1. Background
Pain is one of the most common causes of patient visits to healthcare centers (1). According to the International Association for the Study of Pain, pain is defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage. The pain individuals experience can be acute, chronic, intermittent, or a combination of these types. Chronic or recurrent pain refers to pain that is resistant to treatment and persists beyond the usual three-month recovery period (for research purposes) (2). According to the latest findings, the prevalence of chronic pain among adults in Western societies is 20.5%, meaning that at least one in five individuals experiences chronic pain (3). Additionally, its six-month prevalence among the general adult population in Iran (ages 18 to 65) has been reported to range between 9% and 14% (4). Chronic pain manifests in various forms, one of the most common being chronic musculoskeletal pain, which has a prevalence rate of 33% in the general population (5). Chronic musculoskeletal pain is associated with injuries affecting muscles, tendons, ligaments, joints, cartilage, the spine, peripheral nerves, and blood vessels (6). Research findings indicate that more than 20% of medical visits and over 10% of medication sales are related to chronic pain (7). Additionally, in a study involving 618 patients with chronic pain, it was found that 25% of them had been hospitalized or admitted to emergency care centers (8). These outcomes, along with the high costs and work absenteeism associated with chronic pain, have turned it from an individual-level issue into a significant social problem (9). Furthermore, due to the widespread nature of the musculoskeletal system — which includes bones, joints, muscles, and tendons — chronic pain leads to substantial suffering and psychological stress. Medical treatments for this type of pain are also economically burdensome (10, 11). One of the problems individuals with chronic pain face is psychological distress, which refers to a specific emotional state that arises in response to life difficulties and the pressures resulting from them, manifesting either temporarily or persistently (12). Emotional fluctuations associated with psychological distress often present with symptoms such as anxiety, stress, and depression, which influence both overt and covert behaviors and disrupt an individual’s normal functioning (13, 14). The emotional dimension of pain has a strong correlation with psychological problems and significantly affects the patient’s recovery process (15).
Furthermore, pain self-efficacy is another relevant factor in this context. Pain self-efficacy refers to an individual’s confidence in their ability to maintain functioning despite the presence of pain, and its role in alleviating pain-related perceptual disabilities has been well established (16). Pain self-efficacy can effectively enhance functioning and coping in patients with chronic pain and plays a crucial role in self-care. Thus, self-efficacy is an important factor in managing many chronic conditions, and increasing self-efficacy has been linked to reductions in pain, emotional distress, and disability (17, 18). Due to the widespread prevalence of chronic pain and its detrimental effects on patients’ lives, this condition has consistently attracted the attention of clinical specialists, prompting them to explore various therapeutic approaches. Pharmacological treatments, particularly analgesics, primarily aim to reduce or eliminate pain; however, numerous reports indicate unsatisfactory outcomes with existing drug therapies. Consequently, researchers have sought alternative therapeutic options with better safety profiles and comparable efficacy to mitigate the adverse effects associated with pharmacological treatments (19, 20). In this regard, Acceptance and Commitment Therapy (ACT), a third-wave psychological intervention, aims to promote comprehensive awareness and educate patients in managing controllable aspects while accepting and being open to the uncontrollable aspects of their condition. This means that instead of attempting to suppress or control pain-related thoughts, patients are encouraged to allow these thoughts to exist in their minds (21, 22). When these experiences (thoughts and emotions) are engaged with openness and acceptance, even the most distressing ones become more tolerable and less threatening. The ACT is structured around six core processes, including acceptance, cognitive defusion, self-as-context, present-moment awareness, values, and committed action, all of which collectively aim to enhance psychological flexibility (23). Research findings indicate that ACT is effective in various domains, including anxiety, depression, and stress (24-27), as well as pain self-efficacy (27-29).
Given the issues discussed above, and considering that numerous studies have been conducted on the treatment of chronic pain, including psychological therapies, it is noted that such treatments have rarely been applied to individuals with chronic musculoskeletal pain.
2. Objectives
The present study aimed to examine the effectiveness of group-based ACT on pain self-efficacy and psychological distress among individuals with chronic musculoskeletal pain.
3. Methods
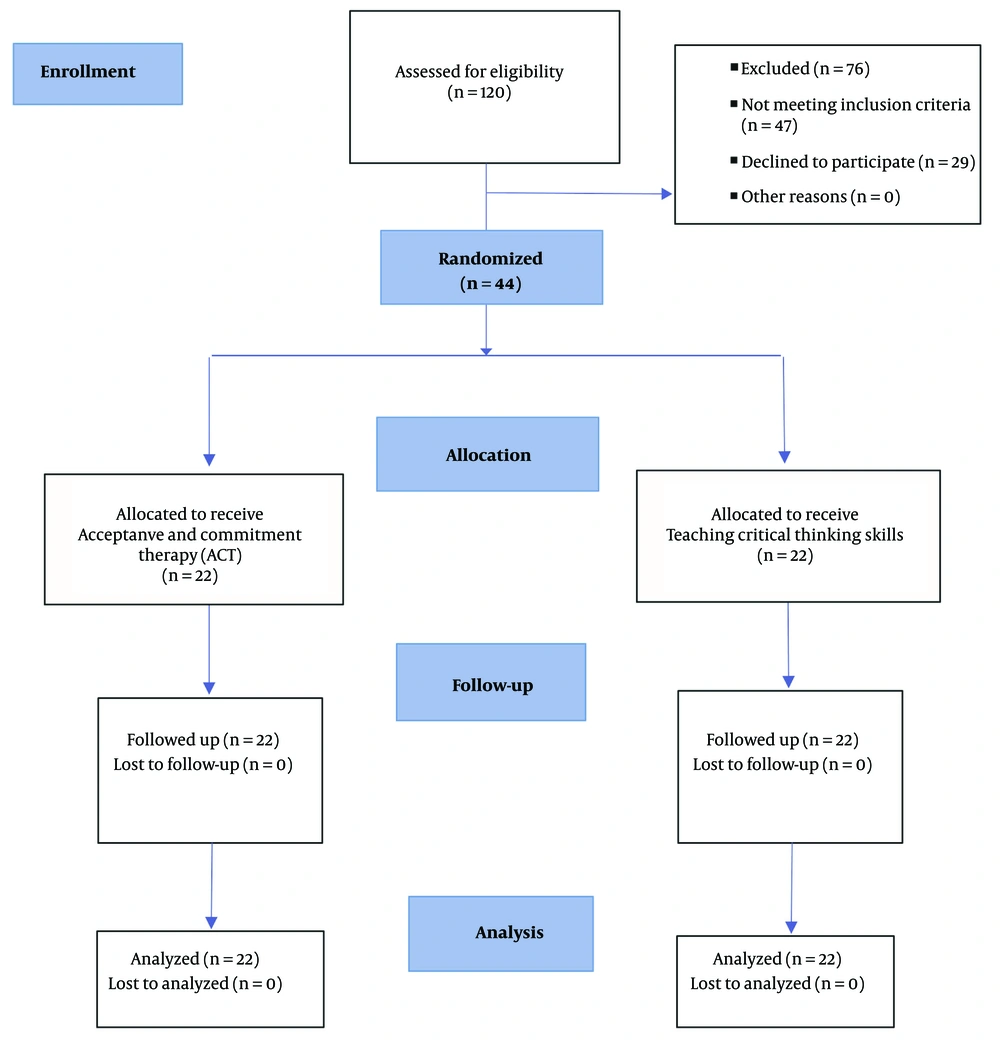
The present research utilized an experimental design with three assessment points: Baseline, post-treatment, and two-month follow-up. The study population consisted of all individuals with chronic musculoskeletal pain who visited Shahid Beheshti Hospital in Kashan during the autumn and winter of 2023. Ethics approval was secured from the research ethics committee of Kashan University of Medical Sciences (IR.KAUMS.MEDNT.REC.1402.105) prior to commencing the study, which is also registered with the Iranian Registry of Clinical Trials under the code IRCT20230806059054N1. Following the acquisition of informed consent, an initial assessment was performed. To determine the sample size, the G*Power 3.1 software was used. Based on the analysis of variance with repeated measures, an effect size of 0.82, a Type I error rate of 0.05, and a power of 0.80 were calculated. For two groups with three measurements, 40 participants were deemed adequate for the study (20 for the experimental group and 20 for the control group). Participants (n = 44) were randomly assigned to either the ACT group or the control group using a 1:1 allocation ratio. The random assignment of eligible participants to the ACT and control groups was facilitated using a secure web-based randomization tool to minimize allocation bias. Given the possibility of attrition, 44 individuals were selected; however, due to the lack of male cooperation, all participants were female (22 for the experimental group and 22 for the control group) and underwent group-based ACT treatment in 8 weekly 90-minute sessions, while the control group received critical thinking skills training in 8 weekly 90-minute sessions. Due to the nature of the psychological intervention, it was not possible to blind participants or therapists to group allocation. However, to minimize potential bias, the outcome assessor who administered and scored the questionnaires was blinded to participants’ group assignments throughout the study.
Inclusion criteria for the study included having a diagnosis of chronic pain by a specialist in physical medicine and rehabilitation, being between the ages of 35 and 65, having at least a basic literacy level, no immediate need for treatment for psychological disorders such as substance use or alcohol abuse, psychotic disorders, or any other condition requiring urgent treatment, no psychological interventions received within the last year, and no medication related to the disorder at least one month before the sessions and throughout the follow-up phase. Exclusion criteria included missing more than two treatment sessions, developing medical conditions that could influence the intervention, and incomplete questionnaire responses (Figure 1).
The data collected were analyzed using multivariate analysis of variance (MANOVA) with repeated measures (baseline, post-treatment, and two-month follow-up). The analysis was performed using SPSS version 23. To assess the effects of time, group, and their interaction on multiple correlated outcomes, a RM MANOVA was conducted. All dependent variables — psychological distress and pain self-efficacy — were simultaneously entered into the model to account for their intercorrelations and to control for Type I error inflation due to multiple testing.
3.1. Tools
3.1.1. Nicholas Pain Self-efficacy Questionnaire (1989)
This 10-item questionnaire, developed by Nicholas in 1989, is based on Bandura’s theory of self-efficacy and aims to assess the patient’s belief in their ability to carry out various activities despite experiencing pain (30). The primary objective is to measure an individual’s sense of efficacy and satisfaction in living with pain. The items on this questionnaire are rated using a 7-point Likert scale (0 = not confident at all to 6 = very confident). The total score ranges from 0 to 60, with a higher score indicating a strong belief in one’s ability to perform daily activities despite the presence of pain, and a lower score suggesting lower self-efficacy. Nicholas (1989) reported the validity of this questionnaire as adequate. Furthermore, the concurrent validity of this questionnaire was verified in the research by Asghari and Nicholas through calculating the correlation between self-efficacy and psychological and general health, which yielded a value of 0.42. The reliability coefficients of the test were reported by Cronbach’s alpha; the reliability of the Nicholas Pain Self-Efficacy Questionnaire (PSEQ) was found to be 0.81 (31). In a study by Sahebi et al., test-retest reliability coefficients were reported to be 0.88 over a 9-day interval (32, 33).
3.1.2. Psychological Distress Questionnaire
The Depression, Anxiety, and Stress Scale (DASS)-21 was introduced by Lovibond and Lovibond as an instrument for assessing these psychological constructs (34). Due to the limitations of the original DASS-42, Antony et al. developed the DASS-21, which retained the three subscales of the previous version and consisted of 21 items (35): Eight items for depression, 7 items for anxiety, and 6 items for stress. Participants are asked to rate their emotional state over the past week based on the statements provided in the questionnaire. The response scale is categorized into four levels: (Not at all), (Mildly), (Moderately), and (Severely). The scoring of this scale, which is based on self-reporting, ranges from 0 (“Not at all”) to 3 (“Very much”). Studies conducted both internationally and in Iran have reported favorable psychometric properties for this scale (33, 36). The psychometric properties of the DASS-21 were examined, and internal consistency reliability (Cronbach’s alpha) was reported as 0.77 for depression, 0.79 for anxiety, and 0.78 for stress. For construct validity assessment, the Beck Depression Inventory (BDI), Zung Anxiety Scale, and Perceived Stress Scale were used. The correlation coefficients were 0.70 between the DASS depression subscale and BDI, 0.67 between the DASS anxiety subscale and Zung Anxiety Scale, and 0.49 between the DASS stress subscale and the Perceived Stress Scale (34). In the present study, the DASS-21 was used to assess psychological distress.
3.1.3. Acceptance and Commitment Therapy Protocol
It is one of the third-wave psychological interventions, aiming to promote comprehensive awareness and educate patients in managing controllable aspects while accepting and being open to the uncontrollable aspects of their condition. The experimental group underwent ACT according to the protocol outlined in Table 1, in eight weekly group sessions, each lasting 90 minutes (37).
| Week | Techniques and Skills |
|---|---|
| Session 1 | Introduction to the fundamental concepts of therapy; familiarizing participants with the research topic; exploring chronic pain experiences among group members and their coping strategies; discussing experiential avoidance and the concept of creative hopelessness; explaining the importance of homework assignments. |
| Session 2 | Retrieving reconnection of values (identifying what truly matters to them); exploring actions they would like to take in the remainder of their lives to uncover their values; evaluating how much pain control aligns with their values; discussing alternative ways to live with pain and discomfort; introductory mindfulness exercise (raisin-eating practice); assigning homework (mindful eating despite pain). |
| Session 3 | Reviewing homework; increasing awareness of inner experiences; recognizing that a thought about pain is merely a thought; distinguishing between having a thought and being defined by its content; distancing from the conceptualized self; living with chronic pain and discomfort; practicing body scan exercise; assigning homework (paying attention to body sensations while falling asleep despite pain). |
| Session 4 | Reviewing homework; mindfulness and practicing mindful breathing; cultivating present moment awareness through exercises; observing thoughts and emotions about chronic pain without judgment; identifying barriers to values-based living; assigning homework (focusing on breathing while falling asleep). |
| Session 5 | Reviewing the previous session, homework assignments, and experiences related to mindful breathing; identifying life goals aligned with values that are hindered by chronic pain; taking gradual steps toward goals; practicing mindful movement; assigning homework (lying down mindfully and observing the rise and fall of the abdomen while breathing during sleep). |
| Session 6 | Reviewing homework; reflecting on actions taken toward values and goals; planning for goal achievement with committed action; assigning homework. |
| Session 7 | Practicing mindful awareness in daily life and routine activities (informal mindfulness exercises); having a beginner’s mind; recognizing language barriers through the “Milk, Milk, Milk” metaphor; assigning homework. |
| Session 8 | Reviewing previous sessions; emphasizing the importance of consistent practice; reinforcing the value of merely observing thoughts; highlighting the significance of commitment to values despite pain and achieving life goals. |
Acceptance and Commitment Therapy Protocol (35)
4. Results
In this study, 44 women participated, who were divided into two groups: Twenty-two participants in the experimental group (ACT group) and 22 in the control group. The average age of the experimental group was 45.36 years, and the control group was 45.59 years. All participants were married. In the experimental group, 13 participants had an education level ranging from primary school to middle school, 5 had education from middle school to high school, 3 had a bachelor’s degree, and 1 had a master’s degree. In the control group, 14 participants had education from primary school to middle school, 6 had education from middle school to high school, and 2 had a bachelor’s degree. The results of the t-test also showed that there was no significant difference between the experimental and control groups in demographic characteristics (Table 2).
| Group/Component | Values | t-Test Results | |
|---|---|---|---|
| t | P-Value | ||
| Experimental group | -0.13 | 0.89 | |
| Elementary school | 13 (59.10) | ||
| Diploma | 5 (22.70) | ||
| Bachelor's degree | 3 (13.60) | ||
| Master's degree | 1 (4.50) | ||
| Control group | -0.13 | 0.89 | |
| Elementary school | 14 (63.60) | ||
| Diploma | 6 (27.30) | ||
| Master's degree | 2 (9.10) | ||
| Experimental group | 0.15 | 0.45 | |
| Average age | 45.36 ± 5.41 | ||
| Control group | 0.15 | 0.45 | |
| Average age | 45.59 ± 5.66 | ||
Descriptive Characteristics of Participants a
Descriptive statistics for each of the study variables, categorized by group and phase, are presented in Table 3.
| Variables | Baseline | Post-treatment | Follow-up | Difference of Means |
|---|---|---|---|---|
| Anxiety | Baseline: 0.09 ± 0.52; post- treatment: -3.95 ± 0.48; follow-up: -3.27 ± 0.45 | |||
| Experimental | 13.45 ± 1.47 | 7.72 ± 1.16 | 8.81 ± 1.05 | |
| Control | 12.54 ± 1.99 | 11.68 ± 1.96 | 12.09 ± 1.84 | |
| Depression | Baseline: 0.63 ± 0.53; post- treatment: -6.36 ± 0.60; follow-up: -6.18 ± 0.74 | |||
| Experimental | 13.90 ± 1.79 | 7.31 ± 1.55 | 8.59 ± 1.43 | |
| Control | 14.54 ± 1.73 | 13.68 ± 2.35 | 14.77 ± 3.20 | |
| Stress | Baseline: -0.04 ± 1.12; post- treatment: -5.31 ± 0.82; follow-up: -4.59 ± 0.91 | |||
| Experimental | 13.13 ± 3.61 | 7.70 ± 1.73 | 8.50 ± 1.99 | |
| Control | 13.18 ± 3.85 | 12.72 ± 3.46 | 13.09 ± 3.80 | |
| Pain | ||||
| Experimental | 24.77 ± 4.23 | 39.45 ± 3.68 | 37.54 ± 2.98 | Baseline: 0.77 ± 1.44; post- treatment: 14.68 ± 1.42; follow-up: 13.37 ± 1.30 |
| Self-efficacy | ||||
| Control | 24.00 ± 5.28 | 24.77 ± 5.58 | 23.81 ± 5.33 | Baseline: 0.77 ± 1.44; post- treatment: 14.68 ± 1.42; follow-up: 13.37 ± 1.30 |
Descriptive Statistics for the Studied Variables, Categorized by Group and Phases a
In Table 3 above, the mean and standard deviation for each of the variables under investigation and their components are reported. To analyze the results, repeated measures analysis of variance (MANOVA) was applied. Prior to conducting this analysis, the assumptions were examined.
The non-significant results of Box’s M test for the study variables in Table 4 confirmed homogeneity of variance-covariance, except for the depression and stress variables (P < 0.05). Additionally, none of the variables were significant in Levene’s test (P > 0.05), confirming that homogeneity of variances was met. The assessment of homogeneity of regression is another assumption of repeated measures ANOVA. Since none of the scales showed significant results for homogeneity of regression (P < 0.05), it can be concluded that the assumption of homogeneity of regression was satisfied. Bartlett’s test of sphericity showed a significant correlation between the dependent variables (Approx. Chi-square = 581.95, P < 0.0001).
| Variables | Box’s M | F | df 1 | P-Value |
|---|---|---|---|---|
| Anxiety | 11.99 | 1.84 | 6 | 0.08 |
| Depression | 17.41 | 2.67 | 6 | 0.01 |
| Stress | 80.54 | 12.37 | 6 | 0.0001 |
| Pain self-efficacy | 12.08 | 1.85 | 6 | 0.08 |
| Variables | Levene | DFB | DFW | P-Value |
| Anxiety | 1.33 | 1 | 42 | 0.25 |
| Depression | 0.01 | 1 | 42 | 0.91 |
| Stress | 11.46 | 1 | 42 | 0.67 |
| Pain Self-efficacy | 0.82 | 1 | 42 | 0.37 |
Results of Levene’s Test for Homogeneity of Variances for the Dependent Variables at the Baseline Stage
Additionally, the results of the Kolmogorov-Smirnov test indicated that the scores for the variables under investigation were normally distributed (P < 0.05). Overall, based on the conducted checks, the fundamental assumptions of the parametric statistical method for repeated measures ANCOVA were met. The results of this test are presented in Table 5.
| Variables | P | F | DF | P-Value | η2 | Post-hoc |
|---|---|---|---|---|---|---|
| Time × group | ||||||
| Pillai’s trace | 0.97 | 126.234 | 32 | 0.0001 | 0.977 | 1.000 |
| Wilks’ lambda | 0.02 | 126.234 | 32 | 0.0001 | 0.977 | 1.000 |
Multivariate Analysis of Covariance for Pain Self-efficacy and Psychological Distress Variables
The results showed that the effect of the ACT intervention was significant, and there was at least one dependent variable with a significant difference between groups. Furthermore, 97% of the difference between the experimental and control groups over time was explained by this effect. Additionally, the interaction between the ACT intervention and group membership over time and group was also significant for the pain self-efficacy variable (P < 0.05). The results of the repeated measures ANCOVA for the pain self-efficacy variable are presented.
As presented in Table 6, the effect of time on the scores of anxiety (F(1, 41) = 173.84, P < .0001), depression (F(1, 41) = 119.22, P < .0001), stress (F(1, 41) = 188.93, P < .0001), and pain self-efficacy (F(1, 41) = 478.53, P < .0001) was statistically significant. These results indicate meaningful changes in all four variables over time, interpreted at the 95% confidence level. Therefore, it can be stated that regardless of the experimental group, there were significant differences in the mean scores for anxiety, depression, stress, and pain self-efficacy at baseline, post-treatment, and follow-up (P < 0.05). To compare and examine the differences in mean scores for pain self-efficacy and psychological distress components at baseline, post-treatment, and two-month follow-up, Bonferroni post-hoc tests were used, and the results are presented in Table 7.
| Components | Sum of Square | DF | Mean Square | F | P-Value | η2 | Power |
|---|---|---|---|---|---|---|---|
| Anxiety | |||||||
| Within subject | |||||||
| Time | 1.13 | 1 | 1.13 | 2.55 | 0.11 | 0.05 | 0.34 |
| Time × group | 2.89 | 1 | 2.89 | 6.53 | 0.01 | 0.13 | 0.70 |
| Error | 18.19 | 41 | 0.44 | ||||
| Between subject | 173.84 | 0.0001 | 0.80 | 1.00 | |||
| Time | 359.46 | 1 | 359.46 | ||||
| Error | 84.77 | 41 | 2.06 | ||||
| Depression | |||||||
| Within subject | |||||||
| Time | 0.15 | 1 | 0.15 | 0.05 | 0.81 | 0.001 | 0.05 |
| Time × group | 0.22 | 1 | 0.22 | 0.08 | 0.77 | 0.002 | 0.05 |
| Error | 109.01 | 41 | 2.65 | ||||
| Between subject | 119.22 | 0.0001 | 0.74 | 1.00 | |||
| Time | 760.54 | 1 | 760.54 | ||||
| Error | 261.53 | 41 | |||||
| Stress | |||||||
| Within subject | |||||||
| Time | 0.61 | 1 | 0.61 | 2.44 | 0.12 | 0.05 | 0.33 |
| Time × group | 2.94 | 1 | 2.94 | 11.66 | 0.001 | 0.22 | 0.91 |
| Error | 10.35 | 41 | 0.25 | ||||
| Between subject | 188.93 | 0.0001 | 0.82 | 1.00 | |||
| Time | 533.11 | 1 | 533.11 | ||||
| Error | 115.69 | 41 | 2.82 | ||||
| Pain; self-efficacy | |||||||
| Within subject | |||||||
| Time | 0.72 | 1 | 0.72 | 0.65 | 0.42 | 0.01 | 0.12 |
| Time × group | 4.21 | 1 | 4.21 | 3.78 | 0.059 | 0.08 | 0.47 |
| Error | 45.74 | 41 | 1.11 | ||||
| Between subject | 478.53 | 0.0001 | 0.92 | 1.00 | |||
| Time | 4017.93 | 1 | 4017.93 | ||||
| Error | 344.24 | 41 | 8.39 |
Repeated Measures Analysis of Variance for Pain Self-efficacy and Psychological Distress Variables
| Components | MD | SE | P-Value |
|---|---|---|---|
| Anxiety | |||
| Baseline | |||
| Post-treatment | -7.727 | 0.331 | 0.0001 |
| Follow-up | -6.295 | 0.364 | 0.0001 |
| Post-treatment | |||
| Follow-up | 1.432 | 0.234 | 0.0001 |
| Depression | |||
| Baseline | |||
| Post-treatment | 3.295 | 0.190 | 0.0001 |
| Follow-up | 2.545 | 0.198 | 0.0001 |
| Post-treatment | |||
| Follow-up | -0.750 | 0.142 | 0.0001 |
| Stress | |||
| Baseline | |||
| Post-treatment | 3.727 | 0.314 | 0.0001 |
| Follow-up | 2.545 | 0.378 | 0.0001 |
| Post-treatment | |||
| Follow-Up | -1.182 | 0.344 | 0.0001 |
| Pain; self-efficacy | |||
| Baseline | |||
| Post-treatment | 3.091 | 0.277 | 0.0001 |
| Follow-up | 2.364 | 0.224 | 0.0001 |
| Post-treatment | |||
| Follow-up | -0.727 | 0.121 | 0.0001 |
Bonferroni Post-hoc Test for Pairwise Comparisons of Scales Across Time
As shown in Table 7, significant differences were found between the baseline, post-treatment, and two-month follow-up scores, as well as between post-treatment and follow-up for the components of pain self-efficacy and psychological distress (anxiety, depression, and stress). Based on the mean scores (Table 2), participants had higher pain self-efficacy and lower psychological distress (anxiety, depression, and stress) after the treatment. These results indicate that the ACT intervention had a significant and favorable effect on these variables among the participants.
5. Discussion
The present study aimed to examine the effectiveness of ACT in pain self-efficacy and psychological distress in individuals with chronic musculoskeletal pain. One of the key findings was that there was a significant difference between the two groups across the three phases (baseline, post-treatment, and two-month follow-up) in pain self-efficacy. This finding is consistent with the research of Wang et al., Khashooi et al., and Zarei et al. (27-29). To explain this result, pain self-efficacy refers to an individual’s confidence in their ability to maintain functioning despite having pain, and its role in improving pain-related cognitive impairments has been confirmed (38). The ACT facilitates this process by promoting open awareness and teaching patients to control the controllable aspects of their condition while accepting and opening up to the uncontrollable aspects. In this approach, rather than trying to suppress thoughts related to the illness, individuals are encouraged to allow these thoughts to exist without attempting to eliminate them (21). The therapist’s goal is not to reduce symptoms directly; rather, it aims to help individuals deal with their symptoms. This approach alters the way individuals relate to distressing thoughts and emotions, allowing them to perceive these experiences not as pathological symptoms but as harmless phenomena (even if they are unpleasant or distressing) (39). Through these techniques, ACT can enhance pain self-efficacy in individuals with chronic musculoskeletal pain, helping them manage their condition more effectively. Value-based action, combined with the willingness to act despite discomfort, is a core component of ACT, enabling individuals to pursue personally meaningful goals rather than solely focusing on eliminating unwanted experiences. These value-based actions contribute to a more meaningful, fulfilling, and successful life and, in turn, increase pain self-efficacy, thereby helping patients manage their condition more effectively (40).
Another finding of this study was a significant difference between the two groups (baseline, post-treatment, and follow-up) in the components of anxiety, depression, and stress. This result is consistent with the findings of Jiang et al. (26), Gloster et al. (25), Fadhil et al. (24), Zamani- Zamani et al. (41), and Rahnama et al. (36). This result can be explained by the concept of psychological distress, which refers to an emotional state in which individuals react to life challenges and stressors, either temporarily or persistently (12). In compassion-focused ACT, emphasis is placed on relaxation, mindfulness, self-compassion, and cognitive defusion, all of which play a crucial role in reducing mental distress and worry. The goal of ACT is not to eliminate symptoms but to enhance psychological flexibility, which in turn improves cognitive flexibility. The ACT promotes a non-judgmental approach to present-moment experiences by encouraging individuals to observe and describe their experiences rather than suppress or avoid them. This leads to the development of active coping strategies that help maintain psychological well-being. Therefore, ACT can be considered an effective approach in reducing stress and psychological distress by utilizing its specific mechanisms. This therapy can help reduce distress in patients and alleviate disorder-related symptoms. One of the key components of ACT is cognitive fusion, where individuals become entangled with their thoughts, bodily sensations, and emotions, failing to distinguish them from reality. In chronic pain, fused thoughts like “I can’t live with this pain” dominate perception, intensifying anxiety, depression, and avoidance. The ACT addresses this by encouraging defusion — changing how individuals relate to their thoughts rather than altering the thoughts themselves — thereby enhancing psychological flexibility and reducing distress. Through this process, individuals can better regulate and manage factors that negatively impact mental health (40).
5.1. Conclusions
The current findings suggest that ACT may be particularly useful for individuals with low psychological resilience or heightened emotional distress due to chronic illness. Therefore, integrating psychological interventions such as ACT alongside standard medical treatments may improve outcomes, particularly when patients exhibit elevated levels of anxiety, depression, or stress. Promoting psychological education focused on illness-related emotions and encouraging collaboration among psychologists, counselors, and medical professionals can contribute to more holistic care and improved quality of life for individuals coping with chronic physical conditions. Such collaboration can occur in integrated care teams where psychologists manage distress, counselors assist with coping strategies, and physicians monitor physical symptoms — ensuring consistent communication through joint treatment plans.
5.2. Limitations
A key limitation of this study is its restricted sample, which affects the generalizability of the findings. The participants were all women aged 35 to 65, residing in Kashan, and diagnosed with chronic musculoskeletal pain. Due to a lack of male referrals and participation, the sample lacked gender diversity, which limits the extent to which the results can be applied to broader or more heterogeneous populations. Moreover, the findings may not be generalizable to individuals with different cultural backgrounds, age ranges, or chronic conditions beyond musculoskeletal pain. To enhance external validity, future studies should be conducted with more diverse and representative samples, including both genders, various age groups, and patients from different geographic or sociocultural contexts. Research should also explore the applicability of ACT to other chronic illnesses to determine whether the observed benefits extend beyond this specific condition. Additionally, it would be valuable to compare ACT with other evidence-based psychological interventions — such as Cognitive Behavioral Therapy (CBT) and Compassion-Focused Therapy (CFT) — to examine relative effectiveness.