1. Context
Attention-deficit/hyperactivity disorder (ADHD) is a psychobiological disorder that is described by attention deficit, hyperactivity, and reduced impulse control. Based on the diagnostic and statistical manual of mental disorders, Fifth edition (DSM-V), ADHD is a “persistent pattern of inattention and/or hyperactivity and impulsivity that interferes with functioning or development. The inattention manifests behaviorally in ADHD as wandering off task, lacking persistence, having difficulty sustaining focus and being disorganized, and is not due to defiance or lack of comprehension. Hyperactivity refers to excessive motor activity (such as a child running about) when it is not appropriate, or excessive fidgeting, tapping, or talkativeness (1).” Based on DSM-V results, several symptoms appear before the age of 7. The 3 subtypes that are related to ADHD include predominantly hyperactive, predominantly inattentive, and a combination of one or more of the aforementioned types.
A child must demonstrate at least 6 of the 9 symptoms and adolescents must demonstrate at least 5 of the 9 symptoms in a cluster form before the 3 subtypes (1). Past research illustrated that symptoms related to hyperactivity may decrease as the child grows older, while the child’s inattentiveness remains relatively unchanged (2, 3). Barkley defined the main characteristic of ADHD as difficulty in behavioral inhibition (4).
Unintentional behavior possessed by the child diagnosed with ADHD appeared to affect their academic achievement throughout their academic career. In addition, these children displayed problems with their social skills and difficulty communicating, due to the apparent frustrations with their academic performance (5). The DSM-V shows that the rate of ADHD was greater in males than in females, with a ratio of nearly 2:1 in children and 1.6:1 in adults (1).
There are dissimilar theories on the subject of the causes of attention deficit. Attention deficit includes the combination of biologically determined reactivity of the nervous system and failure to self-regulate, and environmental disturbances (6, 7). Students who cannot centralize their thoughts are impatient and evoke negative responses from their environment, which can provoke a perception of social refusal. The continued experience of refusal at school mixed with the vulnerability of the child/adolescent nervous system is thought to produce negative perceptions, evoking compensatory behaviors, such as, aggressive comic behavior, feeling alone, and/or a depressive status. To decrease such symptoms, the creation and protection of a supportive and caring home situation would appear to be an important factor. Students must have a feeling of being accepted, the ability to develop trusting relationships, and also a belief that there are methods that can help them. This situation can be quite difficult to achieve if the parents displays symptoms similar to their child. ADHD indicatorsare not just limited to childhood, and the relative dynamics of this disorder may cause the condition to persevere.
Based on previous studies, the principal treatments of ADHD have focused on the use of medication, behavioral, cognitive, cognitive-behavioral, and neural treatments (8-16). A review of the literature between 2000 and 2013 identified the multimodal treatment of ADHD for the ADHD child and/or adolescent. These combination treatments include self-control, self-regulation, cognitive, cognitive-behavioral, cognitive play, behavioral play, motor-perceptual rehearsal, functions management training, verbal self-education training, education of children by parents, positive therapy, training of parents, parental constructive program, and training of stress coping skills. These studies demonstrated that the mentioned treatments were more successful and had longer lasting effects on attention deficit, social skills, and behavioral problems in ADHD than the singular medication treatment or behavioral therapy (17-28).
2. Evidence Acquisition
In this meta-analysis study, the researcher used published journal articles and theses on the topic of the effectiveness of intervention/treatment programs on ADHD from the scientific information database (SID), the Iranian research institute for information science and technology (IRANDOC), the national library and the archives of the Islamic Republic of Iran (NLAI), and the United States national library of medicine (NLM) and national institutes of health (PubMed) websites during 2000 - 2013. Database search was performed with the following keywords: treatment program and ADHD, intervention program and ADHD, and instruction. In the preliminary database search, 72 related articles were obtained from SID, 64 dissertations and abstracts from the IRANDOC website, 23 dissertations and articles from the NLAI website, and 175 dissertations and articles from the PubMed website. All findings were screened for inclusion, based on the title and abstract, using the following restrictions regarding the treatment/intervention program on ADHD. This study’s concern was interventions/treatments intended to improve ADHD. After reviewing the preliminary articles and theses on ADHD, a total number of 17 articles were screened for possible inclusion (Table 1).
| Topic | Author | Type of Research | Treatment/Session |
|---|---|---|---|
| Effectiveness of self-control treatment on social skills in ADHD students | Beh Pajooh et al. (18) | Quasi-experimental | Self-control/4 sessions |
| Effectiveness of self-regulation of attentive behavior, self-regulation of motivational behavior, and verbal self-instruction on symptoms of attention deficit/hyperactivity | Moradi et al. (29) | Quasi-experimental | Self-regulation of attention behavior, self-regulation of motivational behavior, and verbal self-instruction/10 |
| Effectiveness of cognitive behavioral therapy on self-perception in ADHD students | Salehi et al. (21) | Experimental | Cognitive behavioral/19 |
| Effectiveness of early play treatment on ADHD students’ attentive-inattentive behaviors | Shoshtari et al. (30) | Experimental | Play treatment/12 |
| The effectiveness of using perceptual-motor practices on behavioral disorder among five to eight year old children with ADHD | Dehghan et al. (24) | Quasi-experimental | Perceptual-motor practices/18 |
| The efficacy of short-term executive functions training on the reduction of symptoms of attention deficit and hyperactivity of elementary boy students in Isfahan metropolitan area | Saheban et al. (26) | Experimental | Short-term executive functions training/9 |
| The efficacy of neurofeedback, compared to retalian, and combined neurofeedback and ritalin for the reduction of ADHD symptoms | Yaghubi et al. (17) | Quasi-experimental | Neurofeedback, retalin, & drug combination/10 |
| Which symptoms of ADHD would improve with play therapy and yoga? | Saadat (31) | Quasi-experimental | Play therapy and yoga |
| The effect of narrative therapy on increase of attention and decrease of hyperactivity in children with attention deficit hyperactivity disorder | Shafieian (32) | Quasi-experimental | Narrative therapy/11 |
| The effects of training neurofeedback on decreasing the intensity of ADHD symptoms in primary students | Hagighi (33) | Experimental | Neurofeedback therapy/40 |
| Effectiveness of cognitive-behavioral therapy in reducing symptoms in children with ADHD | Rahmanzadeh (34) | Experimental | Cognitive-behavioral therapy/12 |
| The effect of aerobic exercises on the visual and auditory attention of pre-school boys with ADHD in Isfahan in 2009-2010 | Abedi et al. (35) | Quasi-experimental | Aerobic exercise training therapy/12 |
| Impact of training self-regulation of attentional and motivational behaviors, and verbal self-instruction on ADHD symptoms amelioration | Hashemi Nosrat Abad et al. (36) | Quasi-experimental | Self-care behaviors, self-stimulation behaviors, verbal self-instruction |
| Few effects of far transfer of working memory training in ADHD: a randomized controlled trial | Egeland et al. (37) | Experimental | Working memory training/25 |
| Effectiveness of a school-based multicomponent program for the treatment of children with ADHD | Miranda et al. (38) | Experimental | Multicomponent program/6 |
| Comparing therapeutic effects of reboxetine with placebo in adult patients with ADHD: A randomized placebo-controlled clinical trial | Riahi et al. (39) | Clinical trial | Reboxetine & placebo/6 |
| Comparative effectiveness of three treatments In reducing hyperactivity disorder in third and fourth levels of male primary school children in Shiraz, Iran | Hadianfard et al. (28) | Experimental | Verbal self-education and mother verbal self-education/8 |
a Abbreviation: ADHD, attention deficit hyperactivity disorder.
These articles had to meet each of the subsequent criteria: the article must have been an original investigated report (experimental, quasi-experimental research), included treatment of at least one independent variable, and the students must have been diagnosed with ADHD. Articles excluded if they did not meet the above criteria, and if the students’ Intelligence quotient scale (IQs) were below 90, or if data for the ADHD students could not be separated from data of the group without ADHD. A total of 17 articles were screened for inclusion in this meta-analysis.
In the present study, the researcher employed coding procedure (40). A coding structure and operational definitions were made to record quantitative information from each of the 17 studies. The following areas were employed for coding purposes. In this study, the research design was classified as experimental and quasi-experimental. The specific kind of design was recorded (e.g.pretest or posttest).
Treatment type was divided into 9 categories:
1. Preparation training treatments were categorized as either content area preparation or self-regulation preparation. 2. Direct training treatments included teacher-led, explicit, and systematic training. 3. Behavioral treatments included treatments in which the employment of positive reinforcement was dependent on the successful completion of an assignment. 4. Practical treatments contained treatments in which the child was candidate for reiterative performance of an ability that was intended to be already within the student’s repertoire, for example: the student would stay for an extra 20 minutes to read the task. 5. Textbook modification included any treatment that modified an original textbook to decrease its stage of difficulty. 6. Combination treatments included the combination of two or more of the treatments. 7. Play treatment (such as aerobic activity and yoga). 8. Pharmaceutical treatments used were Ritalin, methylphenidate, and dextroamphetamine. 9. The final category included any intervention that did not fit in the above-mentioned categories such as cognitive treatment, cognitive-behavioral treatment, and short-term executive function training.
3. Results
In this study, the researcher employed 17 ADHD studies. The data collection of each study is illustrated in Tables 1 and 2. Moreover, the mean and standard deviations of pretests for the 17 ADHD studies are illustrated in Table 3. Furthermore, mean and standard deviations of posttests for the 17 ADHD studies are provided in Table 4.
| Author | Dependent Variable | Instrument | Sample/Type of Sample | Age | The Atudy Area |
|---|---|---|---|---|---|
| Beh Pajooh et al. (18) | Social skills | Canners b Parent and Teacher Rating Scale, DSM-IV, Social Skills Rating System (SSRS), Raven’s Progressive Matrices a | 20/Available sampling | 12-Jul | Iran/Tehran |
| Moradi et al. (29) | Symptoms of attention deficit/hyperactivity | DSM-IV-TR and Children Pathological Symptoms | 40/Cluster sampling | 12-Sep | Iran/Tabriz |
| Salehi et al. (21) | Self-perception | CSI-4, The Harter perceived competence scale | 40/ Multi-stage sampling | 11-Sep | Iran/Tehran |
| Shoshtari et al. (30) | Attention | DSM–V or DSM–IV, Clinical Interview | 30/Random cluster sampling | 6-May | Iran/Isfahan |
| Dehghan et al. (24) | Behavioral disorder | DSM-IV-TR; American Psychiatric Association | 26/Random sampling | 8-May | Iran/Tehran |
| Sahebanet al. (26) | Reduction symptoms of attention deficit and hyperactivity | DSM-IV ADHD Symptom on the ADHD Checklist and clinical interview | 40/Random | 12-Jul | Iran/Isfahan |
| selection sampling | |||||
| Yaghubi et al. (17) | Reducing ADHD | Canners Continuous Performance Test (CPT), Iran Tova, WISC-R, Canners Parents Rating Scale (CPRS), IVA, DSM-IV-TR | 16/Available sampling | 8 - 9.6 months | Iran/Did not Specify the area |
| Saadat. (31) | Improvement of ADHD symptoms | Child symptom Inventory (CSI-4) | 80/Available sampling | 12-Sep | Iran/Shiraz |
| Shafieian (32) | Increase attention and decrease hyperactivity | Child symptom Inventory (CSI-4) | 14/Available sampling | 11-Aug | Iran/Tehran |
| Hagighi (33) | Decreasing intensity of ADHD | Child symptom Inventory (CSI-4) | 24/Available sampling | 12-Jul | Iran/Isfahan |
| Rahmanzadeh. (34) | Reducing ADHD symptoms | Canners Parent & Teacher Rating Scale, CSI-4 | 30/Random sampling | 12-Jun | Iran/Javanrod |
| Abedi et al. (35) | visual and auditory attention of pre-school boys | Nepsy, Snap-IV scales and Clinical Interview | 30/Cluster sampling | 6 | Iran/Isfahan |
| Hashemi Nosrat Abad et al. (36) | Reducing ADHD symptoms and inattention | DSM-4, CSI-4 | 60/Screening method | 10-Sep | Iran/Did not specify the area |
| Egeland et al. (37) | Working memory in ADHD | F-90 ICD-10, DSM-IV, Neuropsychological Test Performance, Canners Continuous Performance, Trail Making Test, | 67/Randomized controlled trial | 12-Oct | Norway/Departments for Child and Adolescent Psychiatry |
| Miranda et al. (38) | ADHD | DSM-IV, Matching Familiar figures Parents and Teacher Ratings of Child Behavior, Progressive Colored Matrices Test, Battery Scale, Behavioral Observation, Behavioral Rating Scales, Low a Conners Teacher Rating scales, Self-Control Rating Scale, WIS-R | 52/Available sampling | 8 - 9.4 months | Spain/Valencia |
| Riahi et al. (39) | Attention deficit hyperactivity disorder | DSM-IV-TR, Canners Rating Scale, Clinical Global Impression Severity (CGI-S), Global Assessment Function (GAF) | 40/Available sampling | 18 and above | Iran/Tehran |
| Hadianfard et al. (28) | Reducing ADHD Male Great Three and Four CSI-4 | 160/Multi-stage random sampling | 12-Aug | Iran/Shiraz |
a Abbreviations: ADHD, attention deficit hyperactivity disorder; CGI-S, clinical global impressions-severity; CSI-4, children symptom inventory-4 (screens for ADHD and other emotional and behavioral problems); DSM-IV, diagnostic and statistical manual of mental disorders; GAF, global assessment of functioning; SSRS, social skill rating system; WIS-R, wechsler intelligence scale for children-revised.
b A test to measure ADHD children.
| Study | Experimental | Control |
|---|---|---|
| Pretest | ||
| Beh Pajooh et al. (18) | 23.50 (3.92) | 24.20 (3.67) |
| Moradi et al. (29) | 24.67 (2.13) | 24.10 (3.33) |
| Salehi et al. (21) | 18.73 (4.16) | 18.73 (3.35) |
| Shoshtariet al. (30) | 15.98 (5.28) | 16.29 (3.67) |
| Dehghan et al. (24) | 71.69 (3.44) | 072.58 (4.40) |
| Saheban et al. (26) | 35.10 (2.79) | 35.25 (02.01) |
| Yaghubi et al. (17) | 20.03 (7.63) | 6.68 (2.54) |
| Saadat (31) | 06.71 (1.86) | 6.30 (1.45) |
| Shafieian (32) | 09.81 (1.61) | 10.00 (1.61) |
| Hagighi (33) | 27.42 (1.67) | 26.91 (2.09) |
| Rahmanzadeh (34) | 45.13 (3.35) | 45.00 (3.85) |
| Abedi et al. (35) | 07.07 (2.18) | 6.93 (2.17) |
| Hashemi Nosrat Abad et al. (36) | 24.20 (4.84) | 23.80 (5.06) |
| Egeland et al. (37) | 29.56 (6.18) | 29.68 (6.52) |
| Miranda et al. (38) | 19.84 (8.54) | 18.69 (12.27) |
| Riahi et al. (39) | 46.00 (6.00) | 45.00 (5.00) |
| Hadianfard et al. (28) | 11.12 (1.31) | 132.02 (1.82) |
a Abbreviation: mean ± SD, standard deviation.
| Study | Experimental | Control |
|---|---|---|
| Posttest | ||
| BehPajooh et al. (18) | 29.40 (3.20) | 23.30 (4.08) |
| Moradi et al. (29) | 18.76 (2.14) | 24.50 (1.51) |
| Salehi et al. (21) | 14.65 (2.44) | 19.67 (4.48) |
| Shoshtariet al. (30) | 10.74 (4.26) | 14.61 (3.04) |
| Dehghanet al. (24) | 54.92 (4.53) | 67.80 (6.18) |
| Saheban et al. (26) | 27.85 (1.75) | 34.10 (1.38) |
| Yaghubi et al. (17) | 12.00 (8.18) | 30.25 (2.73) |
| Saadat (31) | 4.32 (2.15) | 5.98 (1.69) |
| Shafieian (32) | 4.67 (3.66) | 7.91 (3.61) |
| Hagighi (33) | 13.67 (5.44) | 26.75 (2.08) |
| Rahmanzadeh (34) | 28.53 (3.35) | 45.27 (3.84) |
| Abedi et al. (35) | 11.21 (1.18) | 7.08 (2.65) |
| Hashemi Nosrat Abad et al. (36) | 20.20 (2.39) | 24.80 (1.73) |
| Egeland et al. (37) | 29.38 (6.55) | 29.94 (6.67) |
| Miranda et al. (38) | 16.88 (6.02) | 19.04 (5.91) |
| Riahi et al. (39) | 61.00 (6.33) | 53.33 (5.00) |
| Hadianfard et al. (28) | 136.70 (1.85) | 133.80 (1.83) |
a Abbreviation: SD, standard deviation.
To facilitate statistical analysis, the researcher used continuous means as a part of unmatched group from comprehensive meta-analysis software. The results are separated into 3 parts: a) mean, b) standard deviation, and c) sample size for each group. To test treatment results of experimental and control groups which were different, the effect size on all samples of each group was calculated. Significance testing was performed. Means, standard deviations, and Cohen’s d are given in Table 5.
| Study | d | W a | Wd b |
|---|---|---|---|
| BehPajooh et al. (18) | 1.68 | 0.37 | 0.62 |
| Moradi et al. (29) | -3.15 | 2.63 | -8.28 |
| Salehi et al. (21) | -1.45 | 0.10 | -0.15 |
| Shoshtariet al. (30) | -1.06 | 0.55 | -0.58 |
| Dehghan et al. (24) | -2.40 | 0.21s | -0.48 |
| Saheban et al. (26) | -3.99 | 4.03 | -16.09 |
| Yaghubi et al. (17) | -3.35 | 0.14 | -0.47 |
| Saadat (31) | -0.86 | 4.45 | -3.83 |
| Shafieian (32) | -0.89 | 0.27 | -0.24 |
| Hagighi (33) | -3.48 | 0.35 | -1.22 |
| Rahmanzadeh (34) | -4.66 | 0.58 | -2.70 |
| Abedi et al. (35) | 2.16 | 1.79 | 3.80 |
| Hashemi Nosrat Abad et al. (36) | -2.23 | 3.03 | -6.76 |
| Egeland et al. (37) | 4.66 | 0.38 | 1.77 |
| Miranda et al. (38) | -0.36 | 0.34 | -0.12 |
| Riahi et al. (39) | 1.33 | 0.31 | 0.41 |
| Hadianfard et al. (28) | 1.58 | 9.09 | 14.36 |
| Summation | ∑d = -16.47 | ∑w = 28.62 | ∑wd = -19.51 |
a Weight.
b Weight × d.
| Studies | Statistics For Each Study | ||||||
|---|---|---|---|---|---|---|---|
| SD a | SE | S2 | LL | UL | Z | P Value | |
| Beh Pajooh et al. (18) | 1.660 | 0.52 | 0.27 | 0.650 | 2.690 | 3.210 | 0.001 |
| Moradi et al. (29) | -2.04 | 0.43 | 0.19 | -1.99 | 2.89 | -4.74 | 0.001 |
| Salehi et al. (21) | -1.65 | 0.41 | 0.17 | -2.45 | -0.85 | -4.03 | 0.001 |
| Shoshtariet al. (30) | -1.05 | 0.39 | 0.15 | -1.81 | -0.28 | -2.69 | 0.007 |
| Dehghan et al. (24) | -2.37 | 0.53 | 0.26 | -3.38 | -1.37 | -4.64 | 0.001 |
| Saheban et al. (26) | -3.97 | 0.55 | 0.30 | -5.03 | -2.89 | -7.28 | 0.001 |
| Yaghubi et al. (17) | -2.48 | 0.73 | 0.53 | -3.90 | -1.06 | -3.42 | 0.001 |
| Saadat (31) | -0.81 | 0.27 | 0.07 | -1.33 | -0.28 | -3.05 | 0.002 |
| Shafieian (32) | -0.89 | 0.56 | 0.31 | -1.99 | 0.21 | -1.59 | 0.112 |
| Hagighi (33) | -2.69 | 0.56 | 0.32 | -3.79 | -1.59 | -4.78 | 0.001 |
| Rahmanzadeh (34) | -4.45 | 0.70 | 0.49 | -6.02 | -3.27 | -6.62 | 0.001 |
| Abedi et al. (35) | -1.99 | 0.45 | 0.20 | -1.12 | 2.88 | -4.47 | 0.001 |
| Hashemi Nosrat Abad et al. (36) | -2.05 | 0.35 | 0.12 | -2.74 | -1.36 | -5.82 | 0.001 |
| Egeland et al. (37) | -0.09 | 0.24 | 0.06 | -0.56 | 0.39 | -0.35 | 0.73 |
| Miranda et al. (38) | -0.10 | 0.29 | 0.08 | -0.46 | 0.66 | -0.36 | 0.72 |
| Riahi et al. (39) | -1.35 | 0.35 | 0.12 | -0.66 | 2.03 | -3.84 | 0.001 |
| Hadianfard et al. (28) | -1.57 | 0.20 | 0.04 | -1.76 | 1.97 | -7.76 | 0.001 |
| -0.13 | 0.09 | 0.008 | -0.30 | 0.05 | -1.45 | 0.148 | |
a Abbreviations: LL, low limited; SD, standard deviation; SE, standard error; UL, upper limited.
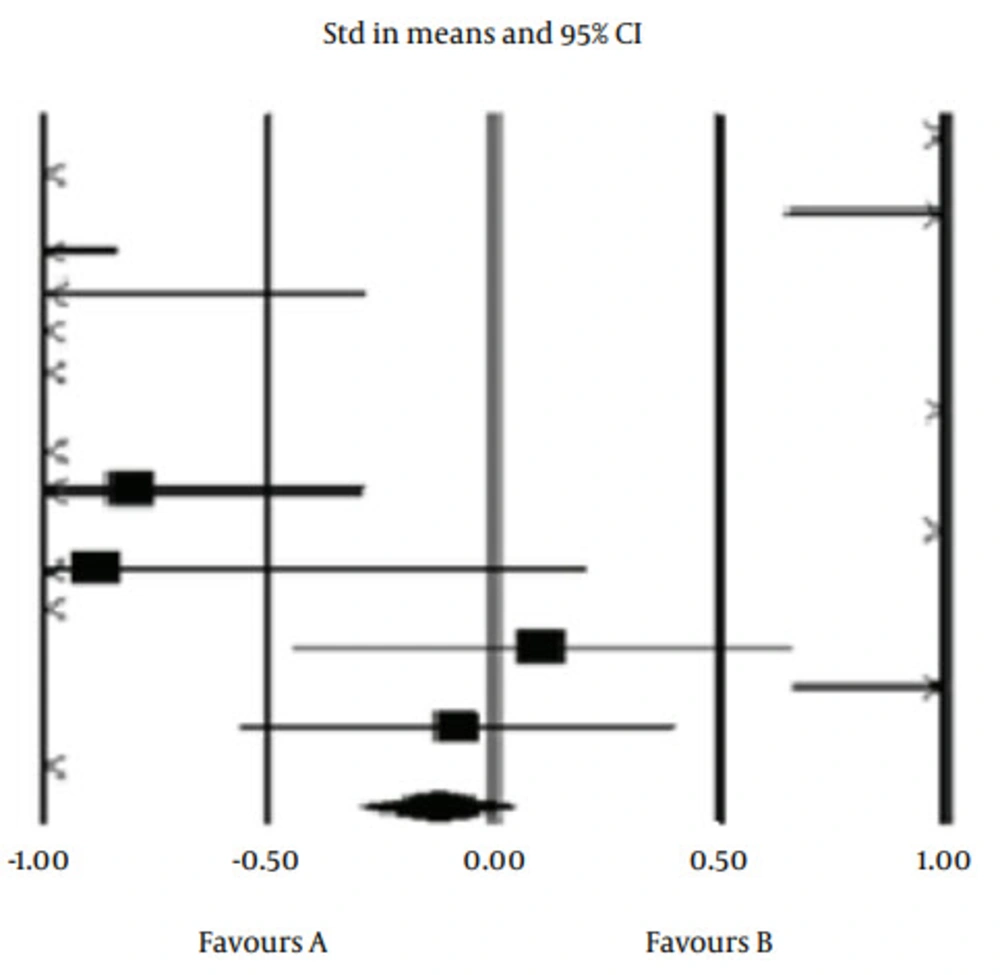
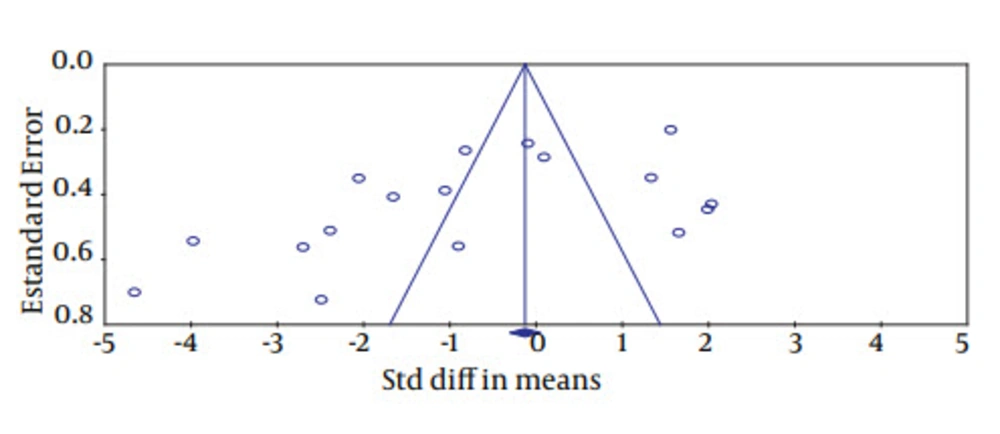
The results of the study illustrated that there is a difference between the mean scores of the experimental and control groups. The overall meta-analysis of these studies illustrated a statistical significance (Figures 1 and 2). In addition, overall standardized differences in means ranged between 0.79% and 95%, confidence interval ranged between 0.57 and 1.08, and Z-value was equal to -1.45 (d = mean d = -0.68 (look at below of Equation 1 and Equation 2)). Furthermore, the Q statistic for heterogeneity of 347.74 is statistically significant (P < 0.001); in addition, I2 = 95.40, T2 = 9.44, SE = 4.30, s2 = 18.41, and Tau = 3.07.
Moreover, in this study, Table 4 indicated that the ADHD symptoms are reduced more in the experimental groups compared to the control groups. Based on this table posttest means of the experimental groups were lower than the posttest means of the control groups in 12 studies. In addition, d average is -0.97 and d (d-= mean, d = -0.68 ), (look at below of Equation 1 and Equation 2.)) is -0.68 which were obtained in Equations 1 and 2
4. Discussion
This study found several interventions that can reduce symptoms of ADHD in children and adolescents. Based on pooled effects, the mentioned treatments can reduce social skills difficulty and behavioral problems. According to the study by Cohen, low effect is below 0.20, median effect is 0.50, and high effect is 0.80 (41). This should be taken into consideration, as there were a range of intervention and evaluation methods. These overall results described that about 75% of children and adolescents in the experimental groups showed a greater reduction in symptoms of ADHD than children and adolescents in the control groups. Effects from studies on far transfer of working memory therapy, cognitive-behavioral therapy and neurofeedback, and ritalin and the combinations of drugs prescribed reduced the symptoms of ADHD in higher percentages of children compared to the control group.
The aim of this study was to perform a comparative study on the effects of treatment programs in reducing ADHD symptoms in children. Results of this study demonstrated that treatments with the highest levels of effectiveness (> 0.80) included cognitive-behavioral therapy, pharmacological treatment, and combinational treatment. This study, like the meta-analysis by Nigg et al. showed that treatment programs reduced symptoms of ADHD in children and adolescents (42).
The difference between overall mean change for treatment and control groups ranged from -0.08- to- 4.45. This showed that the groups receiving treatment programs illustrated significantly larger improvements in term of ADHD symptoms. Consistent evidence from both experimental and quasi-experimental studies suggests that treatment programs had desirable effects for the majority of ADHD studies (43, 44). Effective treatment programs for ADHD students reduced problems in social skills and academic performance, and behavior disorders, which are the cause of the disruption of daily life functioning. These treatment programs are a necessity for children with ADHD in order to overcome the challenges that accompany an ADHD diagnosis over the course of their education. Consequently, improvements in daily life functioning and decreasing of functional disorders are the important, socially suitable standards against which treatment results must be evaluated. The majority of studies regarding effective treatment programs on ADHD illustrated that treatment programs are effective on ADHD.
4.1. Conclusions
In this meta-analysis, the treatment programs used included cognitive treatments, cognitive-behavioral treatments, behavioral treatments, pharmacological treatments, and combinational treatments. Previous studies have demonstrated that students, who received treatment in the various therapy programs, had a higher potential of being mainstreamed into society and showing improvement in their academic and social skills in comparison to students who did not receive some types of therapy. Based on the findings of this research, it is recommended that cognitive-behavioral treatment and pharmacological treatment be used for a higher rate of success in aiding with the ADHD symptoms in children and adolescents.