1. Background
Cardiovascular disease, particularly coronary artery disease (CAD), is a major global health concern and a leading cause of mortality worldwide (1). The CAD occurs when the coronary arteries become narrowed or blocked, typically due to atherosclerosis (2). Cardiovascular diseases, primarily CAD, account for approximately one-third of all deaths globally (3).
The pathology of CAD encompasses a broad range of processes, including dyslipidemia, thrombosis, inflammation, activation of vascular smooth muscle cells, platelet activation, endothelial dysfunction, oxidative stress, and altered matrix metabolism (4). Major risk factors include behavioral factors such as immobility and smoking, as well as metabolic risks like hyperglycemia and hypercholesterolemia (5). Additionally, CAD is significantly influenced by age, gender, and socioeconomic status (6).
The CAD has a profound impact on patients’ personal and social lives, often leading to chronic and progressive complications (7). Functional disability (FD) is a major concern, defined as limitations in physical, personal, or social activities due to health conditions and environmental factors (8). Patients with functional somatic syndromes (FSS) often experience a range of physical symptoms, such as chronic pain, fatigue, and gastrointestinal disturbances, without a clear underlying medical cause (9). While the prevalence of FSS varies across different populations, it is estimated to affect a significant portion of the general population (10). According to the World Health Organization, FD refers to any long-term limitation in daily activities resulting from health conditions (11). The CAD-induced FD affects multiple aspects of life, including physical, mental, educational, and social domains (12), and may manifest as functional physical syndromes (13). Patients with CAD frequently experience symptoms such as chest pain, shortness of breath, and fatigue, all of which significantly impact their functional ability and quality of life (14). This syndrome, also known as medically unexplained physical syndrome, includes conditions such as chronic fatigue syndrome, irritable bowel syndrome, chronic pelvic pain, and deep and rapid breathing syndrome (15). The co-occurrence of FSS and CAD presents unique challenges in patient management and rehabilitation (16).
Certain PTs, such as neuroticism and introversion, have been associated with an increased risk of developing FSS and poorer health outcomes in patients with CAD (17). The PTs play a crucial role in patients’ perceived FD. The PTs are stable patterns of thinking, emotion, and behavior that interact with environmental factors to influence lifestyle and coping mechanisms (18, 19). Certain PTs, such as conscientiousness, are known to significantly impact medical treatment outcomes (20). Moreover, patients with maladaptive illness perceptions (IPs) may experience poorer health outcomes and increased FD (21).
The IP is another critical psycho-behavioral factor affecting medical help-seeking behavior and FD (22). The IP refers to patients’ cognitive appraisal and interpretation of their illness, including its causes, outcomes, signs, and symptoms (23). Patients’ perceptions of their illness influence their physical and mental health, coping abilities (24), and illness-related behaviors such as treatment adherence (25). The IP is shaped by various factors, including physical conditions, financial status, social power, and cultural background (26).
Self-compassion (SC) can also influence FD among CAD patients. The SC involves kindness, care, and acceptance toward oneself, coupled with an unbiased attitude toward personal deficits and failures (27, 28). The construct of SC includes three main components: Self-kindness versus self-judgment, common humanity versus isolation, and mindfulness versus over-identification (29). The SC helps individuals approach their difficulties with kindness rather than self-criticism (30, 31). It enhances coping abilities and necessitates a balanced approach to negative self-feelings (32, 33).
Previous studies have highlighted significant relationships between PTs and IP among various populations, including patients with multiple sclerosis (34), CAD (35), and students (25). Additionally, research has shown significant connections between PTs and SC. For instance, SC-focused therapy has been found to positively impact treatment adherence and components of type D personality among CAD patients (36). Other studies have demonstrated significant relationships between IP, coping strategies, and social support among CAD patients (25), as well as between SC and FD among adults with chronic pain (15). Furthermore, research has identified associations among mindfulness, SC, PTSD symptoms, and FD in American veterans (12).
The SC, defined as the ability to extend kindness and understanding toward oneself in the face of suffering or failure (27), has emerged as a potential factor in the management of chronic health conditions. Higher levels of SC have been associated with improved psychological well-being, reduced stress, and better health outcomes across various populations (37). The SC may serve as a mediator between PTs, IP, and FD in patients with FSS and CAD by influencing how individuals cope with their illness and manage their symptoms (38).
2. Objectives
While previous studies have explored the direct connections between FD and various factors, there remains a noticeable gap in research regarding the interplay between predictor variables such as PTs and SC with FD. Additionally, there is limited information on the structural relationships and mediating functions of these variables among patients with CAD. To bridge these gaps, this study seeks to examine a structural model that predicts FD in FSS by considering the influence of PTs and IP, with SC acting as a mediator.
3. Methods
This applied cross-sectional correlational study was conducted in 2022 using structural equation modeling.
3.1. Participants and Setting
The statistical population of this study consisted of patients with CAD in Amol, Iran. Participants included 250 patients recruited through purposive sampling. Inclusion criteria for the study included patients diagnosed with CAD, aged between 18 and 80, able to understand and communicate in the local language, and willing to provide informed consent. Exclusion criteria included patients with severe cognitive impairment or psychiatric disorders, a history of neurological disorders, severe comorbidities, recent major surgical interventions, a history of substance abuse, physical limitations preventing completion of study questionnaires, and those who declined or withdrew consent during the study. A sample size of 200 participants is generally considered sufficient for most quantitative research studies, as supported by several guidelines and recommendations from the scientific literature (39).
3.2. Data Collection Instruments
Instruments for data collection included the World Health Organization disability assessment schedule, Traits Personality Questionnaire, Brief Illness Perception Questionnaire, and Self-compassion Scale.
3.2.1. The World Health Organization Disability Assessment Schedule
The World Health Organization introduced the second version of this questionnaire in 2014. The twelve items of this instrument are scored as follows: (1) “None”; (2) “mild”; (3) “moderate”; (4) “severe”; and (5) “extreme or cannot do” (5). Higher scores on this instrument indicate greater FD. A study confirmed the acceptable content and construct validity of the instrument and reported a Cronbach’s alpha of 0.98 (40). Another study examining the psychometric properties of the Persian version of this instrument also confirmed its content and concurrent validity and found that its Cronbach’s alpha was 0.82 (41).
3.2.2. The Traits Personality Questionnaire
McCrae and Costa developed this questionnaire with sixty items categorized into five twelve-item PTs: Neuroticism, extraversion, openness to experience, agreeableness, and conscientiousness. Item scoring is performed on a five-point Likert scale as follows: (0) “Strongly disagree”; (1) “disagree”; (2) “indifferent”; (3) “agree”; and (4) “strongly agree”. McCrae and Costa reported that this questionnaire had acceptable content and construct validity, as well as reliability, with Cronbach’s alpha values ranging from 0.79 to 0.88 (42). Similarly, a study found that its Persian version had acceptable content and construct validity and reliability, with Cronbach’s alpha values ranging from 0.56 to 0.87 (43). In the present study, the Cronbach’s alpha values of the neuroticism, extraversion, openness to experience, agreeableness, and conscientiousness subscales of the questionnaire were 0.84, 0.82, 0.87, 0.79, and 0.83, respectively, confirming its acceptable reliability.
3.2.3. The Brief Illness Perception Questionnaire
Broadbent et al. developed this questionnaire with nine items. Items 1 - 8 are scored on a scale of 0 - 90, while item 9 is an open-ended question regarding the three main causes of illness. The developers confirmed the acceptable content and construct validity of the questionnaire and reported a Cronbach’s alpha of 0.86 (44). A study conducted in Iran also validated its content and concurrent validity, with a Cronbach’s alpha of 0.80 and a test-retest correlation coefficient of 0.75 (45). In the present study, the Cronbach’s alpha of the questionnaire was 0.88.
3.2.4. The Self-compassion Scale
Neff developed this scale with 26 items distributed across six subscales: Self-kindness (five items) vs. self-judgment (five items), common humanity (four items) vs. isolation (four items), and mindfulness (four items) vs. over-identification (four items). The subscales of self-judgment, isolation, and over-identification have negative connotations, with their scores inversely correlated with those of self-kindness, common humanity, and mindfulness. Items are rated on a Likert-type scale, where higher scores indicate greater SC. The scale’s developer confirmed its acceptable content and construct validity and reported Cronbach’s alpha values for the subscales ranging from 0.81 to 0.92 (46). Similarly, a study conducted in Iran verified its content and construct validity (47). In the present study, the Cronbach’s alpha values for the subscales ranged from 0.74 to 0.82, confirming the reliability of the scale.
3.3. Data Analysis
Normality was tested using the energy test of multivariate normality (48). Latent-variable structural equation modeling was employed for data analysis to assess the relationships among latent variables and measured variables, as well as the relationships among latent variables. Model fit indices were calculated to evaluate the adequacy of the structural model. These indices included chi-square divided by the degree of freedom (CMIN/DF), root mean square error of approximation (RMSEA), Comparative Fit Index (CFI), Normed Fit Index (NFI), Tucker-Lewis Index (TLI), and Incremental Fit Index (IFI) (49). The relationships among the variables were then examined. The data analysis was conducted using SPSS (V. 26.0), Amos (V. 24), and R (the lavaan and mvnormtest packages; V. 4.2.0). The level of significance for all statistical analyses was set at less than 0.05.
3.4. Ethical Approval
The Ethics Council of the Islamic Azad University Research Committee approved the present study (IR.IAU.TON.REC.1401.069). A key ethical consideration was the protection of patient confidentiality and privacy. Given that the study involved patients with CAD, it was essential to ensure that their personal information and medical history were handled with the highest level of confidentiality. This involved obtaining informed consent from all participants, securely storing and anonymizing their data, and presenting the results in a manner that prevented the identification of individual patients. Upholding ethical standards by maintaining patient privacy and confidentiality was fundamental to ensuring trust in the scientific community and the integrity of the research process.
4. Results
4.1. Descriptive Statistics Findings
The mean scores of FD and IP were 36.48 ± 8.13 and 44.98 ± 10.91, respectively. The mean scores for PTs were as follows: Neuroticism, 29.50 ± 6.30; extraversion, 34.67 ± 7.98; openness to experience, 35.09 ± 5.86; agreeableness, 30.51 ± 6.79; and conscientiousness, 34.84 ± 7.44. Additionally, the mean scores for the SC subscales were: Self-kindness, 15.42 ± 4.01; common humanity, 14.84 ± 3.59; mindfulness, 13.60 ± 3.19; self-judgment, 13.29 ± 4.21; isolation, 11.59 ± 3.96; and over-identification, 11.83 ± 3.76 (Table 1).
| Variables and Subscales | Mean ± SD | Range | Kurtosis | Skewness |
|---|---|---|---|---|
| FD | 36.48 ± 8.13 | 16 - 58 | -0.44 | -0.09 |
| PTs | ||||
| Neuroticism | 29.50 ± 6.30 | 11 - 47 | -24.0 | 0.05 |
| Extraversion | 34.67 ± 7.98 | 9 - 60 | 0.71 | 0.18 |
| Openness to experience | 35.09 ± 5.86 | 20 - 51 | -0.22 | 0.08 |
| Agreeableness | 30.51 ± 6.79 | 15 - 49 | -0.63 | 0.00 |
| Conscientiousness | 34.84 ± 7.44 | 16 - 58 | 0.14 | 0.05 |
| IP | 44.98 ± 10.91 | 19 - 72 | -0.20 | 0.12 |
| SC | ||||
| Self-kindness | 15.42 ± 4.01 | 5 - 25 | -0.22 | 0.01 |
| Common humanity | 14.84 ± 3.59 | 4 - 25 | 0.89 | -0.02 |
| Mindfulness | 13.60 ± 3.19 | 4 - 20 | -0.29 | 0.01 |
| Judgment | 13.29 ± 4.21 | 4 - 19 | -0.36 | -0.17 |
| Isolation | 11.59 ± 3.96 | 4 - 20 | -0.24 | 0.04 |
| Over-identification | 11.83 ± 3.76 | 5 -20 | -0.05 | 0.15 |
Abbreviations: FD, functional disability; PTs, personality traits; IP, illness perception; SC, self-compassion.
4.2. Inferential Statistics Findings
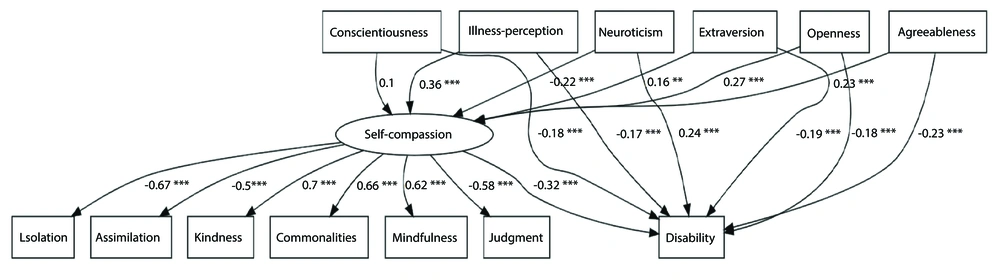
Normality testing indicated that the study variables followed a normal distribution (MVE = 1.42; P = 0.80). Therefore, covariance-based structural equation modeling (CB-SEM) was deemed appropriate. The CMIN/DF was 0.98, and other model fit indices confirmed the good fit of the structural model predicting FD based on PTs and IP with SC as a mediator (Table 2). The structural model is depicted in Figure 1.
| Indices | Values | Acceptable Values |
|---|---|---|
| CMIN/DF | 0.98 | < 3 |
| RMSEA | 0.03 | < 0.08 |
| CFI | 0.99 | > 0.9 |
| NFI | 0.95 | > 0.9 |
| TLI | 0.99 | > 0.9 |
| IFI | 0.98 | > 0.9 |
Abbreviations: CMIN/DF, chi-square divided by degree of freedom; RMSEA, root mean square error of approximation; CFI, Comparative Fit Index; NFI, Normed Fit Index; TLI, Tucker-Lewis Index; IFI, Incremental Fit Index.
The structural equation model demonstrated that IP, SC, and all five PTs collectively explained a substantial 70% of the variance in FD among patients with functional somatic syndrome and CAD (P < 0.05). This indicates that these psychological factors play a major role in determining disability levels in this population.
Importantly, SC was found to significantly mediate the relationships between FD and both IP and several key PTs, including neuroticism, extraversion, openness to experience, and agreeableness. This suggests that SC is a critical mechanism through which these variables influence functional outcomes.
The strongest coefficient was observed for IP (0.11), indicating that higher levels of maladaptive IPs were most strongly associated with greater FD, with this relationship mediated by SC (P < 0.05; Table 3).
| Criterion and Predictor Variables | Mediating Variables | Effect | z | P-Value |
|---|---|---|---|---|
| SC | ||||
| Neuroticism | - | -0.22 | -4.10 | 0.001 |
| Extraversion | - | 0.15 | -2.93 | 0.001 |
| Openness to experience | - | 0.27 | 5.01 | 0.001 |
| Agreeableness | - | 0.22 | 4.14 | 0.001 |
| Conscientiousness | - | 0.10 | 1.87 | 0.07 |
| IP | - | 0.36 | 6.35 | 0.001 |
| FD | ||||
| Neuroticism | - | 0.23 | 6.71 | 0.001 |
| Extraversion | - | -0.19 | -5.62 | 0.001 |
| Openness to experience | - | -0.18 | -5.01 | 0.001 |
| Agreeableness | - | -0.23 | -6.60 | 0.001 |
| Conscientiousness | - | -0.18 | -5.51 | 0.001 |
| IP | - | -0.32 | -5.53 | 0.001 |
| SC | - | -0.17 | -4.45 | 0.001 |
| Neuroticism | SC | 0.07 | -3.43 | 0.001 |
| Extraversion | SC | -0.05 | -2.65 | 0.001 |
| Openness to experience | SC | -0.09 | -3.91 | 0.001 |
| Agreeableness | SC | -0.07 | -3.45 | 0.001 |
| Conscientiousness | SC | -0.03 | 1.74 | 0.07 |
| IP | SC | -0.11 | -4.45 | 0.001 |
Abbreviations: SC, self-compassion; IP, illness perception; FD, functional disability.
5. Discussion
The results of this study indicate a significant relationship between IP, SC, PTs, and FD among patients with CAD. The use of CB-SEM is appropriate for analyzing these complex relationships, as it allows for the examination of both direct and indirect effects among variables. The model fit indices, including a CMIN/DF of 0.98, suggest a good fit for the structural model, confirming that the hypothesized relationships are supported by the data. This aligns with the findings of Zhang et al., who emphasize the importance of model fit indices in validating structural equation models, particularly in health-related research (50).
The finding that IP, SC, and the five PTs collectively explain 70% of the variance in FD is significant. This high percentage indicates that these variables are critical in understanding the factors contributing to FD in CAD patients. Previous research has shown that maladaptive IPs can lead to poorer health outcomes and increased disability (21). Our results reinforce this notion, particularly with IP showing the strongest coefficient (0.11), suggesting that higher levels of maladaptive IP are associated with greater FD, mediated by SC. This is consistent with the work of Sirois et al., who found that SC can play a crucial role in how individuals cope with chronic health conditions, thereby influencing their functional outcomes (38)
Our study found that PTs had a significant direct relationship with FD. Specifically, neuroticism was positively related to FD, while the other four PTs showed an inverse relationship with FD. This suggests that individuals with higher neuroticism — characterized by traits such as anxiety and depression — tend to experience greater functional limitations in their daily activities. This finding is consistent with research indicating that negative affect is associated with increased FD in cancer patients (35).
The analysis revealed that agreeableness was significantly associated with FD, showing an inverse relationship. This finding suggests that patients who exhibit higher levels of agreeableness, characterized by traits such as cooperation and compassion, tend to experience lower levels of FD. However, it is important to clarify that while agreeableness may contribute to positive interpersonal relationships and social support, it does not directly equate to an individual’s overall coping ability.
Previous research has also supported the relationship between PTs and various outcomes such as anxiety and self-care behaviors (35). Therefore, the type of interaction individuals have with their environment can significantly influence their experience of illness, with introverted and highly neurotic individuals experiencing higher FD. Furthermore, our study found that PTs, especially neuroticism and agreeableness, have an indirect influence on FD through SC. This aligns with research suggesting that higher SC and stable interpersonal relationships contribute to better occupational functioning and lower job burnout (51).
The finding that IP, SC, and the five PTs explained 70% of the variance in FD is consistent with previous studies that highlight the significant impact of psychological factors on health outcomes. For instance, Razaghpour et al. demonstrated that PTs and IP significantly predicted FD in patients with CAD, emphasizing the importance of these factors in understanding patient experiences and outcomes. Their study supports our findings, particularly regarding the role of maladaptive IPs in exacerbating FD (52).
Moreover, the significant mediating role of SC in the relationship between IP and FD aligns with the work of Sirois et al., who found that SC can buffer the negative effects of stress and maladaptive coping strategies in individuals with chronic health conditions (38). This suggests that interventions aimed at enhancing SC could be beneficial in reducing FD among patients with CAD and functional somatic syndrome.
The strongest coefficient observed for IP (0.11) further underscores the critical role of IP in predicting FD. This finding is supported by Hagger and Orbell, who conducted a meta-analysis demonstrating that negative IPs are associated with poorer health outcomes across various chronic conditions (21). By highlighting the connection between maladaptive IPs and increased FD, our study contributes to the growing body of literature that advocates for addressing psychological factors in the management of chronic diseases.
Additionally, the integration of PTs into our model reflects the findings of Burton et al. (as cited by Rohricht et al.), who proposed an integrated care pathway for patients with functional somatic disorders, emphasizing the need to consider both psychological and physical health factors in treatment (53). Their work suggests that understanding the interplay between PTs and functional outcomes can lead to more effective, tailored interventions for patients facing similar challenges.
Moreover, the significant mediating role of SC in the relationships between FD and IP, as well as between FD and several PTs (neuroticism, extraversion, openness to experience, and agreeableness), underscores the multifaceted nature of these interactions. The literature supports the notion that SC can mitigate the negative effects of PTs on health outcomes (37). For instance, individuals with high neuroticism may experience greater psychological distress, leading to increased FD; however, higher SC can buffer these effects, promoting better coping strategies.
Additionally, our findings revealed that IP had a significant inverse direct relationship with FD and an indirect relationship through SC. Individuals with higher IP tended to experience lower FD, a result consistent with several studies (54, 55). Furthermore, SC was inversely related to FD, suggesting that higher levels of SC were associated with reduced FD among CAD patients. This supports the findings of previous studies highlighting the role of SC in mitigating FD (12, 15, 36). Therefore, a better understanding of one’s illness can enhance SC and reduce FD in CAD patients.
5.1. Clinical Implications
- A holistic assessment should be integrated into the clinical management of CAD patients, considering PTs, IPs, and SC.
- The SC interventions may enhance psychological well-being in CAD patients, with potential benefits from incorporating SC training into rehabilitation programs.
- Personalized care plans based on individual PTs may improve treatment adherence and overall health outcomes.
- Psychoeducation on IPs can encourage patients to actively participate in their health management and improve coping mechanisms.
- Multidisciplinary collaboration among cardiologists, psychologists, and rehabilitation specialists is crucial for addressing both the physical and psychological aspects of CAD.
- Further research is needed to explore the complex interplay between PTs, IP, SC, and FD in CAD and other chronic conditions.
5.2. Conclusions
This study demonstrates that PTs, IP, and SC are significant predictors of FD in CAD patients with functional somatic syndrome. Additionally, SC mediates the effects of PTs and IP on FD, underscoring its importance in patient care and intervention strategies.
5.3. Limitations
The cross-sectional design restricts the ability to infer causality; future longitudinal studies are needed to establish temporal relationships.
Self-reported measures may introduce bias due to subjectivity, necessitating the use of objective assessments in future research. The sample size and diversity may limit generalizability; larger and more diverse populations should be considered in subsequent studies. Additional psychosocial factors, such as coping strategies and social support, were not included in the model but may significantly impact FD in CAD patients. Future studies should integrate these factors for a more comprehensive understanding.