1. Introduction
Iran has a long and hard-to-control border with Afghanistan, the main producer of illegal opiates in the world. Across this border opioid drugs are smuggled into the luxurious drug markets of European countries (1). According to a national epidemiologic study conducted by Ministry of Health, there are more than 1.2 million opioid dependents in the country (2). A more recent study estimated the number of drug dependents by indirect methods at 1.2 million that most of them were opioid users (3). A rapid change in opiate use patterns during recent years from opium to heroin and from smoking to injection has made the opioid dependence epidemic more problematic (4). Using unsterile syringe and injection equipment is the most prevalent route (69.2%) of HIV transmission among all registered HIV positive cases (5). To respond to HIV epidemic among people who inject opioid, the methadone maintenance treatment was launched in 2002 and scaled up rapidly across the country.
Currently, opioid maintenance, treatment programs, and short-term medically assisted withdrawals are delivered through a network of certified drug treatment centers. Furthermore, opioid maintenance treatment could successfully decrease cue-induced cravings among opioid users (6), however, they are less effective in reducing stress-induced cravings (7). Hypothetically, new approaches of psychotherapies that focus on mindfulness and acceptance might enhance anti-craving properties of opioid maintenance treatment through reducing stress-induced cravings. Mindfulness-based therapies are new approaches in psychotherapy that integrate spiritual traditions such as mindfulness meditation with classic behavioral therapy approaches (8). Mindfulness helps clients to learn how to monitor their own mental processes free of judgment and without being caught up in the actual content of their thoughts. The core skill in mindfulness is the capacity to respond to aversive cognitions, sensations, and emotions with greater acceptance, present moment awareness, and a nonjudgmental attitude (9). Through mindfulness practices, the content of the thought becomes less important than the extent of the individual’s awareness and reaction to it and its occurrence (9).
Mindfulness-based therapies have proved to be effective in a wide range of physical and psychological problems such as chronic pain (10), depression, anxiety, and stress among college students (11) or people with subarachnoid hemorrhage (12), psychosocial stress (13), and depression (14), as well as distinct psychiatric disorders, including hypochondriasis (15), social phobia (16), generalized anxiety disorder (17), obsessive-compulsive disorders (18), and somatization disorder (19). Mindfulness-based relapse prevention (20) is a program integrating mindfulness meditation practices with traditional relapse prevention (RP). The program was tested and proved its effects in decreasing relapses in different groups of drug users, (21). Similar mindfulness-based programs for substance abuse have been shown to increase compliance, cognitive control, regulation of emotions, and reduce stress in alcohol dependents (22, 23) as well as some other similar influences (24).
The effectiveness of mindfulness in different populations of drug users suggests that more trials (in which the type of ‘Mindfulness-based Group Therapy’ was clearly defined and described) were required to establish the efficacy of Mindfulness-based Group Therapy for opioid dependence treatments.
2. Patients and Methods
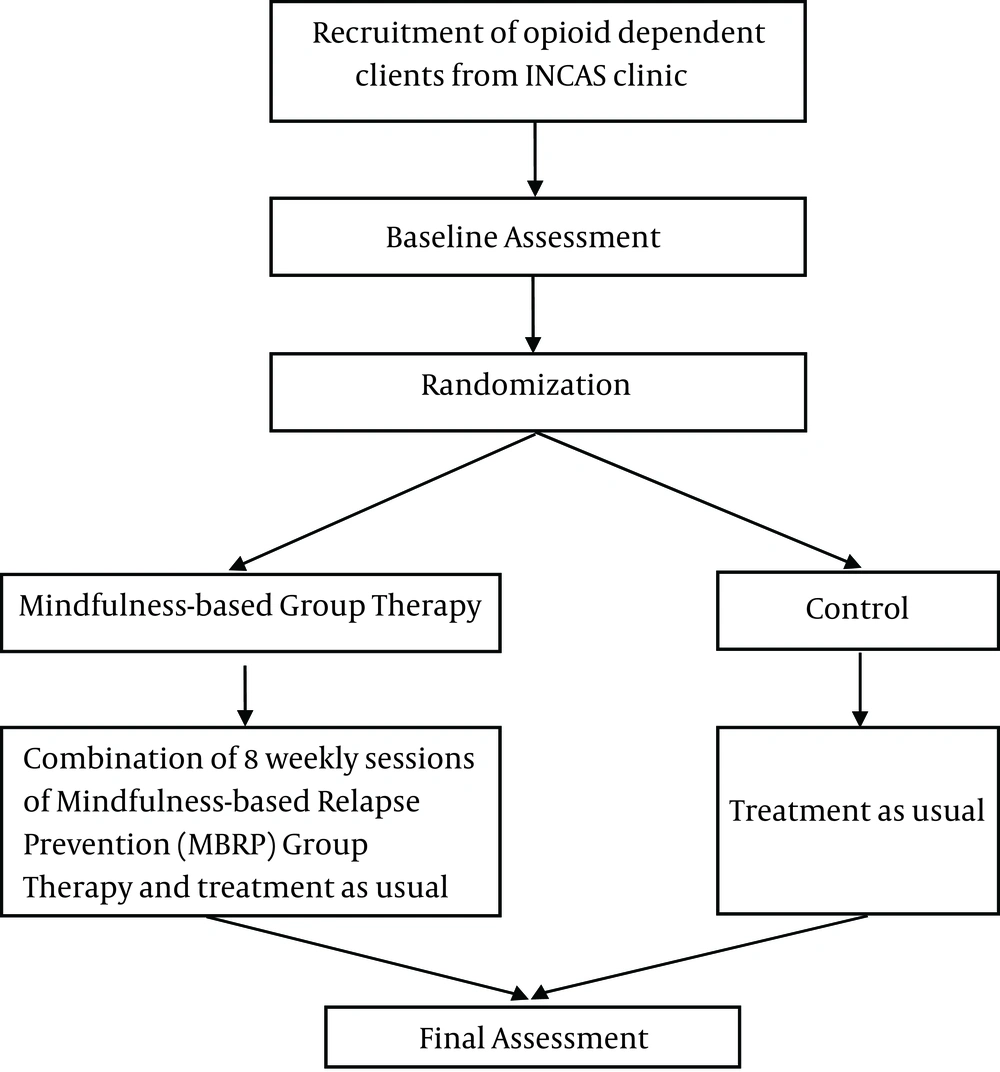
This study was a pilot, randomized, parallel group, one to one controlled trial investigating feasibility, acceptability and effectiveness of mindfulness-based group therapy to improve treatment outcomes in opioid dependent clients.
2.1. Inclusion Criteria
The opioid dependent clients receiving treatment as usual in Iranian National Center for Addiction Studies (INCAS) were randomly assigned to intervention and control groups. INCAS Clinic is located in southwest of Tehran, Iran and provides assisted withdrawal and maintenance treatment with opioid agonist medications, including methadone and buprenorphine for its opioid dependent clients (96.6% male). Inclusion criteria were as follows: (1) diagnosis of opioid dependence according to DSM-IV-TR criteria, (2) age range 18 to 40 years, (3) at least 8 years of completed education (5), stabilization on medical treatment (4), and informed written consent for participation in the study. The exclusion criteria were psychosis, dementia, imminent suicide risk, organic brain disorders, diagnosis of other drug dependence (except nicotine), or non-stabilization on 2-week medical treatments.
2.2. Content of the Interventions
Intervention was a combination of 8-session mindfulness-based group therapy developed by Bowen et al. and the usual treatment provided to opioid dependents in INCAS clinic (Figure 1). The study was designed in a manner to be comparable to other studies of mindfulness-based group therapy for addiction treatment. There was an English manual available to deliver the intervention (20), which described it as a structured intervention. One of the authors translated the manual to Farsi, which was edited by an addiction expert with a PhD in clinical psychology. The therapy sessions held in a closed-group format and conducted on a weekly basis. Each session lasted 120 minutes. It was a structured intervention with a predefined title and content for each session, and the sessions were kept in sequence. Table 1 outlines an overview of the topics and themes that were covered in each session. Although each session had a central theme, the sessions were intended to build upon previous week’s practices.
| Session | Central Theme |
|---|---|
| Automatic pilot and relapse | |
| Awareness of triggers and cravings | |
| Mindfulness in daily life | |
| Mindfulness in high risk situations | |
| Acceptance and skillful actions | |
| Seeing thoughts as thoughts | |
| Self-care and lifestyle balance | |
| Social support and continuing practice |
All study participants received medical treatment through opioid agonist medications in outpatient INCAS clinic according to national protocols (25). The methadone or buprenorphine administration was conducted through regular visits by certified physicians that were more frequent during the first week of treatment and gradually decreased to at least one visit per week. Clients who received maintenance treatment should have come to the clinics for daily supervised dosing during the first two months of treatment. The take-home doses were allowed 1 d/wk from the beginning of the third month, which could increase from 1 d/mon to at most 6 d/wk contingent to appropriate compliance and negative weekly urine tests for morphine and methamphetamine. The baseline, weekly, and end of the treatment study assessments are presented in Table 2.
| Instrument | Baseline | Weekly | 8 Weeks Follow up |
|---|---|---|---|
| √ | |||
| √ | √ | √ | |
| √ | √ | ||
| √ | √ | ||
| √ | √ | ||
| √ | √ | ||
| √ | √ |
2.3. Sample Size Calculation
The study participants recruited in INCAS in the autumn of 2013. Thirty eligible individuals were selected randomly for participation in the study; 15 of them were assigned to each intervention group. In order to have consistency in seasonality across assessment points, the assessment obtained in the autumn of 2013 served as the baseline or pretest assessment point for the main substantive intervention outcome analysis and the winter of 2013 assessment served as the outcome time point for the analysis report; hence, this was an experimental research design.
2.4. Statistical Analysis
To determine legitimate numerical codes, data cleaning was performed by both graphical and descriptive statistics to ensure data accuracy, check out-of-range values for categorical variables, and make sure that mean and standard deviations were within the plausible ranges for continuous composite variables (29). The patterns of missing data were checked regarding how much and why they were missing. Results of SPSS MVA (missing values analysis) using t test (α = 0.05) for outcome composite variables were checked to ensure that patterns of missing data in outcome variables were not related to population’s demographic variables such as sex, area of residency, and group (intervention vs. condition). Distribution of scores on continuous variables was checked for univariate (P < 0.001) and multivariate normality using LISREL, version 8.72 (30). T test and chi-square test were conducted to match the intervention and control groups with respect to demographic variables. Repeated measure analysis of variance was used to test the effectiveness of mindfulness-based group therapy in the study population.
3. Discussion
To the best of our knowledge, this is the first study to test the acceptability and efficacy of ‘Mindfulness-based Group Therapy’ versus ‘Treatment as Usual’ for opioid dependent clients in Iran. There are some potential limitations regarding the present study that merit discussion. One potential concern is the random assign of the participants to their study condition, which may lead to realize whether or not they are receiving the added group therapy. When the participants prefer one group to the other, this might disappoint them, which may negatively affect the treatment outcome. However, since the study intended to investigate the effect of adding the mindfulness-based group therapy to treatment as usual, the current design remains most appropriate as it is closer to a real world situation. After the mindfulness-based group therapy session, the study participants were advised to report their participation in self-help programs during the course of the therapy. As it is not possible to monitor participants’ behavior during this period, self-reports about their use of other treatment programs should be trusted. Throughout the recruitment, the mindfulness-based group therapy sessions and its follow-ups, it was emphasized to the participants that their honest information was crucial and there would be no consequences if they participated in other methods. It is hoped that by conveying this message to the participants, they were motivated to cooperate throughout the study and provide their honest reports about their experiences during study assessments. The results of the present study indicate whether mindfulness-based group therapy can improve the outcome of opioid dependence treatment in the context of Iran drug treatment services.