1. Background
Suicide represents a serious global public health issue (1), defined as the intentional act of ending one’s own life (2). It remains a leading cause of death worldwide and significantly contributes to the overall disease burden (3). According to the World Health Organization (WHO), suicide accounts for the largest share of intentional injuries in developed countries (4). Annually, over 700,000 people globally lose their lives to suicide, making it the fourth leading cause of death among young people aged 15 to 29 (1).
In 2017, the estimated suicide rate in Iran was approximately 9.9 deaths per 100,000 individuals (5). Studies report a concerning prevalence of suicide attempts among Iranian students, ranging from 1.8% to 3.5%, with suicidal ideation rates between 6.2% and 42.7% (6). According to Yasamy et al., students rank second, after housewives, in terms of suicide attempt rates (7). Suicidal behaviors are typically classified into three categories: Suicidal ideation (thoughts of ending one’s life), suicide plans (formulating a specific method), and suicide attempts (engaging in self-injurious behavior with some intent to die) (3).
Suicide is a complex, multi-faceted phenomenon that arises from the interaction of various factors (8). Theorists like Beck have emphasized the role of hopelessness (9), while Shneidman has pointed to severe psychological pain (psychic pain) (10), and Durkheim highlighted the role of social isolation (11). Other factors, such as impulsivity (12), psychiatric disorders (13), and anhedonia (14), have also been identified as serious risk factors. While these theories have been useful for guiding suicide research and prevention, they share a limitation: They do not differentiate between suicidal thoughts and suicidal behaviors (15).
One reason for the limited understanding of suicide risk factors is the insufficient knowledge of the transition from suicidal ideation to action (16). Thomas Joiner's Interpersonal Theory of Suicide (IPTS) introduced a new generation of theories that utilize the "ideation-to-action" framework. These theories differentiate between the development of suicidal thoughts and the progression from ideation to action, recognizing them as distinct processes (15). Joiner's theory suggests that having suicidal thoughts does not necessarily indicate a risk for suicide; the factors influencing ideation may differ from those influencing suicidal behavior (17). According to this theory, suicidal behavior is driven by three key components: Thwarted belongingness, perceived burdensomeness (both contributing to suicidal desire), and acquired capability for suicide, which leads to action (18).
O'Connor’s Integrated Motivational-Volitional (IMV) theory (2011) is another "ideation-to-action" framework. It posits that feelings of defeat and entrapment contribute to suicidal ideation, while the capacity for suicidal action, along with factors such as impulsivity and access to means, drives the transition from thoughts to behavior (19). The most recent theory within this framework is the Three-Step Theory of suicide (3ST) by Klonsky and May (2015), which explains suicidal thoughts and behaviors through four factors: Pain, hopelessness, connectedness, and capacity for suicide (15).
In summary, the 3ST posits: (a) suicidal thoughts arise from high levels of pain and hopelessness (pain being the experience of mental or emotional suffering, and hopelessness being the belief that this pain will never end); (b) connectedness (to loved ones, valued roles, or a sense of meaning or purpose) serves as a protective factor against the intensification of suicidal ideation in individuals experiencing both pain and hopelessness; (c) the transition from ideation to action occurs when an individual develops the capacity to overcome the inherent pain and fear of death (capacity for suicide), which refers to an individual's habituation to pain and death through life experiences (15). In this study, we consider "low connectedness" (or low belongingness) as a factor that intensifies suicidal thoughts.
While the Three-Step Theory of Suicide shares similarities with Joiner’s Interpersonal Theory (2005), such as the role of thwarted belongingness and acquired capability for suicide, it places a greater emphasis on pain and hopelessness in forming suicidal ideation. These constructs are broader than the thwarted belongingness and perceived burdensomeness described in the interpersonal theory. Additionally, pain and hopelessness have numerous potential causes beyond perceived burdensomeness and thwarted belongingness (20). The simplicity of the 3ST structure not only encompasses a wide range of risk factors but also helps explain the mechanisms through which these factors influence suicide risk (21).
2. Objectives
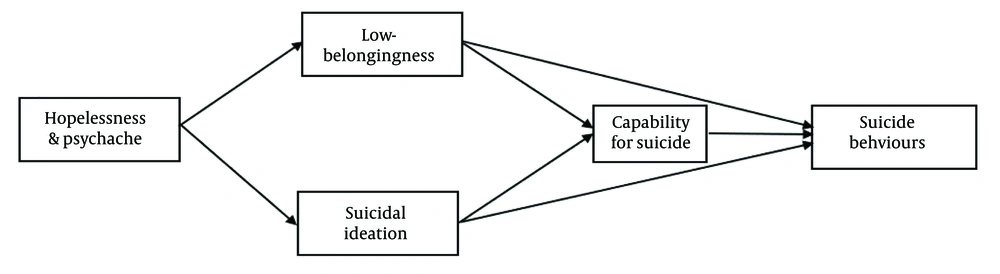
Given the significant impact of suicide, particularly within student populations, and recognizing the Three-Step Theory of Suicide as a relatively new framework, this study aims to explore the structural dynamics of suicide using the 3ST in an Iranian student population. This research seeks to contribute to the development of a practical model for mitigating suicidal ideation and behaviors among students. Figure 1 provides a graphical representation of the hypothetical theoretical model.
3. Methods
3.1. Participants
This cross-sectional study aimed to describe and analyze simple and multivariable relationships using structural equation modeling (SEM). The study population consisted of all students enrolled at Zanjan University of Medical Sciences. Prior to completing the questionnaires, informed virtual consent was obtained from all participants. Based on the sample size estimation method for SEM, 260 students were selected using a convenience sampling method (22). Participants ranged in age from 18 to 52 years (mean: 23.62, standard deviation: 5.48), with 75.8% (n = 197) being female. Of the participants, 13.5% (n = 35) were married, 85% (n = 221) were single, and 1.5% (n = 4) were divorced. In terms of educational level, 67.7% were undergraduates, and 32.3% were postgraduates.
3.2. Procedure
The study was approved by the Ethics Committee of Zanjan University of Medical Sciences (IR.ZUMS.REC.1401.258). Online questionnaires were used, and the Symptom Checklist-25 (SCL-25) was employed to identify individuals without psychiatric disorders (mean score < 4). Based on this criterion, nine individuals with scores above 3 were excluded from the study. Additionally, a single question on suicide attempts was included, and 110 individuals who had attempted suicide were excluded. Participants were informed about the voluntary nature of the study, anonymity, and confidentiality, and were given the option to withdraw at any time. They were also encouraged to contact the researchers with any questions about the questionnaire or if they were interested in the survey results. To maintain anonymity and confidentiality, non-identifying codes were used for the questionnaires.
3.3. Instruments
3.3.1. Symptom Checklist-25
The SCL-25, developed by Najarian and Davoodi, is a shortened version of the SCL-90 used to assess general psychopathologies. The 5-point Likert scale demonstrated a strong correlation (0.95) with the SCL-90 and an internal consistency of 0.97 for females and 0.98 for males (23). In this study, Cronbach's alpha was 0.923.
3.3.2. Suicide Behaviors Questionnaire-Revised (SBQ-R)
The SBQ-R is a four-item self-report questionnaire that evaluates lifetime suicidal behavior, suicidal ideation in the past 12 months, suicide threat, and the likelihood of future suicidal behavior (24). Scores range from 3 to 18, with higher scores indicating greater suicidal risk. The psychometric properties of this questionnaire have been validated in previous studies (25, 26).
3.3.3. Suicide Attempt
To assess suicide attempts, a question adapted from Dhingra et al. (27) was used: "How many times have you attempted to end your life with the intention of dying?" Responses ranged from "None" to "5 times or more."
3.3.4. Beck Scale for Suicidal Ideation (BSSI)
The BSSI assesses and quantifies the severity of suicidal ideations and behaviors. It consists of 19 questions, each scored from 0 to 2, with a total score range of 0 to 38. The scale has high validity and reliability for detecting suicidal ideation (28) and has been validated for use in the Iranian community (29).
3.3.5. Inventory of Motivations for Suicide Attempts (IMSA)
The IMSA is a 54-item self-report questionnaire designed to evaluate motivations for suicide as outlined by major suicide theories. Responses are rated on a 5-point Likert scale. The IMSA includes nine scales with five items each, plus nine additional items (30). This questionnaire was used to assess levels of pain, hopelessness, and low belongingness. Previous studies have validated the psychometric properties of the IMSA (31, 32).
3.3.6. Acquired Capability for Suicide Scale (ACSS)
The ACSS, developed by Van Orden, is a 20-item self-report measure assessing the acquired capability for suicide. Items are rated on a 5-point Likert scale, but only seven items demonstrated adequate reliability in previous research (33). The remaining questions were removed. The Cronbach's alpha of this scale was 0.72 in previous studies (34).
3.3.7. Data Analysis
The quality of the measurement model was assessed through reliability and validity analyses. Cronbach's alpha was calculated using SPSS 24 software to evaluate reliability, while confirmatory factor analysis (CFA) was conducted with AMOS 24 to evaluate validity. Descriptive statistics, including mean and standard deviation, were also reported using SPSS 24. To investigate relationships between the constructs, a structural equation model was applied using AMOS 24. Pearson correlation coefficients were calculated to determine the strength of the relationships between factors. Structural equation modeling with maximum likelihood was used to examine the mediating role of low belongingness and suicidal ideation in the relationship between pain, hopelessness, and suicidal behaviors. Standardized path coefficients were calculated to measure the strength of relationships between variables.
Model fit was assessed using several indicators, including the root mean square error of approximation (RMSEA), Comparative Fit Index (CFI), Tucker Lewis Index (TLI), Goodness of fit Index (GFI), Adjusted Goodness of Fit Index (AGFI), and chi-square statistic (χ2)/degrees of freedom (df) (CMIN/DF). Models with RMSEA < 0.08, CFI > 0.90, TLI > 0.90, GFI > 0.95, AGFI > 0.80, and CMIN/DF < 5 were considered well-fitting. The significance of the mediating effects of low belongingness and suicidal ideation was evaluated using the bootstrap method. Bootstrapping involves resampling the original dataset with replacement to generate a distribution of simulated datasets. A total of 5000 bootstrap samples were created, and 95% confidence intervals (CI) were calculated. If the 95% CI did not include 0, the mediating effects were considered significant. Statistical significance was set at P < 0.05 and P < 0.01.
4. Results
Descriptive analysis and correlations between overall variable. The means, standard deviations, and correlations between the variables are presented in Table 1.
| Scale | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Cronbach's Alpha |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Hopelessness | 9.86 | 6.50 | 1 | 0.870 a | 0.810 a | 0.276 a | 0.304 a | 0.163 a | 0.219 a | -0.032 | 0.397 a | 0.877 |
| 2. Pain | 8.30 | 5.75 | 1 | 0.810 a | 0.286 a | 0.314 a | 0.162 b | 0.241 a | -0.001 | 0.364 a | 0.901 | |
| 3. Low-belongingness | 5.86 | 4.47 | 1 | 0.232 a | 0.246 a | 0.144 b | 0.209 a | -0.070 | 0.273 a | 0.846 | ||
| 4. BSSI | 3.79 | 6.25 | 1 | 0.979 a | 0.744 a | 0.918 a | 0.258 a | 0.627 a | 0.934 | |||
| 5. BSSI-ASD | 1.88 | 3.98 | 1 | 0.640 a | 0.867 a | 0.266 a | 0.629 a | 0.834 | ||||
| 6. BSSI-P | 0.288 | 0.992 | 1 | 0.608 a | 0.232 a | 0.423 a | 0.921 | |||||
| 7. BSSI- PSD | 1.60 | 1.95 | 1 | 0.178 a | 0.572 a | 0.736 | ||||||
| 8. ACS | 37.07 | 11.50 | 1 | 0.199 a | 0.837 | |||||||
| 9. SBQ-R | 5.80 | 6.35 | 1 | 0.993 |
Abbreviations: M, mean; SD, standard deviation; BSSI, Beck Scale for suicidal ideation; ASD, active suicidal desire; P, preparation; PSD, passive suicidal desire; ACS, acquired capability for suicide; SBQ-R, Suicide Behaviors Questionnaire-Revised.
a P < 0.01.
b P < 0.05.
The data show that hopelessness and pain are significantly and strongly positively correlated with low belongingness (r = 0.810, P < 0.001) and weakly positively correlated with suicidal ideation (r = 0.276, 0.286, P < 0.001). Additionally, there is a weak positive correlation with suicidal behaviors (r = 0.397, 0.364, P < 0.001). Moreover, a significant weak positive correlation was observed between low belongingness and both suicidal ideation (r = 0.232, P < 0.001) and suicidal behaviors (r = 0.273, P < 0.001).
A weak positive correlation was also noted between capability for suicide and both suicidal ideation (r = 0.258, P < 0.001) and suicidal behaviors (r = 0.199, P < 0.001). Furthermore, a strong positive correlation was found between suicidal ideation and suicidal behaviors (r = 0.627, P < 0.001). These results are detailed in Table 1.
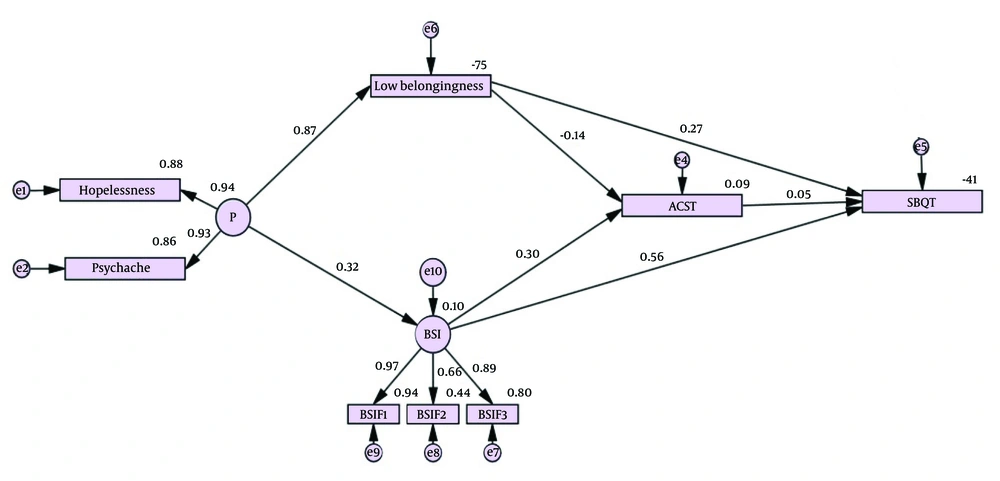
Structural equation modeling model results: The findings from the SEM analysis are summarized in Table 2. The fit indices for the theoretical model were: Chi-square statistic (χ²)/degrees of freedom (CMIN/DF) = 1.505, RMSEA = 0.044, CFI = 0.995, TLI = 0.990, GFI = 0.980, and AGFI = 0.951, indicating a strong model fit (35). A higher standardized path coefficient reflects a stronger correlation between variables, with values exceeding 0.200 considered indicative of a strong correlation.
| Effect and Path | Estimate | C.R | P-Value | 95% Confidence Intervals | |
|---|---|---|---|---|---|
| Lower Bounds | Upper Bounds | ||||
| Direct | |||||
| H&P → BSSI | 0.318 | 4.991 | < 0.001 | 0.199 | 0.425 |
| H&P → L-B | 0.867 | 21.952 | < 0.001 | 0.817 | 0.910 |
| BSSI → ACS | 0.300 | 4.672 | < 0.001 | 0.177 | 0.416 |
| L-B → ACS | -0.145 | -2.334 | 0.031 | -0.277 | -0.010 |
| BSSI → SBQ | 0.556 | 10.119 | < 0.001 | 0.419 | 0.685 |
| L-B → SBQ | 0.226 | 4.318 | < 0.001 | 0.136 | 0.398 |
| ACS → SBQ | 0.047 | .969 | 0.380 | -0.057 | 0.148 |
| Indirect | |||||
| H&P → ACS | -0.030 | 0.633 | -0.151 | 0.090 | |
| H&P → SBQ | 0.406 | < 0.001 | 0.292 | 0.510 | |
| BSSI → SBQ | 0.014 | 0.380 | -0.018 | 0.044 | |
| L-B → SBQ | -0.007 | 0.405 | -0.024 | 0.010 | |
| Total | |||||
| H&P → ACS | -0.030 | 0.633 | -0.151 | 0.090 | |
| H&P → SBQ | 0.406 | < 0.001 | 0.292 | 0.510 | |
Abbreviations: C.R, critical ratio; H&P, hopelessness & pain; BSSI, Beck Scale for suicidal ideation; L-B, low-belongingness; SBQ-R, Suicide Behaviours Questionnaire-Revised; ACS, acquired capability for suicide.
In the SEM model, the variables displayed significant inter-correlations. The standardized path coefficient for the path from hopelessness & pain (H&P) to suicidal ideation was 0.318, indicating that a one standard deviation increase in H&P led to a 0.318 standard deviation increase in BSSI, demonstrating that hopelessness and pain positively predict suicidal ideation. Similarly, a one standard deviation increase in H&P resulted in a 0.867 standard deviation increase in low belongingness (L-B), indicating that hopelessness and pain positively predict low belongingness.
The path from suicidal ideation to capability for suicide (ACS) had a coefficient of 0.300, indicating that suicidal ideation positively predicts the capability for suicide. Conversely, the path from low belongingness (L-B) to ACS showed a coefficient of -0.145, demonstrating that low belongingness negatively predicts capability for suicide in the student sample.
The model also showed that both suicidal ideation and low belongingness positively predict suicidal behaviors (β = 0.556, 0.226, P < 0.001). However, capability for suicide did not have a predictive effect on suicidal behaviors in the student sample. All paths were statistically significant (P < 0.01). Additionally, the indirect association between hopelessness & pain and suicidal behaviors (SBQT) was 0.406 and significant (P < 0.01). The final model is presented in Figure 2.
5. Discussion
The present study aimed to investigate the structural factors influencing suicidal behavior among Iranian students, using the conceptual framework provided by the Three-Step Theory of Suicide. The results showed that the combination of pain and hopelessness directly affects suicidal ideation (β = 0.318, P < 0.001) and predicts low belongingness (β = 0.867, P < 0.001). Additionally, the combination of pain and hopelessness indirectly influences suicidal behavior through the pathways of low belongingness, capability for suicide, and suicidal ideation (β = 0.406, P < 0.001). Both low belongingness and suicidal ideation individually and directly predict suicidal behavior (β = 0.226, 0.556, P < 0.001). However, they do not indirectly predict suicidal behavior through the capability for suicide, and the capability for suicide itself does not predict suicidal behavior in this sample.
The first stage of the 3ST posits that suicidal ideation arises from the simultaneous presence of pain and hopelessness. This principle was supported in this study, aligning with previous findings (36-39). Several studies have also highlighted the role of pain and hopelessness in generating suicidal thoughts. For instance, Montemarano’s four-year longitudinal study demonstrated that pain is a strong predictor of suicidal ideation (40). Another longitudinal study over four weeks indicated that hopelessness predicts suicidal ideation (41). In a study conducted in Iran, a noteworthy correlation was observed between hopelessness and suicidal thoughts among students with low resilience (42). Additionally, hope has been identified as a deterrent against suicidal ideation and behavior (43). In this study, the simultaneous presence of pain and hopelessness was found to significantly increase the risk of suicidal ideation among students, confirming the first assumption of the 3ST.
Pain and hopelessness were also found to have a strong positive relationship with low belongingness among students. Dhingra et al. (2019) reported similar findings, showing a strong positive relationship between pain, hopelessness, and low belongingness among students (36). This result was also corroborated by several other studies (38, 39, 44). These findings suggest that as individuals experience more pain and hopelessness, their sense of connectedness to others or society diminishes.
The results indicated that suicidal ideation directly predicts suicidal behavior, consistent with other studies conducted in Iranian women (45) and in a cohort of depressed individuals in the Netherlands, which demonstrated a similar relationship (46).
In the second stage of the 3ST, the role of connectedness (belongingness) is emphasized. Connectedness can act as a protective factor, even in individuals experiencing high levels of pain and hopelessness. If an individual has low belongingness, suicidal ideation can escalate into serious suicidal intent (15). The findings of this study confirmed that low belongingness has a direct effect on suicidal behavior and mediates the relationship between pain, hopelessness, and suicidal behavior, validating the second assumption of the 3ST. Van Orden et al. (2010) also emphasized the role of interpersonal factors in suicide, noting that thwarted belongingness and perceived burdensomeness predict suicidal desire (18). Other studies have shown that loneliness predicts future suicidal ideation and behavior (47).
Moreover, consistent with the 3ST, the interaction between pain, hopelessness, and suicidal behavior is mediated by suicidal ideation, confirming the theory's assertion that pain and hopelessness indirectly influence suicidal behavior. This finding aligns with a previous study conducted in Iran (44).
The third stage of the 3ST posits that the transition from suicidal thoughts to suicidal actions occurs when an individual possesses the capability for suicide (15). However, this finding was not supported in the current study, which contrasts with the 3ST and previous studies (15, 38, 39). It is important to note that this sample consisted of healthy students who had not attempted suicide, and it is possible that their capability for suicide had not reached a level where it could predict suicidal behavior.
Overall, this study demonstrated that the first two stages of the 3ST effectively explain suicidal thoughts and behaviors in a healthy student population. However, in contrast to the third stage of the theory, the capability for suicide does not predict suicidal behavior in this population.
Importantly, the study presents a novel perspective by demonstrating the applicability of the Three-Step Theory of Suicide in a non-clinical student population, providing valuable insights into the relationships between the model's key elements.
5. 1. Limitations and Future Directions
This study has several limitations that suggest directions for future research. It adopted a cross-sectional design, and future studies should consider longitudinal approaches for a more precise evaluation. This study examined the theory in a non-clinical population without psychiatric disorders, and it would be beneficial to explore the theory in clinical populations or individuals with a history of suicide attempts. Additionally, this study only examined connectedness from a social perspective, rather than considering broader connections (e.g., purpose, meaning, responsibilities) as proposed by the 3ST. Future research should explore these aspects and use more comprehensive tools to assess connectedness.
5. 2. Implications for Suicide Prevention
This study offers concepts relevant to suicide prevention interventions within the student population. According to the 3ST, reducing the risk of suicide requires interventions—whether medication or psychotherapy—that target one or more key components: Reducing pain, increasing hope, and improving interpersonal relationships. Future studies can explore how addressing these factors may contribute to suicide prevention.