1. Background
Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) is a complex and debilitating condition characterized by a range of symptoms. According to the National Institutes of Health (NIH) guidelines, CP/CPPS is classified as a distinct subgroup of prostatitis, with two categories: IIIA and IIIB. This syndrome is defined by the presence of pain in the perineum, pelvis, suprapubic region, or external genitalia, accompanied by varying degrees of urination and/or ejaculation disorders, without evidence of bacterial infection (1).
Chronic prostatitis/chronic pelvic pain syndrome is a significant and complex health issue, affecting approximately 2 - 10% of men worldwide. This condition significantly impairs patients' quality of life due to the chronic nature of its symptoms. Despite significant progress in basic and clinical research, the underlying causes and mechanisms of CP/CPPS remain poorly understood, underscoring the need for further investigation (2, 3). Some studies have suggested that underlying psychiatric factors may contribute to the development of CP/CPPS, with some research even classifying it as a psychosomatic disorder (4-6).
Despite the availability of symptom definitions, a good classification system, and a standardized measurement instrument [National Institutes of Health (NIH) Chronic Prostatitis Symptom Index (NIH-CPSI)] (7), research on the role of psychosocial factors in CP/CPPS lags behind that of other chronic pain conditions. Due to the diverse and complex nature of symptoms in CP/CPPS, it is essential to gain a more detailed understanding of the psychological and social factors underlying the condition to develop targeted and effective treatment strategies for patients with CP/CPPS (8).
Obsessive-compulsive disorder (OCD) is a psychiatric disorder that affects around 1% to 3% of the population, causing significant impairment and distress (9). This disorder is characterized by obsessions and compulsions that consume considerable time and lead to marked discomfort and functional impairment in patients (10). Some previous studies have suggested a relationship between OCD and chronic urological diseases, such as overactive bladder syndrome and CP/CPPS (4, 11).
Recent investigations into the psychiatric factors associated with CP/CPPS have emerged; however, there remains a critical knowledge gap regarding the underlying causes of this condition and the relationship between psychiatric factors and the development and exacerbation of its symptoms (8, 12, 13).
2. Objectives
The primary objective of the present study is to explore the potential correlation between OCD and CP/CPPS. Specifically, we will examine the co-occurrence of OCD and CP/CPPS, as well as the influence of OCD on symptom severity.
3. Methods
3.1. Study Population
This study recruited patients from the Urology Clinic of Shohada-e-Tajrish Referral Hospital between April 2023 and April 2024. The case group consisted of patients diagnosed with CP/CPPS, while the control group consisted of healthy individuals with no history of urological disease or pelvic pain.
The inclusion criteria were as follows.
3.1.1. Case Group
- Confirmation of CP/CPPS diagnosis by a urologist not affiliated with the research team.
- Presence of prostatitis symptoms for at least 6 months.
- Absence of genitourinary infection, as confirmed by urine analysis (U/A), urinalysis (U/C), and the 2-glass test.
3.1.2. Control Group
- Healthy individuals with no history of urinary irritation symptoms or vague pelvic pain
The exclusion criteria are as follows:
- Previous history of genitourinary infection
- Malignancies
- Recurrent urinary stones
- Inflammatory bowel disease
- Benign prostatic hyperplasia
- Psychotic disorder
- Neurological diseases
Patients were excluded from the study if a relevant specialist confirmed any of the above conditions. Ultimately, 60 participants were recruited, with 30 individuals in the case group and 30 in the control group.
3.2. Study Design
This case-control study aimed to explore the association between OCD and CP/CPPS. The study comprised a case group of 30 individuals with CP/CPPS and a control group of 30 healthy individuals. We investigated the prevalence of OCD in both groups and compared the results. Additionally, we examined the relationship between OCD and symptom severity in patients with CP/CPPS.
3.3. Assessment Tools
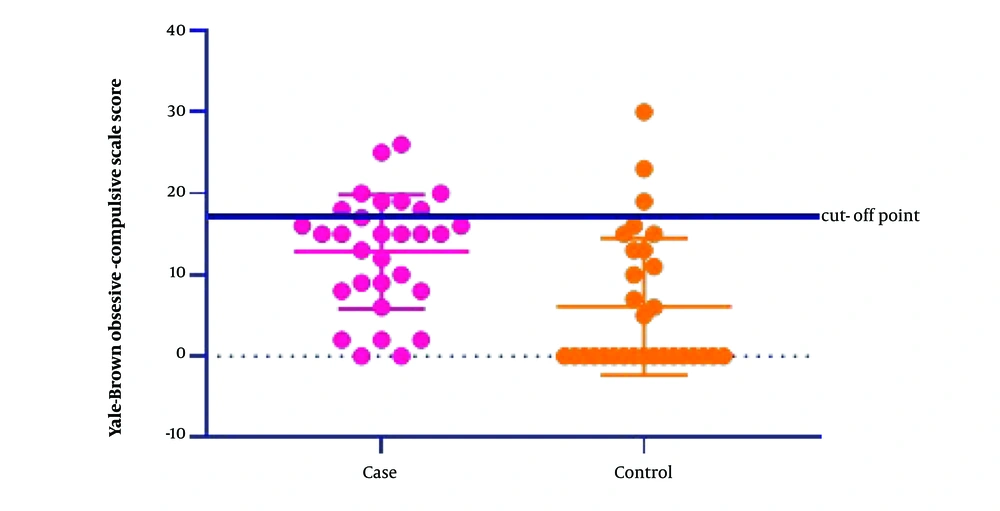
The prevalence of OCD in both groups was assessed by a psychiatrist using the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS) (14). The Y-BOCS scores range from 0 to 40, with a cut-off point of 17 or higher indicating a diagnosis of OCD.
The severity of CP/CPPS symptoms in the case group was evaluated by a urologist using the NIH-CPSI questionnaire (15). This scale assesses three domains: Pain (0 - 21), urinary symptoms (0 - 10), and quality of life (0 - 12), with a total score range of 0 to 43.
Both questionnaires have been validated for use in Iranian populations (16, 17).
3.4. Outcome Assessment
The primary outcome is to investigate the prevalence of OCD in individuals with CP/CPPS compared to healthy individuals. The secondary outcome is to examine the association between OCD and the severity of CP/CPPS symptoms.
3.5. Statistical Methods
Data analysis was conducted using SPSS software version 22. The results are presented as means and standard deviations for quantitative variables, and frequencies and percentages for qualitative variables.
For the analysis of quantitative data, Pearson's correlation test was employed to examine the relationships between variables. To compare the groups in terms of quantitative variables, the normality of the data distribution was assessed using the Shapiro-Wilk test. Then, either the Mann-Whitney U test or the t-test was used to compare the two groups. For comparing qualitative variables, Fisher's exact test or the chi-square test was used. Multivariate linear regression analysis was performed to calculate odds ratios (OR) and identify potential predictors.
In all statistical analyses, a P-value of 0.05 or lower was considered statistically significant.
3.6. Ethical Statement
This study did not incur any costs for participants, and the researchers did not influence the patients' decision-making or treatment processes in any way. Each participant provided informed consent before participating in the study.
This research was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences, with approval number IR.SBMU.MSP.REC.1401.481.
4. Results
The study included 60 participants: Thirty controls and 30 individuals with CP/CPPS. The mean age of the participants was 42.83 ± 14.38 years (range: 18 - 80 years). A comparison of demographic variables between the case and control groups showed no statistically significant differences, as presented in Table 1.
| Variables | Case (N = 30) | Control (N = 30) | P-Value |
|---|---|---|---|
| Age (y) | 43.43 ± 14.36 | 42.25 ± 14.61 | 0.75 |
| BMI (kg/m2) | 24.76 ± 4.26 | 26.56 ± 4.97 | 0.13 |
| Duration of chronic prostatitis (mon) | 37.00 ± 37.29 | - | - |
| Marital status (married) | 21 (70) | 21 (70) | 0.99 |
| Smoking history | 10 (33.3) | 9 (30) | 0.78 |
| Diabetes mellitus | 2 (6.7) | 1 (3.3) | 0.99 |
Demographic and Clinical Characteristics of Case and Control Groups a
In this study, 12 (20%) of the 60 individuals examined met the criteria for OCD based on a Y-BOCS cut-off score of 17. Of these, 9 were from the CP/CPPS group and 3 were from the healthy individuals group. Although there was no statistically significant difference in the prevalence of OCD between the case and control groups (P = 0.10), the average Y-BOCS scores were significantly higher in the CP/CPPS group (12.83 ± 7.02) compared to the control group (6.1 ± 8.4) (P = 0.001), as shown in Figure 1.
To examine the relationship between OCD symptoms and the severity of CP/CPPS symptoms, we analyzed the correlation between Y-BOCS scores and scores from various components of the NIH-CPSI questionnaire, including pain, urinary symptoms, and quality of life. A significant correlation was found between Y-BOCS scores and pain scores, quality of life scores, and total NIH-CPSI scores in patients with CP/CPPS (Table 2). Furthermore, the multivariate regression test results revealed that Y-BOCS scores were an independent predictor of symptom severity, even after controlling for other potential risk factors (Table 3).
| Variables | r Coefficient | P-Value |
|---|---|---|
| Y-BOCS scores/pain scores of NIH-CPSI | 0.4 | 0.02 |
| Y-BOCS scores/urinary symptom scores of NIH-CPSI | -0.27 | 0.15 |
| Y-BOCS scores/quality of life scores of NIH-CPSI | 0.37 | 0.04 |
| Y-BOCS scores/total scores of NIH-CPSI | 0.35 | 0.05 |
Correlation Between Yale-Brown Obsessive-Compulsive Scale Scores and National Institutes of Health Chronic Prostatitis Symptom Index
| Variables | Multivariate Regression | ||
|---|---|---|---|
| SE | P-Value | Odds Ratio | |
| Age | 0.11 | 0.58 | 0.54 |
| BMI | 0.38 | 0.34 | 0.96 |
| Smoking history | 3.38 | 0.98 | 0.02 |
| Diabetes mellitus | 6.71 | 0.66 | 0.44 |
| Y-BOCS scores | 0.24 | 0.04 | 2.11 |
Association Between Study Variables and National Institutes of Health Chronic Prostatitis Symptom Index Scores in Patients with Chronic Prostatitis/Chronic Pelvic Pain Syndrome
5. Discussion
Our findings revealed a statistically significant difference between the patients with CP/CPPS and the healthy individuals in terms of Y-BOCS scores, with the patient group exhibiting higher scores. However, this difference did not translate into a significant difference in the prevalence of OCD itself.
A striking finding of this study was the direct and significant correlation between Y-BOCS scores, pain scores, quality of life scores, and total scores of NIH-CPSI. Specifically, patients with CP/CPPS who had higher Y-BOCS scores experienced more pain and lower quality of life. Furthermore, our analysis revealed that OCD, as evaluated by Y-BOCS scores, was an independent predictor of the severity of CP/CPPS symptoms. These findings suggest that addressing OCD may be an important component of comprehensive treatment plans for individuals with CP/CPPS.
The CP/CPPS is a chronic condition marked by debilitating pelvic pain and discomfort, which can be notoriously challenging to treat (18). Despite its prevalence, the underlying causes of CP/CPPS remain debated among healthcare professionals. Given the significant impact this disease has on patients' quality of life and the substantial costs it incurs for healthcare systems, it is essential to investigate the underlying factors that contribute to this complex condition (3, 19).
The heterogeneity of CP/CPPS underscores the need for a more comprehensive understanding of the psychological mechanisms underlying this condition. Studies indicate that psychological factors have a substantial impact on the development and worsening of CP/CPPS symptoms, a notion that has been supported by studies for decades (8). For instance, Piontek et al. identified behavioral patterns associated with depression in patients with CP/CPPS, particularly during symptom flare-ups (20). Furthermore, Naliboff et al. reported higher levels of lifetime stress in this patient population, along with increased self-reported cognitive deficits compared to individuals in the general population (21). In light of the accumulating evidence regarding the relationship between psychological factors and CP/CPPS symptoms, the application of psychiatric approaches in treating these patients has been increasingly explored and developed (22, 23). A randomized controlled trial by Wang et al. found that psychological interventions significantly improved treatment outcomes for patients with CP/CPPS (22). Despite these advancements, there remains a critical need for deeper insights into the psychological factors contributing to this condition to further enhance the efficacy of treatment strategies.
Obsessive-compulsive disorder is a common psychiatric condition that can manifest with various urological symptoms, including sexual dysfunction or vague urinary-genital infections. Accurate diagnosis of OCD in these cases is crucial to avoid misdiagnosis, which can lead to associated risks to patients, unnecessary physical examinations, and treatment of the wrong disease. Therefore, urologists should consider the possibility of OCD in patients presenting with these symptoms, particularly when the underlying cause is not immediately apparent (24).
A study by Tournikioti et al. evaluated 57 patients with chronic prostatitis, assessing symptoms and OCD using the Leyton Obsessional Inventory (LOI). The results revealed that 58% of patients exhibited abnormal LOI scores, indicating the presence of obsessive-compulsive characteristics, a remarkably high percentage (4).
Some research suggests that cellular and molecular changes related to psychological problems may be primarily responsible for the development of CP/CPPS in some patients (25). For example, studies have shown that individuals with depression tend to have lower levels of interleukin-10 in their peripheral mononuclear cells compared to healthy controls. Additionally, in patients with stage III prostate disease, the level of concern is associated with lower levels of interleukin-6 and 10 in the seminal plasma (26).
A growing body of evidence suggests that urological chronic pain diseases frequently co-occur with psychiatric disorders (27, 28). For instance, Weissman et al.'s study found that patients with interstitial cystitis are at a higher risk of developing panic disorder over their lifetime (29). Similarly, Allameh et al.'s study revealed that Y-BOCS scores were significantly higher in patients with Overactive Bladder Syndrome compared to a control group (11). Our study's results also indicate that, although OCD in patients with prostatitis was not significantly higher than in the control group, these patients had a significantly higher Y-BOCS score than the control group. Furthermore, a significant change in pain intensity and quality of life was observed as this score increased.
The interpretation of these studies' results suggests that an underlying psychiatric issue may be a key contributor to the onset and progression of chronic urological diseases. Moreover, these findings confirm previous studies' results, emphasizing the importance of psychiatric treatments in achieving more effective treatment outcomes for this patient population.
5.1. Limitations of the Study
The main limitation of the present study is its small sample size. As a result, the findings may not be generalizable to all patients with CP/CPPS. Additionally, the limited sample size may have reduced the power to detect statistically significant differences between groups. Future studies with larger, multi-center cohorts covering diverse racial and age groups can help address these limitations and provide more accurate and reliable insights into the relationship between psychiatric treatments and chronic urological diseases. Ultimately, such studies could inform more effective clinical practices and treatment decisions.
5.2. Conclusions
The present study underscores the significance of psychological factors in CP/CPPS, emphasizing the need for a more comprehensive understanding of this complex condition. Our findings suggest that brief screening assessments can facilitate timely diagnosis and referral, which are critical for effective management. Furthermore, we highlight the importance of future research to thoroughly explore psychosocial variables and evaluate the efficacy of psychotherapeutic interventions in patients with CP/CPPS.