1. Background
Comorbidity of anxiety and depression is substantially high, about 55% to 76% of the individuals with a lifetime history of major depression and anxiety report anxiety and depression respectively (1). Furthermore, patients with comorbidity of anxiety and depression have earlier age of onset, greater likelihood of suicide, greater symptom severity, higher chronicity, greater impairment in functioning and poorer overall quality of life (2-5).
Traditionally, cognitive-behavioral therapy focuses on specific disorder approach. Specific manuals are developed that account for the assessment and treatment protocols in specific disorders. Clinicians and therapists are trained according to these manuals, but the high comorbidity among emotional disorders, especially anxiety and unipolar mood disorders leads many researchers and clinicians to find out the reasons and explanations that illuminate this darkness (6). These struggles open the scientific gate to exploring shared processes common across multiple disorders including depression and anxiety, called transdiagnostic components. The transdiagnostic approach assumes an incremental value to understand these shared maintenance factors underlying psychological disorders.
Many surveys are done regarding the role of some of the transdiagnostic components in many mental disorders especially depression and anxiety. Some of these studies try to answer what differences there are between patients with anxiety and those with depression in almost each of these common vulnerabilities. Most of the aforementioned studies found no differences (7-13), but some others revealed small or medium differences (14-16).
In addition to the interrelationship between all shared vulnerabilities to anxiety and depression symptoms, there is evidence supporting the idea of correlations of some of these common factors. For example, worry and rumination are cognitive processes called repetitive negative thoughts. These two variables are highly correlated with each other; however remain as separate variables that predict depression and anxiety symptoms over time (17). Furthermore, there are significant relationships between neuroticism and rumination, worry and depression (17). Another study showed significant correlation between worry, rumination, intolerance of uncertainty and anxiety symptoms. Results showed that worry partially mediated the relationship between intolerance of uncertainty and anxiety and rumination fully mediated the relationship between intolerance of uncertainty and depression symptoms (18). In addition, rumination and worry are considered by different researchers and clinicians as different kinds of avoidance and emotion regulation strategies (19, 20). Suppression as one of the emotion regulation strategies is considered a kind of experiential avoidance (21).
From a more specific perspective, some of these shared variables are mediators which connect other common components such as neuroticism and experiential avoidance to anxiety and depression. For example, emotional avoidance and non-acceptance of negative emotions are associated with anxiety and depressive related psychopathology (10, 12, 22). Furthermore, experiential avoidance predicts depression and anxiety such as posttraumatic stress disorder (PTSD) (23, 24). In addition, evidence shows that experiential avoidance is more than an emotional disorder phenomenon and may have a casual effect on the course of emotional disorder (23, 25). Individuals with anxiety and depressive symptoms use emotion regulation maladaptive strategies to avoid experiencing negative and unwanted emotions; therefore, emotion regulation has mediating effect in the relationship between some common factors such as neuroticism and experiential avoidance, and anxiety and depression symptoms, and their related psychopathology. The mediating role of emotion regulation is demonstrated in some researches (26) and has been the treatment target in several recent treatment approaches (27, 28).
While difficulties in emotion regulation and maladaptive emotion regulation strategies contribute to emotional disorders, personality traits such as neuroticism may also play a pivotal role in etiology and maintenance of emotional disorders (29, 30). Moreover, there is a strong relationship between neuroticism and emotion regulation deficits (31, 32).
The boundaries between transdiagnostic components including emotion regulation components (emotional clarity, non-acceptance of emotion, etc.), worry (as an emotion regulation strategy), experiential avoidance and neuroticism are unclear (33, 34); hence, further study is needed to determine which of these variables have more casual role in relation to other variables for prediction anxiety and depression as emotional disorder symptoms.
2. Objectives
The current study aimed to assess the mediating roles of emotion regulation deficits and worry, as a maladaptive emotion regulation strategy, between experiential avoidance and neuroticism (as independent variables), and anxiety and depression symptoms (as dependent variables).
3. Materials and Methods
3.1. Study Population and Sampling
The study population was university students. Three hundred and thirty individuals at university of social welfare and rehabilitation sciences, Tehran University of Medical Sciences and Iran University of Medical Sciences volunteered to complete a series of questionnaires (through convenient sampling). Fourteen participants were dropped from the sample due to missing data and deleting outliers after data cleaning, resulting in a sample size of 316 individuals.
3.2. Materials
To assess experiential avoidance and neuroticism as independent variables, worry and emotion regulation as mediator variables, and anxiety and depression as dependent variables, authors employed acceptance and action questionnaire-II (AAQ-II), the neuroticism scale of shortened and revised form of Eysenck personality questionnaire scale (EPQ-RS), Penn state worry questionnaire (PSWQ), difficulties in emotion regulation scale (DERS), Beck anxiety questionnaire (BAI) and Beck depression questionnaire (BDI-II), respectively.
3.2.1. Acceptance and Action Questionnaire-II
The acceptance and action questionnaire (AAQ-II) was first developed in 2004 (35). To reduce defects of the former version and make it more applicable, the second version of AAQ-II was then developed (36). It is a 10-item scale and assesses the tendency to evaluate unwanted thoughts and feelings negatively, not accept and try to alter or escape from them (37). In total, it refers to a construct meaning acceptance, experiential avoidance and psychological flexibility. Responses range from 1 (never true) to 7 (always true) with higher scores reflecting greater psychological flexibility. The AAQ-II yields one single factor referred to as experiential avoidance. The mean alpha coefficient is reported 0.84 (0.78 - 0.88) and the three- and twelve-month test-retest reliability values were 0.81 and 0.79 respectively (36). The internal consistency of the Persian version of the AAQ-II in general and clinical population is high, α = 0.71-0.84. Moreover, avoidance of emotional experiences significantly correlated with depressive and anxiety symptoms as well as poor mental health (38).
3.2.2. The Neuroticism Scale of Shortened and Revised Form of Eysenck Personality Questionnaire Scale
EPQ-RS is a 48-item scale. It consists of four subscales: introversion (stability /emotionality) extraversion (extraversion/introversion), psychoticism and a lie subscale to reveal falsehood. The neuroticism subscale is a 12-item subscale with dichotomous (yes or no) answers. It is used for the age range 16 - 70 years. The internal consistency (α) for the neuroticism subscales for male and female were α = 0.84 and α = 0.80, respectively (39). Psychometric properties of Iranian version of EPQ-RS are reported acceptable with high internal consistency, r = 0.74 (40).
3.2.3. Penn State Worry Questionnaire
The PSWQ is a 16-item measure consisting of statements about worry. Each statement is scored on a 5-point Likert scale ranging from 1 to 5 yielding a total score ranging from 16 to 80, with higher scores indicating greater worry levels (41). The scale has very good internal consistency (α = of 0.93) and high test-retest reliability (r = 0.74 - 0.93) (41). The PSWQ has also quite favorable internal consistency in patients with generalized anxiety disorder (GAD), different anxiety disorder groups (0.86 to 0.95) and the control group (0.90) (42). Psychometric properties of Persian version of the scale had high internal consistency (0.88) and test-retest reliability (0.79). In addition, the significant correlation between PSWQ and two variables of trait anxiety (0.68) and depression (0.49) indicated good validity of PSWQ (43).
3.2.4. Difficulties in Emotion Regulation Scale
The DERS is a 36-item scale (44) and assesses individuals’ typical tendencies toward emotion regulation. It consists of several facets such as: 1- Non-acceptance of emotional responses (NONACCEPTANCE); 2- Difficulties engaging in goal directed behaviors (GOALS); 3- Impulse control difficulties (IMPULSE); 4- Lack of emotional awareness (AWARENESS); 5- Limited access to emotion regulation strategies (STRATEGIES) and 6- Lack of emotional clarity (CLARITY). The DERS has high internal consistency (α = higher than 0.80 for each subscale) and good test-retest reliability (r = 0.88). It also has adequate construct and predictive validities (45). Persian version of PSWQ has high internal consistency (α = 0.86). Furthermore the correlation between DERS and Zuckerman-Kuhlman personality questionnaire was significant, showing acceptable validity of the questionnaire (46).
3.2.5. Beck Anxiety Questionnaire
The BAI consists of 21 items in a 4-point Likert scale that assesses cognitive and somatic symptoms of anxiety. Scores range from 0 to 63, with higher scores indicating higher levels of anxiety (47). BAI has high internal consistency (α = 0.92) and test-retest reliability over a week (r = 0.75). In addition, the correlation between BAI and the revised Hamilton anxiety rating scale is moderate (0.51) (48). Good and acceptable psychometric properties are reported by other studies in clinical and non-clinical samples (49, 50). The Persian version of BAI has a good reliability (0.72), a very good validity (0.83) and an excellent internal consistency (Alpha = 0.92) (51).
3.2.6. Beck Depression Questionnaire
BDI-II comprises of 21 items that assesses severity of depression disorder. Each item is scored on a Likert scale from 0 to 3, with higher scores indicating greater depressive symptoms. Total scores are obtained by summing all items and range from 0 to 63 (52). BDI mean coefficient alpha is reported 0.86 in psychiatric populations and 0.81 in non-psychiatric populations. Its mean test-retest reliability is reported 0.86 (47). In Iran, in a study on 354 patients with recovered depressed, coefficient alpha, test-retest over a week and convergent validity (with BDI) were reported 0.91, 0.81, and 0.61, respectively (53).
3.3. Procedure
Participants were recruited from university campuses and dormitories. After signing informed consent and answering any of their questions about the research, they were given a packet of questionnaires. They received a gift to participate in the research. The current study was approved by the ethics committee of medical school. Furthermore, participants were assured that their demographic information would be kept confidential. They were informed that they could leave the research during administration whenever they wished.
3.4. Statistical Analysis
The current cross-sectional study used path analyze via regression by SPSS ver. 20 to analyze the data. The recommended procedure and evaluative criteria of Baron and Kenny (54) were used to assess possible mediation. Experiential avoidance and neuroticism were independent variables, emotion regulation and worry (as a kind of emotion regulation strategy) were mediator variables, and anxiety and depression were dependent variables.
4. Results
The sample consisted of 160 (50.6%) females and 156 (49.4%) males with the mean age of 22.3 (SD = 2.89), ranged from 18 to 35 years. In terms of marital status, 94.9% were single and 5.1% married. In terms of educational level, 56.6% were undergraduate and 43.4% graduate students (master student = 33.5% and doctoral student = 9.8%).
Raw mean scores, standard deviations and correlations among all main study variables are reported in Table 1. After making sure that multicollinearity was not a problem, a series of regression analysis was done to assess these four hypotheses: 1, There are significant relationships between experiential avoidance and anxiety, experiential avoidance and depression, neuroticism and anxiety, and neuroticism and depression; 2, There are significant relationships between experiential avoidance and emotion regulation, experiential avoidance and worry, neuroticism and emotion regulation and neuroticism and worry; 3, There are significant relationships between emotion regulation and anxiety, emotion regulation and depression, worry and anxiety, worry and depression and all of the aforementioned relations are met; 4, There are significant relationships between all independent variables (experiential avoidance, neuroticism, emotion regulation and worry) and dependent variables (anxiety and depression).
a*P < 0.001
bAAQ-II: acceptance and action questionnaire-II (experiential avoidance).
cEPQ-RS: Eysenck personality questionnaire scale (neuroticism subscale).
dDERS: difficulties in emotion regulation scale (emotion regulation).
ePSWQ: Penn state worry questionnaire (worry).
fBAI: Beck anxiety questionnaire Beck anxiety questionnaire (anxiety).
gBDI-II: Beck depression questionnaire (depression).
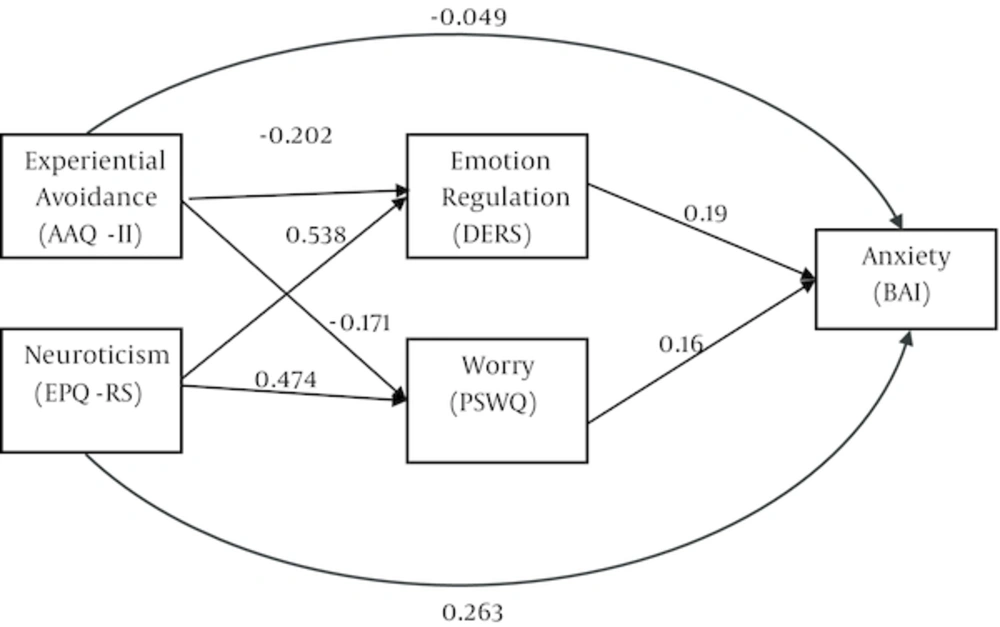
The first regression analysis used AAQ-II and neuroticism as predictor variables and BAI as dependent variable: experiential avoidance (beta = -0.115, t = -2.105, P < 0.036) and neuroticism (beta = 0.440, t = -0.8.078, P < 0.001) were significant predictors of anxiety, R = 0.502, F (2, 313) = 52.591, P < 0.001. The second regression analysis used AAQ-II and neuroticism as independent variables and DERS as dependent variable: both AAQ-II (beta = -0.202, t = -4.224, P < 0.001) and neuroticism (beta = 0.538, t = 11.271, P < 0.001) were significant predictors of DERS, R = 0.653, F(2, 313) = 116.055, P < 0.001; for the second mediator, another analysis used AAQ-II and neuroticism as independent variables and PSWQ as dependent variable: both AAQ-II (beta = -0.171, t = -3.311, P < 0.001) and neuroticism (beta = 0.474, t = 9.175, P < 0.001) were significant predictors of PSWQ, R = 0.571, F (2, 313) = 75.728, P < 0.001. The third regression analysis used DERS and PSWQ as independent variables and BAI as dependent variable: both DERS (beta = 0.328, t = 5.501, P < 0.001) and PSWQ (beta = 0.243, t = 4.083, P < 0.001) were significant predictors of BAI, R = 0.508, F (2, 313) = 54.471, P < 0.001. The fourth regression analysis used all AAQ-II, neuroticism, DERS and PWSQ as independent variables and BAI as dependent variable: all variables including AAQ-II (beta = -0.049, t = -0.9, P < 0.369), neuroticism (beta = 0.263, t = 4.041, P < 0.001), DERS (beta = 0.19, t = 2.864, P < 0.004), and PSWQ (beta = 0.16, t = 2.612, P < 0.009) were significant predictors of BAI, R = 0.549, F (4, 311) = 33.576, P < 0.001.
In total, results showed that PSWQ especially DERS were mediating the relationship between neuroticism and BAI partially and the relationship between AAQ-II and BAI fully. The path model of the results is presented in Figure 1.
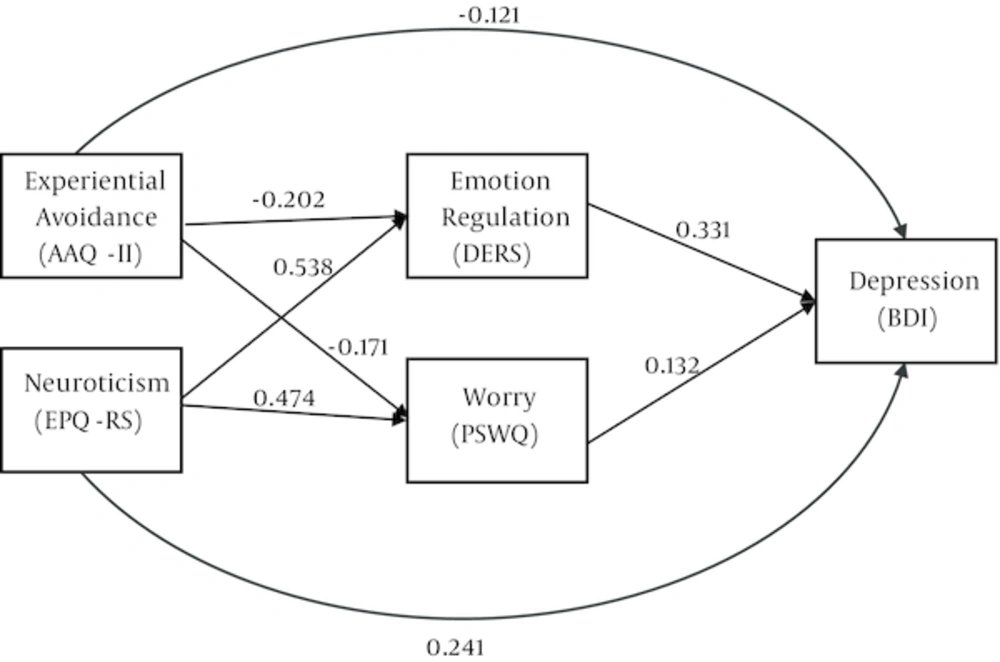
To predict depression, another series of regressions were done. The first regression analysis used AAQ-II and neuroticism as predictor variables and BDI as dependent variable: experiential avoidance (beta = -0.211, t = -4.2, P < 0.001) and neuroticism (beta = 0.481, t = 0.9.597, P < 0.001) were significant predictors of BDI, R = 0.605, F (2, 313) = 90.238, P < 0.001. The second regression analysis used AAQ-II and neuroticism as independent variables and DERS as dependent variable: both AAQ-II (beta = -0.202, t = -4.224, P < 0.001) and neuroticism (beta = -0.538, t = -11.271, P < 0.001) were significant predictors of DERS, R = 0.653, F (2, 313) = 116.055, P < 0.001; for the second mediator, another analysis used AAQ-II and neuroticism as independent variables and PSWQ as dependent variable: both AAQ-II (beta = -0.171, t = -3.311, P < 0.001) and neuroticism (beta = 0.474, t = 9.175, P < 0.001) were significant predictors of PSWQ, R = 0.571, F (2, 313) = 75.728, P < 0.001. The third regression analysis used DERS and PSWQ as independent variables and BDI as dependent variable: both DERS (beta = 0.438, t= 9.067, P < 0.001) and PSWQ (beta = 0.223, t = 4.196, P < 0.001) were significant predictors of BDI, R = 0.638, F (2, 313) = 107.460, P < 0.001. The fourth regression analysis used all AAQ-II, neuroticism, DERS and PWSQ as independent variables and BDI as dependent variable: all variables including AAQ-II (beta = -0.121, t = -2.521, P < 0.012), neuroticism (beta = 0.241, t = 4.205, P < 0.001), DERS (beta = 0.331, t = 5.682, P < 0.001), and PSWQ (beta = 0.132, t = 2.457, P < 0.015) were significant predictors of BDI, R = 0.677, F (4, 311) = 65.768, P < 0.001.
In total, results showed that PSWQ especially DERS were mediating the relationship between neuroticism and BDI and the relationship between AAQ and BDI, partially. The path model of the results is presented in Figure 2.
5. Discussion
As hypothesized, present data support the notion that both neuroticism (negative affect) and experiential avoidance predict anxiety and depression symptoms independently; and also mediate the effects of difficulties in emotion regulation and worry. It appears that heightened neuroticism is associated with increase in difficulties in emotion regulation and worry which contribute to anxiety and depression symptoms. Since Watson and Clark proposed the tripartite model, the important role of neuroticism or negative affectivity is underscored in the etiology and maintenance of anxiety and depression as a common factor (55). In fact, individuals with high neuroticism may be more prone to anxiety and depression symptoms (56, 57). However, many individuals with heightened neuroticism may not exhibit high levels of anxiety and depressive symptomatology; therefore, there may be other factors which mediate or moderate the relationship between neuroticism and anxiety and depression symptoms such as emotion regulation and worry shown in the present study. The mediating effect of emotion regulation in the relationship between negative affect and anxiety and depression was demonstrated previously (58). A study using structural equation modeling tested the relationship between negative affect, emotion regulation and psychological distress in clinical and nonclinical samples; it suggested that negative effect leads people to control negative emotions via maladaptive emotion regulation strategies and these lead to psychopathology (59). Similar findings were shown by Suveg et al. (60). Neuroticism or negative emotionality as a higher-order factor operates from a distinct motivational system, and the behavioral inhibition system (BIS); therefore, the individuals with high levels of neuroticism exhibit higher levels of BIS sensitivity which is somehow underlying factor of neuroticism and may explain casualty better and more precisely (61). The aversive motivational systems (BIS system) are gaining attention of researchers (62) and the most recent psychological treatments that target emotion regulation strategies and emotion regulation therapy, use the motivation and behavioral approach system (BAS) and inhibition system in conceptualizing and targeting it in corresponded treatment via some emotional and cognitive techniques (63). Therefore, it seems more reasonable and more effective to target some underlying factors such as neuroticism, besides emotion regulation.
Experiential avoidance as an independent variable in the present study has significant relationship with anxiety and depression related psychopathology (22, 25), that is consistent with the results of the current study. Furthermore, people with lower psychological flexibility or higher experiential avoidance level rarely tolerate the negative emotion and to avoid or lessen the experience of negative emotion engage in series of emotion regulation strategies. This will lead to temporary relief, and this negative reinforcement is the cause of repeating maladaptive behavior (34). Additionally, experiential avoidance has robust relationship with emotion regulation and some theorists suggest that the experiential avoidance is a kind of emotion regulation such as suppression (64). The pivotal role of experiential avoidance in the etiology and maintenance of emotional disorders were indicated in some recent and evidence based treatments, such as acceptance and commitment therapy (65), dialectical behavior therapy (66)), mindfulness-base cognitive therapy (67), emotion-focused therapy (68) and the emotion regulation therapy (63).
As mentioned, many researchers tried to find different pathways that connect emotional disorders and common etiological and maintenance factors, but it was not enough. Assessment and psychotherapy areas need more subtle investigation to find out the route to more straight, economical and effective instrument to assess and cue emotions and comorbid disorders via affecting fundamental factors.
The current study had a number of limitations that should be addressed. First, the design of the present study was cross-sectional which limited establishment of the casual links. Furthermore, the analysis method was path analysis via regression with some limitations, path analysis or structural equation modeling using Amose and other more advanced methods with fewer errors would lead to more valid and reliable results. Second, there was no consistent definition of emotion regulation concept and different approaches yield distinct conceptualization and related instruments to assess the concepts; therefore, the measure of emotion regulation used in the present study was just one of many instruments designed to assess emotion regulation, and the results of the present study should be interpreted for other emotion regulation concepts cautiously. Third, the current study used some limited variables as mediators and there were more transdiagnostic variables that may be mediating the relationships between other common underlying factors and emotional disorders. Hence, future studies are needed to examine the mediating or moderating roles of variables. Finally, the present study sample was nonclinical; therefore, future studies should be done on clinical samples.