1. Introduction
Fecal impaction (FI) is a disorder characterized by the inability to evacuate large mass of compacted faces at any level of lower GI tract (1). It is commonly found in the rectum. The population with the highest risk for FI are elderly patients with neuropsychiatric disorders such as Alzheimer disease, Parkinson disease, dementia, and severe stroke (2). The main risk factor for FI is old, however, it can occur at any age (1, 3). From a pathophysiological aspect, fecal impaction causes an intraluminal pressure increase of the colon, which may lead to ulceration and perforation (4). The typical symptoms of FI are those found in any type of intestinal obstruction including abdominal pain, distention, nausea, vomiting, and anorexia (5). In addition, sustained dilation of the colon may lead to a megacolon (6). FI can compress nerve, vascular, or solid organ structures (7). FI is also responsible for hospital admissions (8) and increased morbidity-mortality rates (5). Clozapine is an antipsychotic drug that can be used to manage schizophrenia. It has several side effects such as fatal sepsis and clozapine-related constipation. Several cases have been reported with fatal sepsis, however, unfortunately, clozapine-related constipation is not always diagnosed early in its course. If not recognized early, the consequences can be serious and deleterious (9).
2. Case Presentation
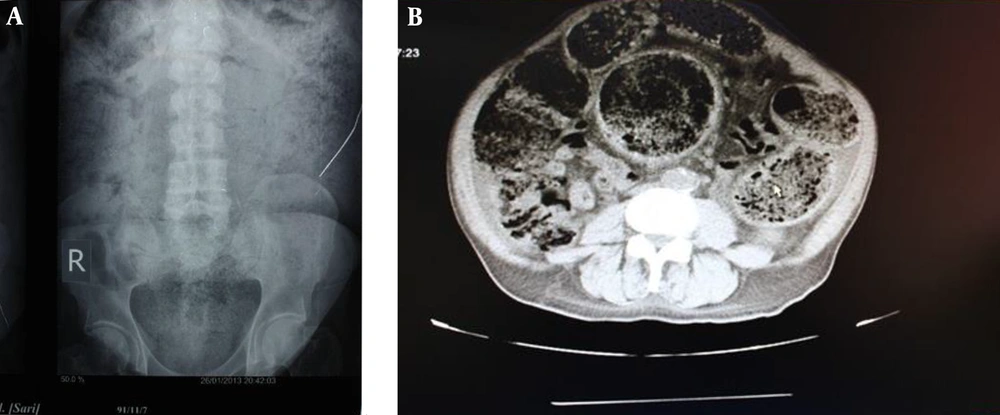
A 63-year-old man visited the gastrointestinal clinic due to a history of constipation for 4 weeks, characterized by a lack of urge to defecate, as well as hard stool. He had no bowel movements over 20 days with abdominal distention, abdominal pain in hypogastric region, vomiting, anorexia, frequency, and nocturia. He has lost 8 kg in the past 6 months. His past medical records showed that he was being treated for schizophrenia with clozapine (100 mg TDS for 30 years) and was also using captopril (25 mg ½ tablet BD) and Tamsulosin (0.4 mg/day) for his hypertension and benign prostatic hyperplasia, respectively. He was a smoker (60 pack year) and an opium addict for about 20 years. In the abdominal physical examination, abdominal protrusion was visible. A lobulated stony hard mass occupied the entire abdomen (Figure 1A). Abdominal radiographs (Figure 2A) and computed tomography scan of the patient (Figure 2B) revealed a dilated colon filled with impacted fecal material. A colonoscopy was tried, which was not successful. After a couple of days of saline enema with laxative suppositories and having a poor preparation, a limited left sided and afterwards a full colonoscopy was performed. His upper endoscopy showed a healed duodenal ulcer. Doppler ultrasound of lower limb veins, abdominal, and pelvic ultrasonography was unremarkable. However, ultrasound of his urinary tract showed bilateral hydronephrosis. Routine blood tests showed a moderate normocytic anemia (9.3 g/dL). Thyroid function was normal. Serum potassium was low (2.7 mEq/L), which was corrected in the first days with no effect on bowel habit. Other blood chemistries and tumor markers were all normal.
With daily enemas and manual fecal disimpaction after 16 days, the whole stool bulk was evacuated (Figure 1B). The patient began a liquid diet and then a regular diet. He began having bowel movements every day and gained weight after a few weeks.
3. Discussion
Anticholinergic side effects such as constipation are common in psychiatric patients due to their usage of antipsychotic drugs, especially low-potency first generation antipsychotics and clozapine, and also high prevalence of opioids consumption. Habibisaravi et al. emphasized the importance of substance use among psychiatric patients and its effect on the outcome of a psychiatric illness. They reported a rate of 26.4% opioid and cannabinoid substances or prescription medicines abuse or dependence in their cases. Opium with or without other substances was the most frequent substance abused in 67% of cases. Schizophrenia and mood disorders were the two most common psychiatric disorders in substance abusers or dependent inpatients, however, schizophrenia had a statistically significant association with substance misuse or dependence (10).
As mentioned earlier, constipation is a common side effect of clozapine and in some cases, it can progress to bowel obstruction due to FI or even death (11). There are some reasons that patients with schizophrenia are more at risk in this situation. These patients may have altered sensitivity to pain and this phenomenon may be important in the diagnosis of the acute abdomen (12).
Oke et al. reported a case of a 61-year-old male with unrecognized clozapine-related constipation leading to fatal intra-abdominal sepsis. The patient was being treated for his schizophrenia with clozapine. The abdominal x-ray revealed plenty of feces in the colon suggestive of bowel obstruction from FI (13). Levin et al. reported a patient with a history of chronic paranoid schizophrenia, which had been treated with clozapine (750 mg/d). The laboratory revealed a large bowel obstruction secondary to severe FI affecting the entire colon (14).
Another possible reason is that pain perception is normal, however, schizophrenic patients cannot express the pain that they feel. They may have difficulty in expressing their thoughts in regards to pain. The managing staff should be aware of the complication as early diagnosis prevents advanced complications (15).
The pathophysiology of this kind of constipation has been assumed to be due to an anticholinergic side effect of the medication; however, this has never been investigated. A logical strategy to decrease the symptoms is to minimize the dose of clozapine. Measurement of serum clozapine levels can be helpful. When the serum level of clozapine is 500 - 700 ng/mL or greater serum, we should cautiously have lowered the dose. However, there is a threshold of 350 ng/mL. If the serum level of clozapine was lower than 350 ng/mL, we may have a lack of clinical response. In this situation, we can use quetiapine as a clozapine-sparing agent (14).
One of the common side effects of clozapine is sialorrhea. Clozapine-induced sialorrhea (CIS) occurs at a rate of approximately 30%, although it varies from 10% to 80% in the literature (16). Several treatment options exist, however, in practice, most cases of sialorrhea are not adequately treated due to the fact that available treatment options have limited efficacy or unwanted side effects (17). Drugs in this class include selective (e.g., pirenzepine) or nonselective (e.g., atropine, trihexyphenidyl, benztropine, procyclidine) antagonists at muscarinic receptors. All these drugs have the potential to increase the anticholinergic adverse effects of clozapine (e.g., constipation, urinary retention, blurring of vision, etc.) so treatment of clozapine-induced sialorrhea can worsen the constipation and it may increase the risk of FI. Due to these side effects, these drugs should be used cautiously in patients with narrow-angle glaucoma and prostatic hypertrophy. However, these agents should not be preferred; if administered with clozapine, there may be an increase in central anticholinergic effects, orthostasis, sedation, or lowering of the seizure threshold (18).
Another cause of FI in this patient was the chronic use of opium, which itself can cause bothersome constipation (19). The additive effect of constipation and hypokalemia to the clozapine-induced constipation caused a very severe form of FI, which needed a 20 day course of medical treatment to gain a semi-normal bowel habit in this case (11).
Opioids have different gastrointestinal effects including decreasing gastric emptying and stimulating pyloric tone, anorexia, nausea, and vomiting. They also cause inhibition of propulsion and increased fluid absorption in the intestine result in delayed absorption of medication, hard dry stools, constipation, sense of incomplete rectal evacuation, bloating, and abdominal distention. There are other effects including increased anal sphincter tone, impaired reflex relaxation in response to rectal distention. These effects can result in the inability to evacuate the bowel, abdominal spasm, cramps, and pain (20).
Constipation occurs in about 90% of patients who take opioids even with a single dose. This effect of opioids occurs via opioid receptors in the brain and gastrointestinal tract, in which μ receptors are more involved in this phenomenon (21). These receptors affect pain regulation. They also possibly influence the inhibitory and excitatory neural system of GI muscles (22). As we said, chronic constipation can lead to FI and causes substantial morbidity with reducing the quality of life, considering that constipation is not tolerated over time, a good monitoring and treatment are necessary.
Fecal impaction can be found at any age, especially in old age. A study showed that 42% of the old patients of geriatric wards in the United Kingdom had FI (23). Gurll et al. reported in their study that 39% of patients with FI had a history of prior impaction (24). In some cases, there are some serious complications such as mega-colon, stercoral ulceration, rectovaginal fistula, lower GI bleeding, intussusception, or even perforation (25-27). Elderly patients with dementia or psychosis may present with fecal incontinence of paradoxical diarrhea (5). The aims of treatment in patients with FIs are to relieve symptoms, clear out the colon, and also restore normal bowel habits (28). There are different kinds of management for clearing out the colon including manual disimpaction, distal softening or wash out, and proximal softening or wash out (29). In manual disimpaction, if the hardened stool is palpable in the rectum, removal of the fecal material with a lubricated index finger inserted into the rectum is done. The stool should be broken up using a scissoring motion. The finger is then moved in a circular manner and then bent gently and removed, extracting stool with it (5, 26, 30-32). In distal softening strategy, enemas can be used for softening of the hardened stool and stimulation of evacuation. Each enema solution has characteristics that may be helpful in selected patients; however, most enema solutions contain water and an osmotic agent. One combination that can be used is water, docusate sodium syrup, and sorbitol (24, 33-35). We used a combination of normal saline and glycerin in our patients. During enema administration, the patient should be placed in the left lateral decubitus position (31, 36, 37). Administration of small volumes (1 - 2 L) is more beneficial than a large volume enema. After a few minutes, the patient voluntarily evacuates the enema-stool mixture; abdominal manipulation can often be helpful in evacuation (32, 38). Oral lavage with polyethylene glycol solutions can be used in proximal softening or washout. This strategy is contraindicated when a complete bowel obstruction exists (39). Youssef et al. reported that 1 to 1.5 g/kg/d of polyethylene glycol solution can be useful in the treatment of childhood FI (40). For adults, regimens may vary from 1 to 2 L of PEG with electrolytes (38).
A review of 10 randomized controlled trials comparing lactulose to PEG showed higher weekly frequency for patients using PEG (41). There are also other osmotic laxatives such as oral magnesium citrate that has been used for proximal washout. A study of 10 patients reported that osmotic laxative is effective for patients with no evidence of bowel obstruction (29). Bekkali and colleagues (42), in their trial study, showed that enema and polyethylene glycol are equally effective for patients with rectal FI, and it should be the first line therapy (43). The operation is required in cases with evidence of obstruction or being refractory to medication therapy (44). In this case, successful therapy is focused on keeping the mechanical balance of the colon, to clear out FI. If there is a bowel obstruction, food and water intake should be ceased due to the fact that it can increase the intra-colonic pressure, which may develop a complication of fecal perforation. Once symptoms are relieved, it is necessary to receive maintenance therapy to avoid recurrence (45). In addition, a radiographic study may be necessary for monitoring the adequacy of treatment (46). A water-soluble contrast can be helpful for outlining the colon and fecal mass as well as ruling out other diseases without aggravating the condition when FI is present, however, whenever we want to use barium contrast we should be cautious (47).
3.1. Conclusion
In conclusion, physicians should be aware of severe constipation in patients who are abusers/dependent to opioids. High potency first generation antipsychotics (such as haloperidol and trifluoperazine) as well as second generation antipsychotics with low anticholinergic properties (such as risperidone) are preferred medications. Clozapine-induced constipation can lead to bowel obstruction due to FI so psychiatrists, general physicians, and radiologists, in particular, should be aware of the risk bowel obstruction in these cases. A patient with a history of schizophrenia who had been treated with clozapine presenting with abdominal pain and vomiting should raise immediate concern. Attention should be given to the aggravating concomitant factors that are worsening constipation.