1. Background
Sleep disorders are a group of mental disorders that play prominent roles in public health (1). It is estimated that approximately 30 to 45 percent of people in the world suffer from sleep problems (2), thereby leading to serious outcomes because a study shows that low-quality sleep is associated with various effects, including deficits in executive functions and the ability of the brain to design, organize, and paying close attention to activities (3), damages to the immune system and metabolism adjustment (4), creativity and memory (5), accidents and injuries (6), behavioral problems (7), and neuro-behavioral dysfunction (8), which can be caused by poor quality of sleep. Accordingly, conducting research into sleep is a basic need. On the other hand, insomnia is one of the most common sleep disorders and the results of a study revealed that the prevalence of insomnia is between 20 and 40 percent (9). It can be expressed that the prevalence of insomnia in various countries of the world is different but in general, it is estimated that 30 percent of people around the world experience insomnia at a stage in life. However, it is estimated that 10% of people around the world continuously and constantly suffer from insomnia (10).
It should be noted that emotional dysregulation is the main feature in 75 percent of mental disorders (11). The term ‘emotional regulation’ refers to internal processes as well as external processes that its function is processing, evaluation, and recognition of emotional responses (12). Reviewing the psychological literature showed that emotional regulation was a determining factor in health (13). In general, we can say that emotional dysregulation occurs in every psychiatric disorder (14). As for sleep, the results of a study indicated that emotions play important roles in sleep disorders (15). Most theories about the etiology of insomnia have referred to the role of emotion regulation as one of the main causes of high arousal in patients with insomnia (16). For this reason, emotional dysregulation was considered another predictor variable of insomnia. Emotional regulation is one of the variables that correlates with repetitive negative thoughts and includes strategies that are adopted to display and intensify an extended range of emotions (17). A study indicates that repetitive negative thoughts are a major variable in many mental disorders, including sleep disorders (18). Researchers claimed that cognitive arousal resulted in insomnia more than physiological arousal and cognitive arousal can be manifested in the form of anxiety, rumination, intrusive thoughts, and difficulty controlling emotional thoughts (19). Another research also confirms this theory. For example, the results of this research demonstrated that people with low-quality sleep had more rumination and intrusive thoughts compared to others (20).
Moreover, it seems that experiential avoidance, one of the constructs of acceptance and commitment theory, is another important variable whose role should be examined in insomnia. In the acceptance and commitment theory, one of the main causes of disorders is how a person communicates with thoughts, emotions, and behaviors (21). The third-generation behavioral theories believe that the presence of unpleasant cognitions alone cannot cause problems such as insomnia since it is one of the efforts to avoid such unpleasant subjective experiences that pose psychological problems. In fact, experiential avoidance is regarded as an important factor in the etiology and persistence of psychopathology. Experiential avoidance refers to the severely negative evaluating of emotions, unwanted feelings and thoughts and, unwillingness to experience these events and intentional attempts to control them (22).
In fact, experiential avoidance is a set of interdependent constructs, which include thought suppression, emotion suppression, and reevaluation (23). Further, the role of experiential avoidance has been confirmed in many psychiatric disorders (22). Despite sufficient evidence in favor of the relationship between emotional-physiological arousal and sleep disorder, some claim that this path is not certainly clear (24). In this study, two models have been investigated in two examples that can help clarify this path.
2. Objectives
The current study was done to investigate the mediating roles of repetitive negative thoughts in contribution to sleep quality and each of emotional dysregulation and experiential avoidance.
3. Materials and Methods
3.1. Participants and Procedure
In this descriptive and correlational study (a cross-sectional), two groups of samples were selected. The first group consisted of the patients suffered from chronic insomnia disorder (CID) who visited the Sleep Disorders Research center in Kermanshah for the cure in 2016 and their records were kept there. Also, the second group consisted of the employees at Kermanshah University of Medical Sciences. Furthermore, 120 and 200 samples were selected in the first and second group through simple random sampling, respectively (according to the statisticians, for structural equation modeling is required 15 people for each variable). It should be noted that none of the members of the second group suffered from insomnia. The selected patients have had almost a year of illness’s diagnosis of insomnia. They received the medicine. In addition, written informed consent was obtained from all participants before the study began and the inclusion criteria were the age range of 18 - 60 and to have junior school education at least. Moreover, the exclusion criteria were medical illness, substance dependency or abuse, Hypnotic drugs, and shift work. Then, the questionnaires were distributed among the participants. To this aim, the detailed descriptions of how to complete the questionnaires were presented by the researchers and the subjects were said to ask for more clarification in case of facing problems in completing the questionnaires. Moreover, the questionnaires were completed individually in the presence of the researchers. Finally, the questionnaires were collected and then analyzed. Then the data collected from 320 participants were analyzed using the AMOS-2 software and SPSS statistical software version 21.0, through path analysis and structural equation modeling.
3.2. Ethical Considerations
After obtaining an informed consent form for participating in the study and providing the necessary guarantees to the subjects ensuring them of the confidentiality of their information, the necessary data were assembled from each of the subjects, which would usually take 25 - 30 minutes.
This study was approved by the Medical Research and Ethical Committee of Kermanshah University of Medical Sciences, Kermanshah, Iran with registration No. Kums.REC.1395.230 at the date of June 22, 2016.
3.3. Measures
3.3.1. Pittsburgh Sleep Quality Index
This standard index, created by Buysse et al. in 1989, is a self-report questionnaire with 18 questions included under 7 subscales. The first subscale was linked with subjective sleep quality, specified by one question (question 9). The second one was correlated to delays in starting sleep, specified by two questions, i.e. the mean score of the second question and section ‘A’ of the fifth question. The third subscale was related to sleep duration, specified by one item (question 4). The fourth one dealt with one’s sleep efficiency. The fifth subscale was mentioned to sleep disorders and was specified by calculating the average scores of the fifth question. The sixth subscale was linked to using of sleeping medicine, specified by one question (question 6). The seventh one dealt with poor function, specified by two items (the average of the scores of the seventh and eighth questions), and the score of each question ranged from zero to three, with a maximum score of three for each question. The total of these seven subscales made up the total score of the instrument, ranging from zero to 21. The upper the score, the lower the sleep quality would be, and a score of more than six showed poor sleep quality (25). Furthermore, in the present study, the reliability of the instrument was examined that Cronbach’s alpha in total sample was 0.78, in clinical sample was 0.81 and in the non-clinical sample was 0.71.
3.3.2. Difficulties in Emotion Regulation Scale (DERS)
This 36-item scale comprised six subscales: Non-acceptance of emotional responses (NONACCEPT), difficulties engaging in goal-directed (GOALS), impulse control difficulties (IMPULSE), lack of emotional awareness (AWARE), limited access to emotion regulation strategies (STRATEGIES), and lack of emotional clarity (CLARITY). The questionnaire scoring method was as follows: Almost never = 1, sometimes = 2, about half the time = 3, most of the time = 4, almost always = 5.
The overall internal reliability of the scale was 0.93, which measured 0.85, 0.89, 0.86, 0.80, 0.88 and 0.84 for each of the above-mentioned subscales, respectively. Moreover, in a study performed by Alavi et al. overall internal reliability of the questionnaire was reported at 0.86. The higher one’s score on this scale, the lower his/her emotion regulation would be (26). In addition, the validity of the instrument was examined in the present study (α = 0.86).
3.3.3. Repetitive Negative Thinking Scale
This 31-item scale was developed by Mack et al. (2010) to assess the repetitive negative thoughts on a five-point Likert scale. The reported Cronbach’s alpha coefficient for this questionnaire measured 0.72-0.93. To calculate the predictive validity, the correlation between this instrument and Beck’s depression and anxiety questionnaire was used and the correlation coefficients were measured 0.42 and 0.38, respectively (19). The reliability of the Persian version of this instrument was reported at 0.89 (27).
3.3.4. Experiential Avoidance Questionnaire
This 32-item instrument was developed by Hayes et al. on a seven-point Likert scale; for the option never = 1; very low score = 2; low score = 3; sometimes = 4; great = 5; often = 6; and always = 7. Moreover, the former versions of the scale used to consist of 16 and nine items, but the latest version, which was used in the current study, has 10 questions on a seven-point Likert scale. In this research, a single-factor structure was obtained for this scale, and the reported Cronbach’s alpha measured 0.84 (28). Additionally, the reliability of the questionnaire was evaluated in Iran (α = 0.82). To check the validity of the scale, the Beck’s depression and anxiety questionnaire and emotional dysregulation scale were employed, and the correlation coefficients measured 0.44, 0.59, and 0.59, respectively. Furthermore, the results of factor analysis showed that the factors had appropriate weights (29).
4. Results
Detailed information about the nature of the samples is shown in Table 1.
| Variables | Clinical Sample | Non-Clinical Sample | P Value |
|---|---|---|---|
| Gender | 0.003 | ||
| Female | 77 (64.2) | 94 (47) | |
| Male | 43 (35.8) | 106 (53) | |
| Education | 0.001 | ||
| Junior school | 6 (5) | 18 (9) | |
| High school diploma | 56 (46.7) | 35 (17.5) | |
| University degree | 58 (48.3) | 147 (73.5) | |
| Marital status | 0.001 | ||
| Married | 90 (75) | 102 (51) | |
| Single | 30 (25) | 98 (49) | |
| Smoking | 0.14 | ||
| Yes | 14 (11.7) | 15 (7.5) | |
| No | 106 (88.33) | 185 (92.5) | |
| Age, y | 39.73 ± 9.58 | 37.78 ± 11.58 | 0.10 |
| Weight, kg | 65.98 ± 12.20 | 69.44 ± 17.44 | 0.06 |
Detailed Information About the Nature of the Samplesa
First, the simple correlation coefficients obtained from the Pearson product-moment correlation coefficient were examined in separate groups. As for the clinical samples, the results indicated that there was a correlation of 0.60 between the emotional dysregulation and sleep quality. In addition, the results revealed that there was a correlation of 0.36 between experiential avoidance and sleep quality, and the correlation between repetitive negative thoughts and sleep quality was measured 0.60. As for the group of employees, the results demonstrated that there was a correlation of 0.34 between the emotional dysregulation and sleep quality. In addition, the results showed that there was a correlation of 0.36 between experiential avoidance and sleep quality, and the correlation between repetitive negative thoughts and sleep quality measured 0.52 (P < 0.001). All these correlations were positive, i.e., the higher the levels of emotional dysregulation, experiential avoidance and repetitive negative thoughts, there would be greater sleep disorders, and vice versa. As shown in Table 2, the intensity of the correlation between emotional dysregulation and sleep quality in the clinical samples was higher (Z = 2.9, P = 0.001).
| Variables | Clinical Sample | Non-Clinical Sample | Fisher r-to-z | |||
|---|---|---|---|---|---|---|
| Mean ± SD | ra | Mean ± SD | r | Zb | P Value | |
| Sleep quality | 8 ± 4.78 | 1 | 4.36 ± 2.33 | 1 | - | - |
| Emotional dysregulation | 93.04 ± 21.05 | 0.60 | 88.39 ± 30.56 | 0.34 | 2.9 | 0.001 |
| Experiential avoidance | 36.68 ± 12.65 | 0.36 | 33.55 ± 11.46 | 0.36 | 0 | 0.5 |
| Repetitive negative thinking | 87.15 ± 29.97 | 0.60 | 84.70 ± 20.63 | 0.52 | 1 | 0.16 |
The Means and Correlation Coefficients with Sleep Quality in Both Groups
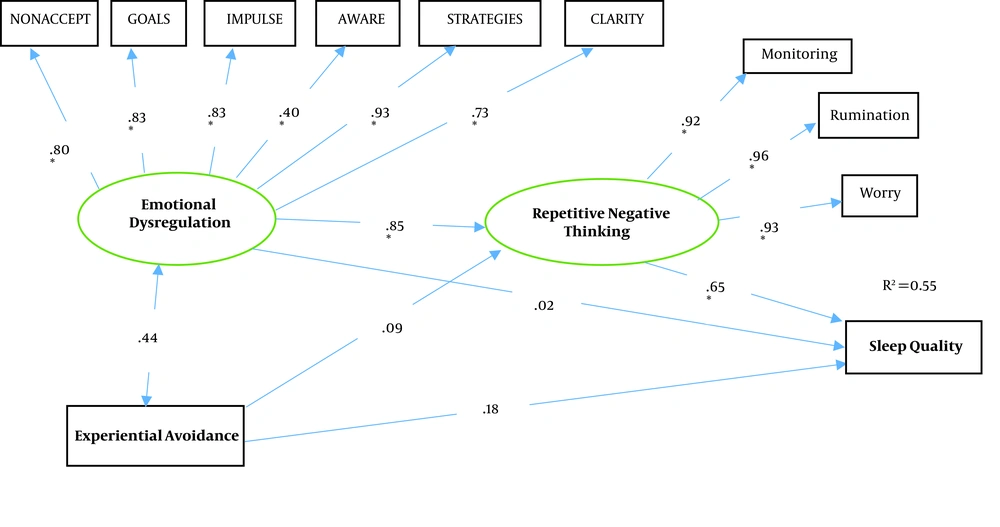
To investigate the mediating role of repetitive negative thoughts in contribution to sleep quality and each of emotional dysregulation and experiential avoidance in separate groups, the path analysis and structural equation modeling were utilized. The results showed that the proposed model had an acceptable fit in the clinical samples (χ2/df = 2.59, df = 129, CFI = 0.90, TLI = 0.91, RMSEA = 0.081, akaike information criterion (AIC) = 102.25). The proposed model for clinical samples is presented in Figure 1.
The research model in the clinical samples. NONACCEPT, non acceptance of emotional responses; GOALS, difficulties engaging in goal-directed; IMPULSE, impulse control difficulties; AWARE, lack of emotional awareness; STRATEGIES, limited access to emotion regulation strategies; CLARITY, lack of emotional clarity; * = path coefficients are statistically significant.
The results of the analysis revealed that emotional dysregulation, experiential avoidance, and repetitive negative thoughts together could predict 55% of the changes of sleep quality in the clinical samples. Additionally, in the model presented for the clinical samples, the standard coefficient of the emotional dysregulation path to repetitive negative thoughts was measured 0.85, and the repetitive negative thoughts path to sleep quality was 0.65. However, the results revealed that the experiential avoidance did not have direct effects on repetitive negative thoughts. Moreover, it was demonstrated that each of emotional dysregulation and experiential avoidance did not directly affect the sleep quality among patients suffered from insomnia. The results also indicated that the standard coefficient of the experiential avoidance path to sleep quality was not significant through repetitive negative thoughts among clinical samples, while the standard coefficient of emotional dysregulation path to sleep quality was significant through repetitive negative thoughts (β = 0.55). Therefore, it can be indicated that emotional dysregulation leads to reduced sleep quality among clinical samples suffering from insomnia when the level of repetitive negative thoughts is high.
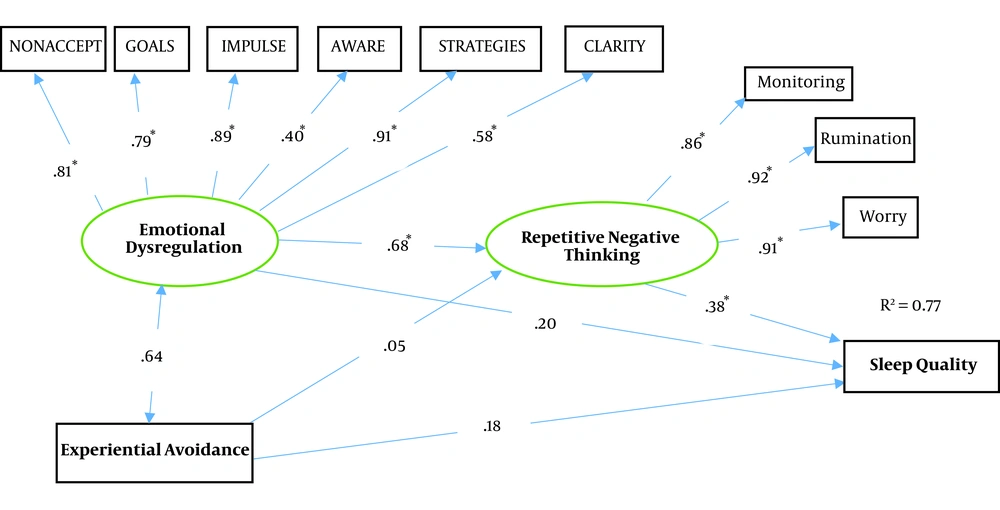
As for the non-clinical samples, the results showed that the proposed model had an acceptable fit among non-clinical samples (χ2/df = 1.84, df = 129, CFI = 0.94, TLI = 0.95, RMSEA = 0.039, AIC = 82.02). The proposed model for non-clinical subjects is presented in Figure 2.
The results of the analysis revealed that emotional dysregulation, experiential avoidance, and repetitive negative thoughts together could predict 77% of the changes of sleep quality in the non-clinical samples. These results also demonstrated that repetitive thoughts were directly affected by emotional dysregulation (β = 0.68), and repetitive negative thoughts had direct effects on sleep quality (β = 0.38). However, other paths were not significant. The standard coefficient of the path between emotional dysregulation and sleep quality was significant through repetitive thoughts (β = 0.26). Accordingly, it can be claimed that emotional dysregulation leads to low-quality sleep when the level of repetitive thoughts is high. In fact, the results of the study revealed that repetitive negative thoughts played a mediating role in the relationship between emotion regulation and experiential avoidance. The summary of the results of path analysis (direct effects) for the proposed models of the research is shown in Table 3.
Summary of the Results of Path Analysis for the Proposed Models of the Research (Direct Effects)
The summary of the results of path analysis (indirect effects) for the proposed models of the research is shown in Table 4.
Summary of the Results of Path Analysis for the Proposed Models of the Research (Indirect Effects)
5. Discussion
The results of the present study demonstrated that emotional dysregulation and sleep quality correlated in both samples, but the intensity of this relationship in patients with insomnia disorders was more noticeable. Accordingly, it can be concluded that emotional dysregulation leads to reduced sleep quality. In a longitudinal study (30), the relationship between emotional dysregulation and sleep quality was addressed and the results indicated that emotional dysregulation correlated with the onset and maintenance of insomnia. In addition, it was concluded that emotional dysregulation could predict the possibility of insomnia in the future. However, the effect size was reported to be very low. The results of another study showed that there was a negative relationship between emotional dysregulation and sleep quality (31). People with emotional dysregulation always try to monitor their behavior and since the monitoring process requires energy, attention, and cognitive engagement (32), it can result in cognitive arousal and reduced sleep quality. The results of the present study revealed that emotional dysregulation did not have direct effects on sleep quality in both samples.
In models provided by Harvey (33) and Espie (34) it has been emphasized that patients with insomnia disorders have emotional dysregulation, but the mechanisms of the effects of emotional dysregulation on sleep have not been clearly expressed. However, the results of the present study demonstrated that emotional dysregulation did not have direct effects on sleep quality in both samples. Hence, it seems that the effects of emotional dysregulation on the quality of sleep are not direct because the results of the present study revealed that emotional dysregulation affected sleep quality through repetitive negative thoughts.
Moreover, the results of the present study indicated that experiential avoidance correlated with sleep quality. In other words, a rise in experiential avoidance leads to reduced sleep quality in people with and without insomnia. The results of the present study in another section showed that experiential avoidance did not have direct effects on sleep quality.
In a study conducted on a sample of 327 patients with insomnia by Li, the relationship between experiential avoidance and sleep quality was addressed and the results showed that experiential avoidance correlated with sleep quality and experiential avoidance could predict sleep quality. Furthermore, it was shown that the direct effect of experiential avoidance on sleep quality was measured 0.19 (35). The results of the present study indicated that the correlation between experiential avoidance and sleep quality exceeded this value in both samples (0.36).
From the perspective of acceptance and commitment therapy, the experiential avoidance results in efforts at suppressing feelings, thoughts, and other inner experiences. In addition, it is believed that lack of mental flexibility lays the groundwork for emotional disorders (36), while another research indicates that there is a relationship between emotional disorders and sleep disorders (37). On the other hand, avoidance of inner thoughts and experiences increases physiological arousal and negative emotions (38), thereby leading to reduced sleep quality.
In addition, the results of the present study revealed that experiential avoidance did not have direct effects on sleep quality in both samples. Thus the repetitive negative thoughts were considered to find the mediator in this relationship. The results showed that repetitive negative thoughts did not act as a mediator in the relationship between experiential avoidance and sleep quality. Therefore, it is recommended that further studies should be conducted to find a suitable mediator in this relationship.
In addition, the results of our study revealed that repetitive negative thoughts and sleep quality strongly correlated in both samples and it was found that repetitive negative thoughts had direct effects on sleep quality. Hence, it can be concluded that with the increase of repetitive negative thoughts, the sleep quality is reduced. The results of a study indicated that rumination affected sleep quality (39). On the other hand, the results of another study on a sample of 242 patients with insomnia revealed that anxiety and rumination played roles in the quality of sleep of patients with insomnia (40).
In fact, these repetitive negative thoughts result in cognitive, emotional, and physiological arousal. However, some researchers (41) believe that repetitive negative thoughts have a strong correlation with physiological arousal. In general, the results of our study showed that the repetitive negative thoughts acted as a mediator in the relationship between emotional dysregulation and sleep quality. Similarly, Slavish and Graham-Engeland showed that sleep quality, depression, and anxiety correlated through rumination (42). In a study performed about the relationship between sleep quality and factors such as cognitive processes, arousal and emotional dysfunction, it was shown that the role of rumination in this relationship was more noticeable. The results also indicated that rumination acted as a response style for emotion regulation, while cognitive processes lead to insomnia when one’s approach is rumination for emotional regulation (43).
5.1. Limitations
Since the present study was conducted among employees at Kermanshah University of Medical Sciences and patients with insomnia who visited the Sleep Disorders Research Center under the supervision of Farabi Hospital based in Kermanshah for cure in 2016, extreme caution should be exercised in generalizing the results to other communities due to the different social and cultural conditions. We suggest that these variables be studied in other populations and be examined in longitudinal studies.
5.2. Conclusions
Given the results of the present study, it can be concluded that emotional dysregulation leads to sleep disturbances when there are repetitive negative thoughts. Accordingly, the role and importance of repetitive negative thoughts should be taken into consideration by therapists to treat insomnia.