1. Background
The birth of an infant requiring intensive care is a stressful and painful experience for the parents. Uncertainty about survival, later consequences, the duration of hospitalization, and caring for the infant at home are among concerns of these parents. Such concerns make parents feel confused, helpless, frightened, anxious, and depressed and may even cause posttraumatic stress disorder (PTSD), especially in mothers (1, 2).
Furthermore, PTSD is a very common, chronic, and debilitating psychiatric disorder. Based on the Diagnostic and statistical manual of mental disorders-fifth edition (DSM-5), PTSD is a stress- and trauma-related disorder that can develop after a harmful event and is characterized by four clusters of symptoms, including harassment, avoidance, negative changes in cognition and mood, and prominent changes in excitability and reactivity. This disorder is often accompanied by major depression, other anxiety disorders, drug abuse, and poor quality of life (3-5).
Facing the above-mentioned stresses prompts parents to use coping strategies. If the health system fails to help them cope with their new conditions, they might resort to ineffective coping strategies, such as drug abuse, smoking, illegal acts, avoiding work and activity, violence, and aggression towards the medical personnel (6). Such conditions may exert negative effects on mothers’ personal and social quality of life, reduce their ability to provide their infants with the required care, and ultimately lead to further psychological problems (7-9). Globally, research on maternal emotional responses to childbirth is increasing. The symptoms of anxiety and depression have been widely studied and have been shown to affect the relationship between the mother and the infant yet studies about PTSD and its effect are very young (10).
Various pharmacological and non-pharmacological strategies have been proposed for the treatment of PTSD. A combination of pharmacotherapy and non-pharmacological interventions, such as counseling and training, has been found more effective than drug therapy alone in the treatment of PTSD (11).
Counseling can be offered with different approaches, including the cognitive-behavioral approach. Cognitive-behavioral therapy involves the use of cognitive-behavioral strategies to provide group counseling through training and group discussions. This form of therapy aims mainly at helping group members identify and experience their own feelings, understand the ways their beliefs and assumptions affect their feelings and behaviors, and experience alternative behaviors (12-14). This method helps mothers find ways to cope with stress (15) and feel better about themselves and their children (16, 17). Group counseling is more effective than individual counseling in situations of crisis, in which psychological pressure leads to feelings of helplessness, inadequacy, fear, defeat, and severe anguish (18).
Previous studies have shown that most mothers need the support of the medical team for meeting their needs. Therefore, care providers should establish a close relationship with mothers, in order to help them identify and satisfy their needs. Midwives are a group of health care workers, who can best establish such a relationship by providing women, their families, and the community with the required counseling and health education (19).
2. Objectives
Considering all the mentioned points and the importance of paying attention to mothers with special conditions, this study evaluated the effects of cognitive-behavioral counseling on PTSD in mothers with infants hospitalized in neonatal intensive care units (NICU).
3. Materials and Methods
3.1. Design
The present randomized clinical trial was conducted in parallel on 90 eligible females attending the Kowsar Teaching Hospital (Qazvin, Iran), during year 2016.
3.2. Sample
Based on the PTSD scores obtained in previous studies (1, 20, 21) and the standard deviations before (3.65) and after (2.71) the intervention and considering a score difference (reduced PTSD score) of 1.96 for the comparison of two mean values, the sample size was calculated as 42 individuals per group. The number of participants in each group was increased to 45 to allow for a 10% potential withdrawal. The participants were selected from eligible women attending the Kowsar Hospital in Qazvin. Iranian women with a preterm (born before 37 weeks of gestation) and/or low-birth-weight infant (< 2500 g) hospitalized at the NICU for at least one month were included, if they were willing to participate, had a high school diploma or higher education, and had PTSD (confirmed through Beck’s PTSD symptom scale). Women, who had experienced an adverse life event, e.g. the death of a loved one, in the past six months, received anxiolytics or antidepressants, or had a history of giving birth to an infant with special diseases or severe abnormalities, were not included.
3.3. Data and Measures
A checklist including socio-demographic characteristics and the items of the PTSD symptom scale was used to collect data. The PTSD symptom scale consists of 17 items in three domains, including re-experiencing, avoidance, and arousal symptoms (four, seven, and six items, respectively). All items were scored based on a Likert scale from zero (not at all) to three (five times or more per week/a lot). The diagnosis of PTSD was confirmed if a person indicated the presence of at least one re-experiencing symptom, three avoidance symptoms, and two arousal symptoms (1). The PTSD symptom scale is a standard scale, whose validity and reliability have been widely assessed. In Iran, it was assessed by Mirzamani et al. and according to their report, the concurrent validity and test-retest reliability was 0.62 (P < 0.001; r = 0.62) and 0.76 (P < 0.001; k = 0.76), respectively (1).
3.4. Procedures
This study was approved by the Ethics Committee of Alborz University of Medical Sciences (Karaj, Iran). The ethical code number was 1395.13. The study was also registered in the Iranian Registry of Clinical Trials (code: IRCT2016051427728N1). Convenience sampling was used to select the participants. For this purpose, the researcher visited the NICU, identified eligible mothers, provided them with the objectives of the study, and asked them to sign an informed consent form, if they were willing to participate. The selected females were then assigned to the intervention (PTSD counseling + routine care counseling) and control (routine care counseling + educational package containing the topics discussed in the PTSD counseling sessions) groups. Eight (twice weekly) sessions of routine counseling (routine infant care) were held for both groups and it included:
Session 1: Information about the hospitalized infant, such as the type of disease and the diagnostic and therapy methods used.
Session 2: Information about the disease symptoms and consequences.
Session 3: Obtaining knowledge and skills about nutrition.
Session 4: Obtaining knowledge and skills about moving and positioning.
Session 5: Obtaining knowledge and skills about hygiene and infection control.
Session 6: Obtaining knowledge and skills about temperature and how to clothe the infant.
Session 7: Obtaining knowledge and skills about the infant’s behavior.
Session 8: Obtaining knowledge and skills on how to interact with the infant.
This package was prepared by Kowsar Teaching Hospital and used for all patients.
The package for PTSD counseling was prepared by an expert panel, including a psychologist, psychiatrist with a cognitive-behavioral approach. The topics discussed in the intervention group and in the package for the control group were as follows:
Session 1: Introduction, discussing group rules and objectives of group therapy, building relationships between mothers, and getting feedback.
Session 2: Asking mothers to discuss the psychological aspects of their feelings and thoughts about the hospitalization of their infants while observing the limitations of a support group, psychological adjustment and emotional release within a supportive environment, and trying to combine the feelings of all group members.
Session 3: Discussing the definition and signs of stress and explaining stress relief techniques for eliminating the signs of stirred emotions.
Session 4: Evaluating the effects of cognition and thoughts on stress responses, advising the participants on how to identify their negative self-talks, emphasizing the significance of coping skills, such as stress management strategies, and discussing how different individuals deal with various stressful events.
Session 5: Discussing stressful self-talk, helping the participants use self-talk as an effective coping strategy, and reviewing stress relief exercises discussed in previous sessions.
Session 6: Focusing on problem-solving skills and asking each mother to provide a description of her problem.
Session 7: Discussing and evaluating alternative solutions and choosing the best one.
Session 8: Examining the efficacy of each solution and readjusting them when necessary.
The duration of the sessions ranged between 40 and 60 minutes in both groups. For ethical considerations, at the end of the last session, the control group also received the educational package, containing topics discussed in the counseling sessions of the intervention group.
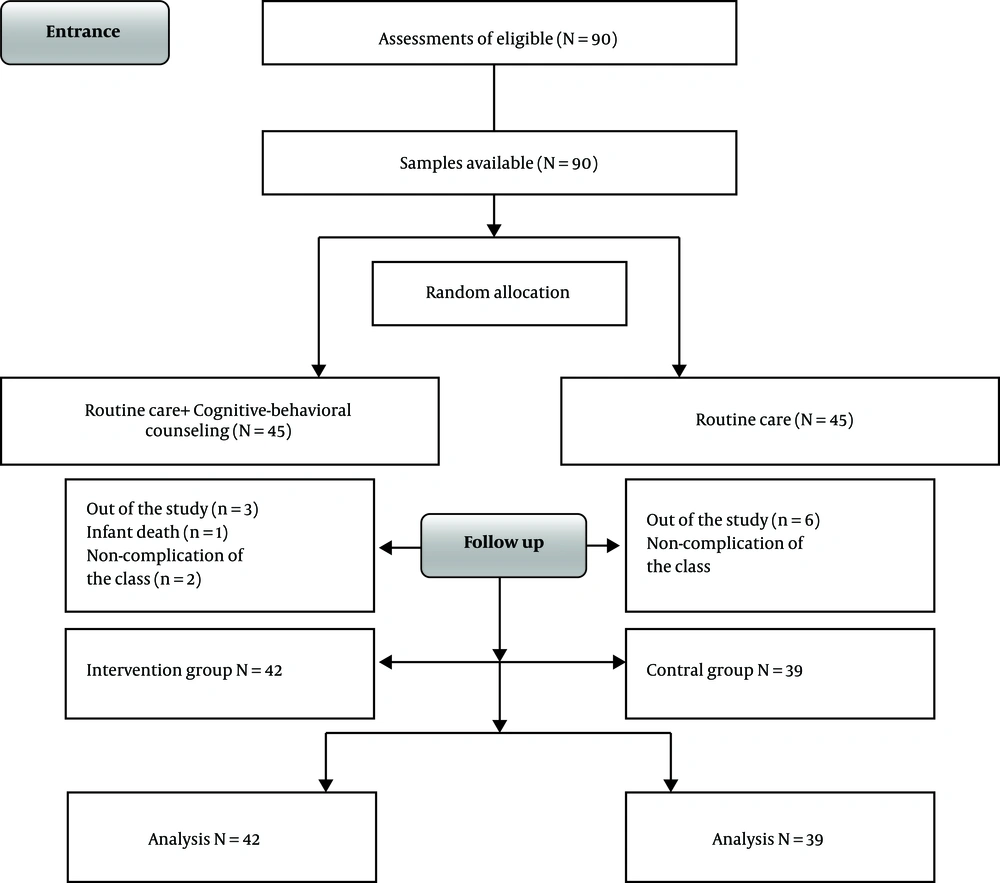
The questionnaire was completed by the mothers before the intervention. The obtained scores were considered as both the baseline scores and a standard for ensuring that they met the inclusion criteria. The questionnaire was again completed immediately and three weeks after the intervention (to examine the persistence of the effects of the intervention). Overall, three women from the intervention group and six from the control group withdrew from the study. These women were all excluded as they did not attend all sessions (in one case, however, the participant’s infant died). The total number of the participants was, hence, 81 (Figure 1).
Data analysis was performed using the SPSS 19.0 software (SPSS Inc., Chicago, IL, USA). Independent t, Mann-Whitney, and Friedman test, along with the generalized estimating equation (GEE), were applied to analyze the data.
4. Results
Most of the 81 mothers with infants hospitalized at the NICU were housewives and 18 to 24 years old. The normal distribution of the variables was examined using the Kolmogorov-Smirnov test. According to the obtained results, the two groups matched in terms of the participants’ mean age, education, occupation, and income (Table 1). Moreover, the two groups had no significant differences in the mean baseline PTSD scores (P = 0.385). The GEE, however, showed that the two groups were significantly different in terms of their mean PTSD scores after the intervention. Moreover, the PTSD scores of the intervention group immediately and three weeks after the intervention were significantly lower than their baseline score (Table 2). According to the Friedman test, the intervention had a significant effect throughout the three stages of the study. Furthermore, the mean PTSD score immediately after the intervention was significantly lower than the baseline scores in both groups. Nonetheless, three weeks after the intervention, this score decreased in the intervention group yet increased in the control group (Table 3).
| Variable | Group | P Value | |
|---|---|---|---|
| Intervention Groupb | Control Groupc | ||
| Age | 0.2 | ||
| 24 - 18 | 22 (52.4) | 22 (56.4) | |
| 35 - 25 | 20 (47.6) | 17 (43.6) | |
| Mean ± SD | 23.83 ± 3.8 | 22.87 ± 3.7 | |
| Level of education | 0.528 | ||
| Bachelor’s degree | 23 (54.7) | 25 (64.1) | |
| Master’s degree or higher | 19 (45.3) | 14 (35.9) | |
| Mean rank | 42.43 | 39.46 | |
| Employment status | 0.728 | ||
| Housewife | 25 (59.5) | 25 (64.1) | |
| Employee | 17 (40.5) | 14 (35.9) | |
| Mean rank | 41.76 | 40.18 | |
| Income | 0.731 | ||
| Mean rank | 41.57 | 40.38 | |
aValues are expressed as F (%).
bIntervention group (PTSD counseling + routine care counseling).
cControl group (routine neonatal care).
| Variable | Mean ± SD | Generalized Estimating Equation | ||
|---|---|---|---|---|
| Before the Intervention | Immediately After the Intervention | Three Weeks After the Intervention | ||
| Intervention group | 8.095 ± 5.202 | 4.547 ± 2.297 | 5.000 ± 2.447 | P = 0.000 |
| Control group | 6.820 ± 4.297 | 6.564 ± 4.290 | 14.205 ± 4.856 | |
| Variable | Mean ± SD | Friedman Test | ||
|---|---|---|---|---|
| Before the Intervention | Immediately After the Intervention | Three Weeks After the Intervention | ||
| Intervention group | 8.095 ± 5.202 | 4.547 ± 2.297 | 5.000 ± 2.447 | P = 0.000 |
| Control group | 6.820 ± 4.297 | 6.564 ± 4.290 | 14.205 ± 4.856 | P = 0.033 |
5. Discussion
Post-traumatic stress disorder is a very common, chronic, and debilitating psychiatric disorder (3-5). The current findings showed that cognitive-behavioral counseling positively affected PTSD symptoms in mothers with special conditions. The comparison of the two groups in terms of their mean PTSD scores immediately and three weeks after the intervention indicated a significant reduction in the intervention group compared to the controls on both occasions. Moreover, the mean PTSD scores in the intervention group were significantly lower in both post-intervention stages, compared to the baseline. In the control group, however, the mean score increased three weeks after the intervention. This highlights the important role of counsellors. Likewise, Taghizadeh et al. found counseling to be effective in reducing the symptoms of PTSD and identified the presence of a counsellor, not leaving the mothers to themselves after the end of the counseling, the availability of the counsellor whenever required, and special counseling content, as the reasons for this positive effect (22).
Owing to their high levels of anxiety and depression, patients with PTSD are incapable of regulating their basic emotions. Cognitive-behavioral counseling reduces PTSD by teaching techniques for controlling the physiological components of the disorder and by helping the patients modify their misunderstandings of their surrounding events (8). Kazemi reported that teaching mindfulness-based cognitive strategies was effective in reducing the general symptoms of PTSD and its related variables, including disturbing thoughts and arousal avoidance responses. It could also alleviate the symptoms of depression, anxiety, and stress, as well as ineffective attitudes and beliefs in negative automatic thoughts, in people with PTSD (23).
Cognitive-behavioral therapy assumes that anxious people are more prone to perceiving threats and show debilitating and avoidance coping responses rather than constructive behaviors and proper coping responses. This will, in turn, lead to the persistence of anxiety and a progression towards PTSD and anxiety (24). As a result, regular daily observation of the behaviors of people, who respond differently to the same situation, and form judgments, evaluations, expectations, and perceptions (which dominate the person’s awareness) helps change their behavior and attitude while dealing with stressful situations. Cognitive-behavioral therapy enables individuals to carefully adopt the most reasonable and adaptive interpretation and behave in a way that is compatible with their new perspective (25).
Midwives are a group of healthcare professionals with a major role in providing women, their families, and the community with counseling and health education. They, hence, play a key role in the mentioned interventions (19).
The strengths of this study include matching the two groups in terms of their baseline PTSD scores and reducing the confounding factors as much as possible. While the special conditions of the participating mothers might have affected the way they responded to the questions, this factor could not be controlled by the researcher and remained as a limitation of the study, despite the adopted efforts (by defining relevant inclusion and exclusion criteria).
5.1. Conclusion
This study confirmed the effectiveness of cognitive-behavioral counseling in decreasing the degree of PTSD in mothers with infants hospitalized at NICUs. Considering the important role of healthcare professionals, particularly midwives in keeping new mothers company, facilitating a conducive counseling environment appears to help reduce PTSD and anxiety in mothers with special conditions. Such efforts can also improve these women’s quality of life and provide them with the skills required for taking care of their infant at home.