components: Demographic characteristics, the Depression Anxiety Stress Scales (DASS-21), and the Moral Injury Symptom Scale-Healthcare Professionals version (MISS-HP) (Appendices 1-5 in the Supplementary file).
3.5. Depression Anxiety Stress Scales Questionnaire
The DASS-21 is a self-reported screening instrument designed for the general population and patients to measure depression, anxiety, and stress independently (11). The depression subscale evaluates feelings of hopelessness, lethargy, lack of interest, self-deprecation, dysphoria, and anhedonia. The anxiety subscale measures autonomic arousal, musculoskeletal symptoms, situational anxiety, and subjective feelings of anxiety. The stress subscale assesses irritability, anxious arousal, ease of disturbance or irritation, and difficulties with relaxation. Each subscale consists of seven items rated on a 4-point Likert Scale (0 - 3). The total score ranges from 0 to 63, with higher scores indicating higher levels of stress, anxiety, and depression.
The severity of symptoms is indicated by the scores in each domain (12). The cross-cultural validity of the DASS-21-Persian for measuring related symptoms among the general population in Iran has been evaluated in previous studies (11). The internal consistency of the DASS-21-Persian, calculated using Cronbach’s alpha (α), was found to be an acceptable 0.94 (13).
3.6. Moral Injury Symptom Scale-Healthcare Professionals Questionnaire
The MISS-HP is a 10-item questionnaire designed to assess various dimensions of moral injury. Responses for each item range from 1 (indicating "absolutely disagree") to 10 (indicating "absolutely agree") on a 10-point Likert Scale. The total score can range from 10 to 100, with higher values indicating more severe moral harm (14). For our study, the MISS-HP was translated into Persian, and the translated version was validated through a pilot study (15).
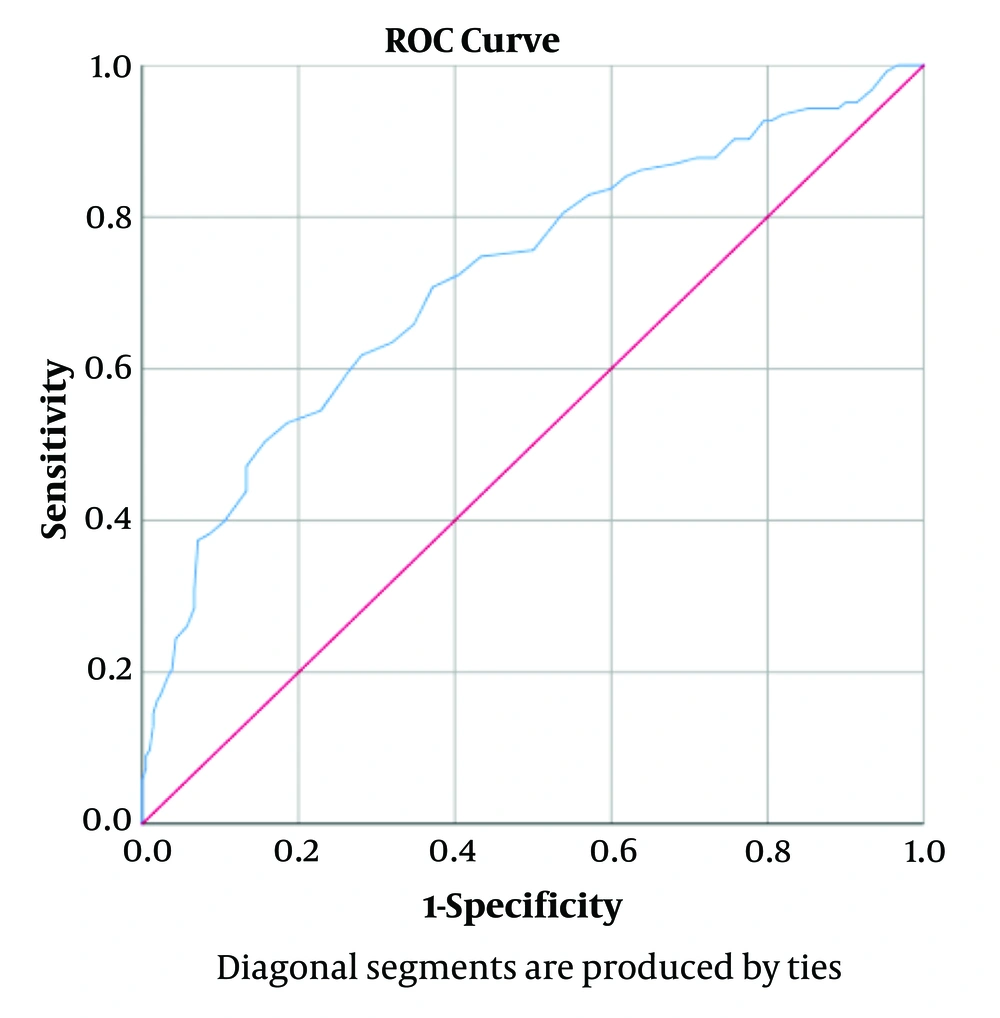
The optimal cutoff score for identifying healthcare professionals with clinically significant moral injury symptoms using the MISS-HP-Persian was determined to be 42 or higher, according to Youden’s index from the receiver operating characteristic (ROC) curve. The ROC curve is a tool used to evaluate how well the questionnaire distinguishes between healthcare professionals with and without clinically significant moral injury symptoms. Youden’s index summarizes the ROC curve, helping to identify the optimal cutoff point. In this study, a score of 42 or higher on the MISS-HP-Persian indicates clinically significant moral injury symptoms (Figure 1). With this cutoff point, the sensitivity and specificity for detecting moral injury symptoms with significant functional impairment were 70% and 63%, respectively (positive predictive value: 53%, negative predictive value: 79%).
Content validity of the questionnaire was evaluated both qualitatively and quantitatively. For qualitative content validity, the questionnaire was reviewed by thirty-five experts, who provided feedback on item allocation, wording, scaling, and grammar. This method of content validation follows previous publications (16). The internal consistency of the questionnaire was assessed using Cronbach’s alpha (α), yielding an acceptable rate of 0.73 (13).
3.7. Statistical Analysis
For analysis, SPSS 24 was used. Continuous variables were reported as means and standard deviations, while categorical variables were presented as numbers and percentages. Univariate analysis was conducted using the independent t-test, Pearson correlation coefficient, and Spearman correlation coefficient. Multivariable analysis was performed after checking for variance inflation factors (VIF) and collinearity using one-way ANOVA (P < 0.05).
3.8. Ethical Approval
The protocol was approved by the Medical Ethics Committee of Shiraz University of Medical Sciences (ethical code: IR.SUMS.MED.REC.1399.545). Participants were asked to provide informed consent at the beginning of the questionnaire. The anonymity and confidentiality of the participants were ensured.
4. Results
A total of 333 healthcare professionals participated in this study, with the majority being in the 26 to 30-year age group. The study population comprised 107 nurses (32.1%), 125 medical interns (37.5%), and 101 medical residents (30.3%). Among the participants, 195 were female (58.6%) and 138 were male (41.1%). More than half of the respondents were single (61.6%), and most participants (60.1%) had been in their profession for 1 - 3 years (Table 1).
| Variables | No. (%) |
|---|---|
| Gender | |
| Female | 195 (58.6) |
| Male | 138 (41.1) |
| Age group (y) | |
| 21 - 25 | 106 (31.8) |
| 25 - 30 | 147 (44.1) |
| > 30 | 80 (24.0) |
| Marital status | |
| Single | 205 (61.6) |
| Married | 128 (38.4) |
| Profession | |
| Medical intern | 125 (37.5) |
| Medical resident | 101 (30.3) |
| Nurse | 107 (32.1) |
| Years of profession | |
| 1 - 3 | 200 (60.1) |
| 4 - 7 | 94 (28.2) |
| > 7 | 39 (11.7) |
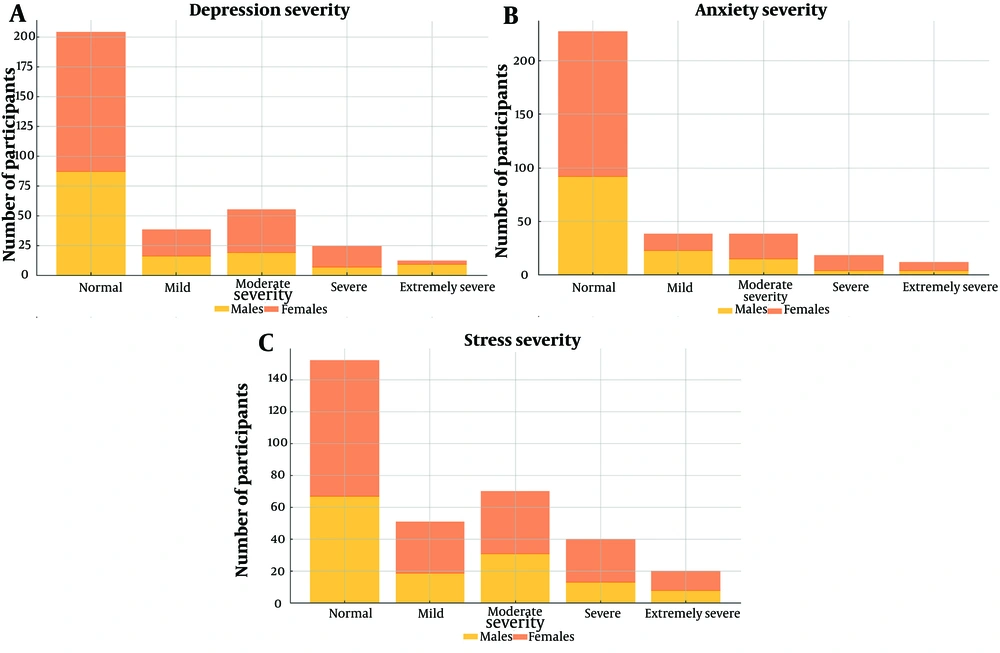
Table 2 presents the results of the DASS-21 Persian questionnaire distributed among the participants. Moderate to extremely severe anxiety was detected in 23 (16.7%) male participants. The rates for stress and depression in male participants were 52 (37.7%) and 35 (25.4%), respectively. In comparison, anxiety, stress, and depression were diagnosed in 45 (23.1%), 78 (40%), and 56 (28.7%) female participants, respectively (Figure 2).
| Variables | Males (N = 138) | Females (N = 195) | Total (N = 333) |
|---|---|---|---|
| Depression | |||
| Normal | 87 (63) | 117 (60) | 204 (61.3) |
| Mild | 16 (11.6) | 22 (11.3) | 38 (11.4) |
| Moderate | 19 (13.6) | 36 (18.5) | 55 (16.5) |
| Severe | 7 (5.1) | 17 (8.7) | 24 (7.2) |
| Extremely severe | 9 (6.5) | 3 (1.5) | 12 (3.6) |
| Anxiety | |||
| Normal | 92 (66.7) | 135 (69.2) | 227 (68.2) |
| Mild | 23 (16.7) | 15 (7.7) | 38 (11.4) |
| Moderate | 15 (10.9) | 23 (11.8) | 38 (11.4) |
| Severe | 4 (2.9) | 14 (7.2) | 18 (5.4) |
| Extremely severe | 4 (2.9) | 8 (4.1) | 12 (3.6) |
| Stress | |||
| Normal | 67 (48.6) | 85 (43.6) | 152 (45.6) |
| Mild | 19 (13.8) | 32 (16.4) | 51 (15.3) |
| Moderate | 31 (22.5) | 39 (20) | 70 (21.0) |
| Severe | 13 (9.4) | 27 (13.8) | 40 (12.0) |
| Extremely severe | 8 (5.8) | 12 (6.2) | 20 (6.0) |
a Values are expressed as No. (%).
According to Table 3, females had significantly higher mean scores for both anxiety (P = 0.001) and stress (P = 0.001) compared to males. Single participants had significantly higher mean depression scores (P = 0.007). Nurses exhibited the highest levels of depression (P = 0.001), anxiety (P = 0.001), and stress (P = 0.006) compared to medical interns and residents. Participants without adequate personal protective equipment (PPE) reported significantly higher levels of depression (P = 0.004), anxiety (P = 0.014), and stress (P = 0.0001). Additionally, work experience with the death of COVID-19 patients was associated with significantly higher levels of depression (P = 0.047) and stress (P = 0.028).
| Variables | Depression | P-Value | Anxiety | P-Value | Stress | P-Value | Moral Injury | P-Value |
|---|---|---|---|---|---|---|---|---|
| Gender | 0.063 b | 0.001 b | 0.001 b | 0.018 b | ||||
| Male | 6.61 ± 5.33 | 4.47 ± 4.11 | 8.35 ± 5.06 | 39.51 ± 11.81 | ||||
| Female | 7.72 ± 5.38 | 6.21 ± 4.76 | 10.35 ± 4.97 | 42.92 ± 13.56 | ||||
| Marital status | 0.007 b | 0.902 b | 0.203 b | 0.044 b | ||||
| Single | 7.89 ± 5.54 | 5.51 ± 4.65 | 9.81 ± 5.09 | 42.63 ± 12.86 | ||||
| Married | 6.26 ± 4.97 | 5.45 ± 4.47 | 9.07 ± 5.11 | 39.70 ± 12.95 | ||||
| Type of profession | 0.001 c | 0.001 c | 0.006 c | 0.007 c | ||||
| Nurses | 8.81 ± 5.79 | 7.64 ± 5.51 | 10.81 ± 5.18 | 44.01 ± 13.33 | ||||
| Medical Interns | 6.80 ± 5.34 | 4.32 ± 3.56 | 9.00 ± 5.12 | 41.88 ± 11.86 | ||||
| Medical Residents | 6.20 ± 4.60 | 4.66 ± 3.77 | 8.83 ± 4.78 | 38.39 ± 13.34 | ||||
| Adequacy of personal protective equipment | 0.004 b | 0.014 b | 0.0001 b | 0.0001 b | ||||
| Yes | 6.54 ± 5.02 | 4.97 ± 4.27 | 8.66 ± 4.86 | 39.26 ± 12.75 | ||||
| No | 8.28 ± 5.71 | 6.21 ± 4.89 | 10.74 ± 5.21 | 44.64 ± 12.63 | ||||
| Work experience with the death of COVID-19 patients | 0.047 b | 0.169 b | 0.028 b | 0.095 b | ||||
| Yes | 7.69 ± 5.48 | 5.74 ± 4.73 | 9.98 ± 5.10 | 42.37 ± 13.18 | ||||
| No | 6.46 ± 5.11 | 5.01 ± 4.24 | 8.68 ± 5.02 | 39.87 ± 12.42 | ||||
| Years of profession | 0.097 c | 0.065 c | 0.525 c | 0.249 c | ||||
| 1 - 3 (y) | 7.53 ± 5.56 | 5.44 ± 4.54 | 9.64 ± 5.12 | 42.47 ± 12.55 | ||||
| 4 - 7 (y) | 6.30 ± 4.56 | 4.97 ± 4.13 | 9.08 ± 4.91 | 40.13 ± 13.68 | ||||
| More than 8 (y) | 8.20 ± 5.88 | 7.00 ± 5.47 | 10.05 ± 5.53 | 39.87 ± 13.12 |
a Values are expressed as mean ± SD.
b Independent t-test.
c One-way ANOVA.
The average score obtained on the MISS-HP was 41.51 with a standard deviation of 12.96. The results indicated that 49.6% of the participants experienced clinically significant moral injury, while 50.4% had non-clinically significant moral injury. We also examined the correlation between moral injury and symptoms of depression, anxiety, and stress using the Pearson correlation coefficient test. The results showed a significant positive correlation between moral injury and depression (correlation coefficient = 0.471, P = 0.001), anxiety (correlation coefficient = 0.430, P = 0.001), and stress (correlation coefficient = 0.464, P = 0.001).
Based on our findings, female participants had higher rates of moral injury than their male counterparts (P = 0.018) (Table 3). Single participants experienced more moral injury than married ones (P = 0.044). Our results also indicated that moral injury was significantly higher in nurses compared to other healthcare professionals (P = 0.007). Furthermore, moral injury was significantly correlated with inadequate PPE at the workplace (P = 0.0001) (Table 3).
5. Discussion
This study assessed the prevalence of moral injuries, stress, anxiety, and depression among HCPs during the pandemic. 20.4% of the participants reported experiencing anxiety, which is consistent with findings from previous studies in Italy, China, and India (17-19). In our study, the prevalence of depression was 27.3%, similar to the findings reported by Rossi et al. (17). Other studies have also observed increased levels of anxiety and depression among HCPs on the frontlines of outbreaks, such as volunteers treating patients with Ebola in West Africa (20). In our study, 39.1% of participants had moderate to highly severe stress symptoms, which is significantly higher than the rate found by Lenzo et al. using the same assessment tool (21). These variations may be attributed to the phase of the outbreak during which the studies were conducted. Since our study was carried out between the third and fourth peaks of the pandemic in Iran, the higher rates could reflect the increased burden on healthcare systems during the peak phase. Factors such as the duration and degree of exposure to COVID-19 patients, the type of study, the characteristics of the study population, the assessment tools used, and sociocultural differences may also contribute to variations in findings across different studies.
Our results indicated that about one in two HCPs suffered from moral injury during the COVID-19 pandemic, with 49.1% of all participants exhibiting clinically significant moral injury. These findings are consistent with previous evidence showing that a significant proportion of HCPs are at risk of moral injury during the pandemic (22).
In this study, although female participants were at higher risk for developing anxiety, stress, and moral injury, no significant difference was found in depression levels between different genders. Wang et al. previously reported that female HCPs were more vulnerable to moral injury during the COVID-19 pandemic (22). Additionally, other investigations have shown a higher prevalence of anxiety, stress, and depression among female HCPs during the pandemic (23, 24). These higher levels of psychological distress among women were also observed in the general population, suggesting that women may be more vulnerable to developing anxiety, stress, and depression than men (25-27).
Depression and moral injury were significantly lower among married participants. Consistent with our findings, Wang et al. reported lower rates of these issues in married healthcare workers (22). Similarly, married individuals demonstrated higher levels of resilience against anxiety, stress, and depression during the COVID-19 pandemic (23). Previous studies have also identified marital status as a factor influencing the risk of developing depression due to various social and psychological reasons (28, 29).
According to our study’s findings, there is a substantial correlation between profession and the levels of stress, anxiety, depression, and moral injury. In line with previously published evidence, our study indicated that nurses experienced higher levels of anxiety, stress, depression, and moral injury compared to medical interns and residents (22). This difference may be attributed to nurses spending more hours providing medical services to COVID-19 patients than medical interns and residents. Xiao et al. also observed a higher prevalence of anxiety and depression among nurses, although the difference between various HCP groups was not statistically significant (30).
The lack of PPE in the workplace increased participants’ levels of anxiety, stress, depression, and moral injury. This finding aligns with previous reports indicating that inadequate PPE significantly elevated anxiety and depression levels among HCPs (30). Other studies have also shown that adequate provision of PPE mitigates anxiety and depression among HCPs (31). The fear of contracting and potentially spreading the virus due to insufficient protective equipment likely contributed to these heightened levels of anxiety and depression.
Additionally, we observed that HCPs who worked with end-stage COVID-19 patients experienced higher levels of stress and depression. Previous studies have found a strong correlation between death anxiety and mental disorders such as depression (32). Physicians may empathize deeply with these patients, leading to feelings of fear, grief, and depression.
Our findings showed a significant correlation between self-reported depressive symptoms and moral injury in the study population. This result is consistent with a recent study evaluating the association between psychiatric symptoms and moral injury among HCPs during the COVID-19 pandemic (33). Previous research has also demonstrated an association between psychopathology and moral injury among military veterans (34-38). Additionally, trauma-related stress has been highlighted in a recent review evaluating traumatic responses among HCPs during the COVID-19 outbreak (39). In line with the findings of Amsalem et al., we observed that the effects of the COVID-19 pandemic on HCPs resemble the impacts following a traumatic event (33). Ahmed and Umaralso evaluated the concern regarding Ebola and Swine flu, noting a rising apprehension towards these outbreaks (40). Other publications have further emphasized the importance of addressing moral injury among HCPs during the pandemic (41-44).
Based on our findings, early diagnosis and treatment of mental health issues among HCPs are highly recommended. However, many HCPs are reluctant to seek mental health care, complicating the issue further. Stigma surrounding mental health care is a significant barrier, as some HCPs view psychiatric follow-up as a sign of weakness or failure to meet social expectations (45). The presence of mental health problems among HCPs long after the COVID-19 pandemic has subsided is a crucial issue that should not be ignored, as it can leave HCPs vulnerable (46-48).
5.1. Limitations
Our study has several limitations. Although participants were drawn from various sections of the hospitals, there is a potential for selection bias, as our study was conducted through a web-based survey. The findings are limited to the population from which the sample size was derived, and may not represent HCPs in other regions of the world. Furthermore, our assessment relied on self-report questionnaires, which do not provide the accuracy of a formal diagnostic interview.
5.2. Conclusions
The study's findings revealed the prevalence of anxiety, stress, depression, and moral injury among HCPs during the COVID-19 pandemic, as well as the relationship between moral injuries and the participants' levels of anxiety, stress, and depression. Female HCPs exhibited a higher prevalence of anxiety and stress during the pandemic compared to their male counterparts. Additionally, being married appeared to be a protective factor against depression and moral injury. Variations in anxiety, stress, depression, and moral injury were observed across different positions, with nurses being more vulnerable to these issues. Encounters with end-stage patients and inadequate resources, such as PPE, were other factors contributing to increased rates of anxiety, stress, depression, and moral injury during the crisis.
A growing body of evidence suggests that the prevalence of mental health disorders, including anxiety, depression, and stress, has increased among HCPs since the onset of COVID-19. This study also highlights the increased prevalence and significance of moral injuries within this population. Such issues could lead to a decrease in the quality of care provided to the general public, ultimately impacting overall public health (49). Further research is needed to develop effective policies to mitigate the consequences of high rates of moral injury among HCPs. Researchers and policymakers should take appropriate measures to assess the severity and scope of the problem and work on prevention and resolution strategies for future pandemics, which could be even more widespread and severe. Regular therapy visits, reassurance from expert psychologists, and mindfulness training are examples of interventions that have been successful in reducing psychological complications during other pandemics (43, 50).