1. Context
The high prevalence of trauma and disaster exposure, as well as their subsequent complications, for both survivors and community as a whole highlights the need for the secondary prevention of (post-traumatic stress disorder) PTSD (1).
Traumatic events have a different distribution of incidence in the world. However, in several geographical regions, specific populations are frequently exposed to trauma experiences such as combats, organized violence, terrorism, and natural disasters (2, 3). Studies on PTSD suggest different trajectories in different populations due to the various types of traumatic events, living situations, psychological agents, and methodological differences (4-6). According to the literature, the prevalence of possible traumatic experiences is greater in the USA than in Europe (7). Indeed, while the PTSD prevalence in the USA has been reported about 10% for women and 5% for men (7, 8), it is between 2.0 and 3.5% in the European population (9, 10). It is worth mentioning that PTSD is related to various mental and physical distress, as well as high economic burden (9, 10).
Iran was unfortunately invaded for eight years, during 1980 - 1988, by neighboring countries. Besides, it was exposed to several natural disasters such as the Bam earthquake in 2003 that resulted in more than 40,000 deaths. Therefore, it would be of great importance to study various aspects of PTSD in this country (11, 12), as adverse mental health effects in Iran are mostly noted in times of war and natural disasters along with PTSD as the main outcome (13).
2. Evidence Acquisition
2.1. Data and Source Search Strategy
The purpose of the study was to carry out a meta-analysis of published studies reporting the prevalence of PTSD in the Iranian population from 2000 to 2015. This study was approved by the joint council of the centers for neuroscience study in 2015. Indeed, it was reviewed by the Research Committee of Baqiyatallah University (No., 421) in 2015 and all protocols were approved.
We estimated the prevalence of PTSD in the Iranian population with a comprehensive systematic review and a meta-analysis of the literature and evidence, followed by integrating the data and analyzing the findings. We included all published studies evaluating the prevalence of PTSD in the Iran population, irrespective of their publication status or language.
2.2. Search Strategy
The purpose of the study was to determine the PTSD prevalence in the population at risk based on the obtained data from Iranian patients’ society. Therefore, we observed both national and international databases. In October 2015, the following libraries and electronic databases were searched for potentially relevant studies: PubMed, MEDLINE via OVID, Wiley, EMBASE via OVID, ProQuest dissertations and thesis, ISI Web of knowledge, Scopus, Magiran, SID, Google Scholar, and Noormags. Notably, the terminologies used to identify these articles included: PTSD, stress disorder, post-traumatic, posttraumatic neuroses, chronic post-traumatic stress disorder, delayed-onset post-traumatic stress disorder, acute post-traumatic stress disorder, post-traumatic stress disorders, Iran. Besides, we used a suitable combination of terminologies as mentioned above for searching. We also manually checked the references of all included studies to recognize any new study.
2.3. Types of Outcome Measures
We labeled PTSD diagnosed patients according to the standard questionnaires and interviews (diagnostic and statistical manual of mental disorders (DSM-IV), Mississippi scale, PTSD symptom scale (PSS-I), posttraumatic stress disorder checklist (PCL), questionnaires, and interviews for PTSD based on various criteria) implemented by clinicians or trained interviewers and individuals in these studies to recognize PTSD.
2.4. Inclusion Criteria
All patients exposed to horrifying and traumatic events such as earthquakes, wars, childbirth, job, and others were included.
Notably, articles were published from 2000 to 2015. The outcome was the point prevalence of PTSD defined according to the standard tools. All of the contributors were Iranian people and had PTSD following natural or unnatural events taking place in Iran.
2.5. Exclusion Criteria
Studies with < 25 participants were excluded because the risk of recruitment bias was high.
2.6. Selection of Studies
Two reviewers independently assessed the titles and abstracts of all articles found by the searching strategy outlined above for inclusion based on predefined inclusion and exclusion criteria. Disagreements were resolved through discussion. If it was not helpful, a third review author was addressed in order to handle very disagreements.
2.7. Data Extraction
Two reviewers independently extracted data via a tested extraction sheet and disagreements were resolved through a joint meeting with a third reviewer.
Information was categorized regarding the study characteristics (year of publication, place of the study, study method quality), participants’ characteristics, the cause of PTSD, accession percentage, diagnosis tool, age range, and study population.
2.8. Statistical Analysis
Meta-analysis was performed using “metaprop” command in STATA 11 software. This command calculates the pooled estimate after arcsine stabilizes the estimations. According to the existence of heterogeneity between studies, data were pooled using a fixed or random effects model. The heterogeneity of studies was assessed by the Cochran Q statistic. We planned to test the statistical heterogeneity with the Q test (χ2, I2, and Tau-squared statistics). The findings were considered heterogeneous if the P value was less than 0.1. Moreover, I2 was utilized to provide a model of the degree of inconsistency between the results of the studies. A value of 0% indicated no observed heterogeneity, whereas larger values showed increasing heterogeneity.
3. Results
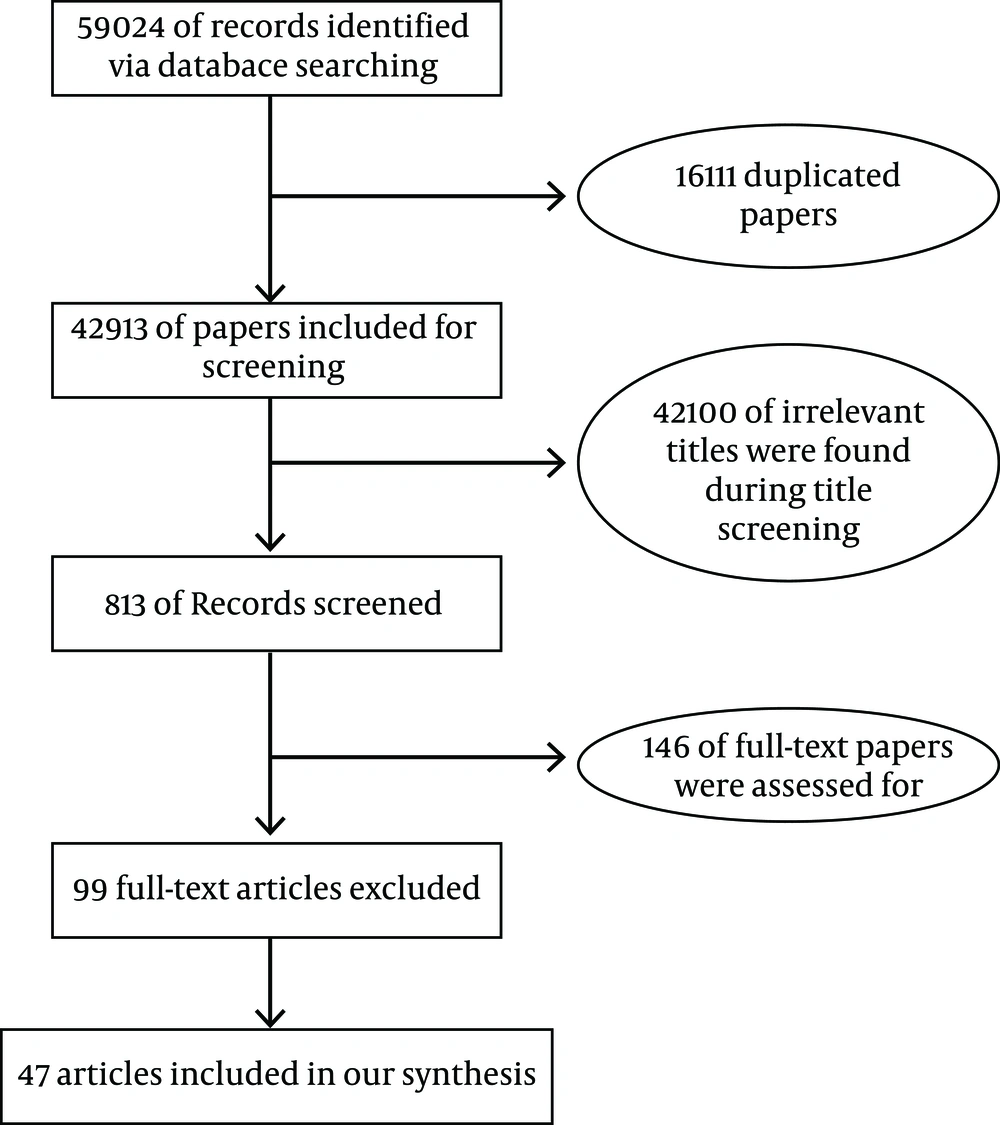
Our initial search retrieved 59024 studies of PTSD following traumatic events and disasters, which had been published from 2000 to 2015 (Figure 1). However, 16111 papers were eliminated because of duplication among databases. Then, 42913 studies were included in the primary screening.
Upon screening the titles and abstracts, 186 studies were identified for full-text reviewing.
Finally, we scrutinized the total number of 186 full texts. In the end, after applying the inclusion/exclusion criteria, 47 studies were selected (Table 1).
| First Author (Ref.) | Year | Year of Event | Duration of Identification | Total Sample Size | Male Sample Size | Female Sample Size | Prevalence | Primary/Secondary PTSD | Natural/Technical PTSD | Age Range | Study Population | PTSD Cause | Tools |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Firouzkouhi Moghadam (14) | 2015 | - | 6 to 24 weeks after delivery | 400 | 400 | 0.32 | P | N | Women with childbirth | Childbirth | PSS-I | ||
| Naderi (15) | 2012 | 2009-2010 | - | 256 | 0.2 | S | N | 29 - 75 | Parents of children with cancer | Disease | PTSD standard questionnaire according To DSM-IV | ||
| Sadeghi-Bazargani (16) | 2011 | 2009-2010 | 3.5 after event | 53 | 0.31 | P | N | 16 - 65 | Burn patients | Burn | PCL-DSM-IV-TR | ||
| Khajeh Mougahi (17) | 2008 | 2008 | 3 months after bombing | 62 | 42 | 20 | 0.63 | P | T | 4 - 6 | Children near bombing place | Explosion | Questionnaire for people under 15 years based on DSM-IV |
| Aminizadeh (18) | 2014 | 2011 | - | 240 | 171 | 79 | 0.97 | P | N | Emergency staff | Job | Mississippi scale | |
| Ghorbani (19) | 2014 | 2011 | 2 months after childbirth | 328 | 164 | 164 | 0.03 | P | N | 28.2 | Woman with preterm and term pregnancy | childbirth | DSM-VI |
| Shafiee Kamalabadi (20) | 2015 | 1980 - 1988 | 26 years after the war | 172 | 172 | 0.39 | P | N | Veterans | War | Mississippi scale | ||
| Kharamin (21) | 2013 | 2011 - 2012 | - | 70 | 70 | 0.91 | P | N | 7 - 40 | Victims of rape | Rape | PTSD checklist-clinical interview | |
| Farhoudian (22) | 2007 | 2004 | 8 months after the earthquake | 786 | 0.52 | P | N | 15 - 75 | Earthquake survivors | Earthquake | CIDI | ||
| Donyavi (23) | 2008 | 2005 | - | 355 | 335 | 0.15 | P | N | 20.68 | Army staff in Tehran | Explosion and Accident | DSM-IV-TR criteria by psychiatrists | |
| Modares (24) | 2011 | 2008 | 6 to 8 weeks after childbirth | 400 | 400 | 0.38 | P | N | 25 - 30 | Pregnant women | Childbirth | PSS-1-DSM-IV | |
| Karami (25) | 2008 | 2004 | 16 days after event | 100 | 55 | 45 | 0.22 | P | N | 14 - 32 | Earthquake Survivors | Earthquake | Interview based on questionnaire |
| Narimani (26) | 2010 | 2008 | - | 100 | 18 | 82 | 0.14 | P | N | Emergency staff | Job | Mississippi scale | |
| Narimani (26) | 2010 | 2008 | - | 100 | 90 | 10 | 0.08 | P | N | Firefighter staff | Job | Mississippi scale | |
| Khodadadi (27) | 2015 | 2010 | 1 month after event | 89 | 0.023 | P | T | 18 - 65 | Victims of road accident | Accident | SRS-PTSD | ||
| Saberi (28) | 2009 | 2008 | - | 121 | 121 | 0.36 | P | N | Emergency staff | Job | PTSS-10-DSM-IV, IES-I5-DSM-IV | ||
| Haji Maghsoudi (29) | 2006 | 2004 | A Few months after the earthquake | 259 | 0.6 | P | N | 17 - 18 | Earthquake Survivors | Earthquake | CPSS-DSM-IV | ||
| Vasegh Rahimparvar (30) | 2015 | 2012 - 2013 | 6 weeks after rape | 130 | 130 | 0.62 | P | N | 20 - 30 | Rape Victims | Rape | PSS-I | |
| Andy (31) | 2007 | 2005 | - | 80 | 80 | 0.47 | P | N | 20 - 40 | Burn patients | Burn | PSS-I -DSM-Iv | |
| Abedian (32) | 2014 | 2013 | - | 127 | 127 | 0.26 | P | N | Women with pre-eclampsia | Childbirth | Prenatal Posttraumatic Stress | ||
| Parvaresh (33) | 2007 | 2003 | 4 months after the earthquake | 243 | 175 | 68 | 0.53 | P | N | Under 15 | Bam students | Earthquake | PPQ |
| Nateghian (34) | 2008 | 1980 - 1988 | 20 years after the war | 84 | 42 | 42 | 0.4 | P | N | Men:40 - 49, women:30 - 39 | Spouses of veterans with PTSD | War | Mississippi scale |
| Fathi Ashtiani (35) | 2001 | 1980 - 1988 | 14 years after the war | 52 | 52 | 0.44 | P | N | Psychological war veterans | War | Davidian questionnaire based on semi-structured interviews | ||
| Mohaghegh Motlagh (36) | 2014 | 1980 - 1988 | 25 years after the war | 80 | 80 | 0.4 | P & s | N | Chemically injured veterans | War | PCL-M و IES-R | ||
| Mohaghegh Motlagh (36) | 2014 | 1980 - 1988 | 25 years after the war | 89 | 89 | 0.28 | P | N | No-chemically injured veterans | War | PCL-M و IES-R | ||
| Azampor Afshar (37) | 2010 | 1980 - 1988 | Yearlong | 100 | 100 | 0.99 | S | N | Spouses of veterans | War | Mississippi scale | ||
| Vizeh (38) | 2013 | - | 6 to 8 weeks after childbirth | 572 | 572 | 0.39 | P | N | 16 - 43 | Women with childbirth | Childbirth | PSS-I | |
| Noor Mohammadi (39) | 2010 | 2008 | - | 174 | 45 | 129 | 0.94 | P | N | 15 - 55 | Earthquake Survivors | Earthquake | IES-R |
| Attari (40) | 2005 | 2003 | - | 200 | 200 | 0.52 | S | N | 7 - 11 | Students who have seen a suicide | Execution | DSM-Iv | |
| Nohi (41) | 2007 | - | - | 100 | 77 | 23 | 0.46 | P | N | 16 - 60 | Aggressive patients | Aggression | DSM-Iv |
| Yassini (42) | 2006 | 2004 | 3 months after the earthquake | 226 | 0.89 | P | N | Earthquake Survivors | Earthquake | SIP | |||
| Saki (43) | 2013 | 1980 - 1988 | 25 years after the war | 5110 | 0.26 | P | N | Upper 25 | Whole population of Ilam | War | New questionnaire specific to war-induced PTSD | ||
| Saberi (44) | 2013 | 2012 - 2013 | Road accident yearlong | 385 | 385 | 0.19 | P | T | 35 - 40 | Drivers with more than one-year experience | Road accident | PLC-C | |
| Hemmati (45) | 2015 | - | years after the war | 78 | 67 | 11 | 0.25 | P | T | 9 - 18 | Victims of mine explosion | Mine explosion | DSM-IV |
| Mirzamani (46) | 2007 | 2005 | - | 39 | 8 | 31 | 0.74 | P | T | 17 - 70 | Survivors of airplane crash | Airplane crash | PSS |
| Mofidi (47) | 2009 | 1980 - 1988 | - | 1000 | 0.11 | P & S | N | Men:17 - 50, women:16 - 55 | Population of Kurdistan-Iran | War | PCL | ||
| Shaban (48) | 2013 | 2009 - 2010 | 6 to 8 weeks after childbirth | 600 | 600 | 0.17 | P | N | 25 - 30 | Women with childbirth | Childbirth | PSS | |
| Abedian (49) | 2013 | - | - | 100 | 100 | 0.3 | P | N | Upper 18 | Multiparous women with preeclampsia | Childbirth | PPQ | |
| Sadat (50) | 2015 | 2014 | - | 332 | 191 | 141 | 0.482 | P | N | Men:16 - 70, women:13 - 50 | Patients discharged from hospitals | Heart disease | PCL |
| Amirian (51) | 2008 | 2004 - 2007 | - | 100 | 30 | 70 | 0.78 | S | N | 25 - 35 | People seen a suicide | Seeing suicide | DSM-IV-TR |
| Ziaaddini (52) | 2009 | 2010 | 10 years after the earthquake | 466 | 183 | 283 | 0.667 | P | N | 15 - 18 | Earthquake survivors | Earthquake | DSM-IV-TR |
| Hashemian (53) | 2015 | 1980 - 1988 | 16 years after the war | 153 | 87 | 66 | 0.59 | P | N | 18 - 61 | Civilian population | War | CAPS-5 |
| Basharpoor (54) | 2015 | - | - | 100 | 54 | 42 | 0.197 | P | N | 37.53 | Emergency staff | Job | Mississippi scale |
| Sheikhbardsiri (55) | 2015 | 2013 | - | 400 | 229 | 171 | 0.04 | P | N | Emergency staff | Job | Mississippi scale | |
| Hagh-Shenas (56) | 2006 | 2004 | 40 days after the earthquake | 145 | 62 | 83 | 0.81 | P | N | 20 - 40 | Earthquake survivor | Earthquake | PSS |
| Mohamadi (57) | 2015 | 2015 | - | 100 | 49 | 76 | 0.41 | P | N | 21 - 42 | Nurses | Job | PCL-C |
| Haji Maghsoudi (29) | 2005 | 2004 | 5 months after the earthquake | 259 | 108 | 151 | 0.6 | P | N | 17 - 18 | Students | Earthquake | PTSD questionnaire |
| Ahmadi (58) | 2010 | 1980 - 1988 | 20 years after the war | 150 | 150 | 0.78 | P | - | Chemically injured veterans | War | Mississippi scale | ||
| Mohamadi (59) | 2011 | 2005 | 10 months after the earthquake | 1000 | 300 | 700 | 0.2 | P | N | 13.9 (11 - 16) | Earthquake survivors | Earthquake | PSS-I |
| Parvaresh (33) | 2007 | 2014 | 4 months after the earthquake | 160 | 56 | 104 | 0.33 | P | N | Upper 15 | Bam city students | Earthquake | Watson PTSD questionnaire |
Abbreviations: CAPS-5, clinician-administered PTSD scale for DSM-5; CIDI, composite international diagnostic interview; CPSS, child PTSD symptom scale; CPSS, child PTSD symptom scale; IES-I5, impact of event scale; IES-R, impact of event scale-revised; PCL, PTSD checklist; PCL-C, PTSD checklist-civilian; PCL-M, PTSD checklist-military; PCL-DSM-IV-TR, PTSD checklist-diagnostic and statistical manual of mental disorders-fourth edition-text revision; PPQ, patient pain questionnaire; PSS-I, PTSD symptom scale-interview; PSS, posttraumatic stress disorder symptom scale; PTSS-10, post trauma symptoms scale; PTSD, perinatal post-traumatic stress disorder; SIP, structured interview for PTSD; SRS PTSD, self-rating scale for PTSD; SRS-PTSD, self-rating scale for post-traumatic stress disorder.
3.1. Articles’ Descriptive Characteristics
Table 1 provides a summary including the lead author, year of publication, study design, population research, subjects’ roles (e.g., disaster workers), time of data collection, PTSD tool, and the main findings.
The number of participants in all studies was 16546. Based on the year, the studies were done in various years as follows: 2001 to 2005: 3 studies, 2006 to 2010: 20 studies, and 2011 to 2015: 24 studies.
Eight studies only included male participants; nine studies only female participants, and 30 studies both male and female participants. Primary PTSD was investigated in 44 studies and secondary PTSD in four studies. Forty studies investigated natural PTSD and five studies technical PTSD.
The instrument for diagnosing PTSD was divided into five categories:
-Diagnostic and statistical manual of mental disorders (DSM-IV)
-Mississippi scale
-PTSD Symptom Scale (PSS-I)
-Questionnaires and interviews for PTSD based on various criteria
-Posttraumatic stress disorder checklist (PCL)
We categorized studies according to the following PTSD causes as war, earthquake, childbirth, and job; then, we reported the prevalence of PTSD in each category.
3.2. PTSD Prevalence Based on the Cause of PTSD
3.2.1. Childbirth
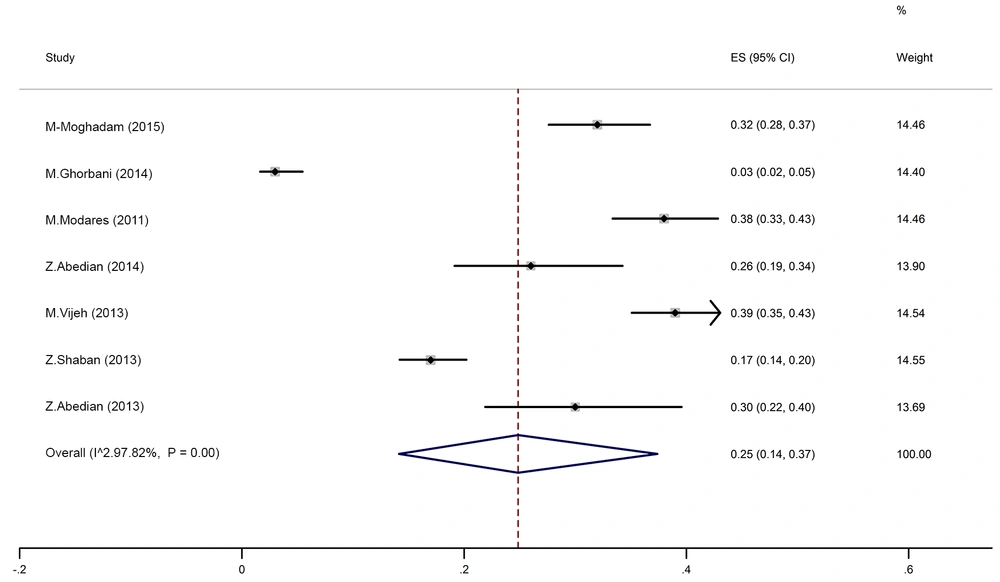
Seven studies investigated PTSD following childbirth. Based on testing heterogeneity (χ2 = 274.98, chi-square DF = 6, P ≤ 0.001) and heterogeneity indices (I2 = 97.82% and tau-squared = 0.13), we used a random-effects model to calculate the prevalence. The pooled prevalence of PTSD in these studies was 25% [95% CI (14 - 37)]. Moreover, Begg’s test [z = 0.75, P value = 0.453) showed that there was no publication bias in results. Figure 1 depicts the prevalence of PTSD in all included studies.
3.2.2. Job
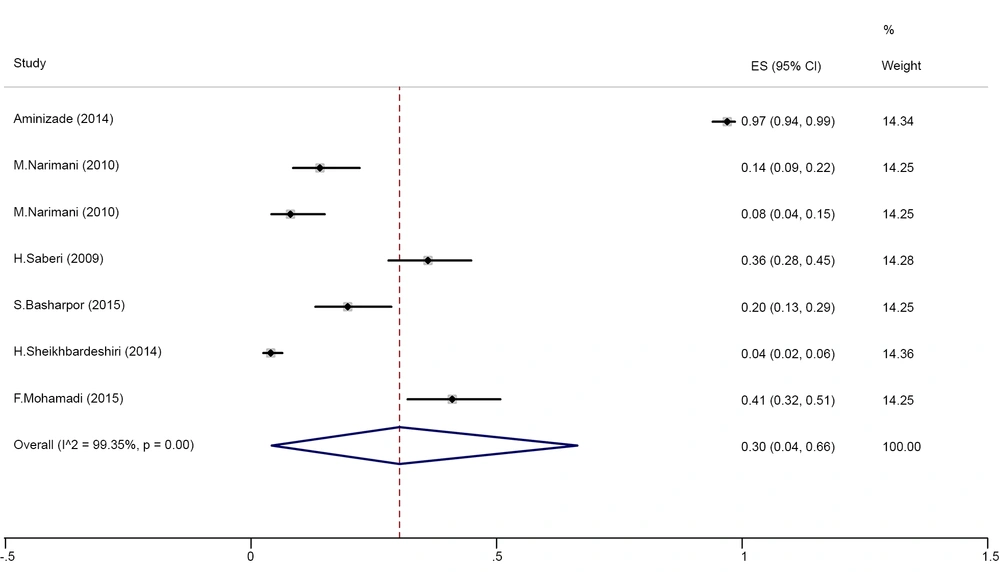
Six studies investigated job-related PTSD. Based on the test of heterogeneity (χ2 = 919.57, chi-square DF = 6, P ≤ 0.001) and heterogeneity indices [I2 = 99.35% and tau-squared=0.98], we used a random-effects model to calculate the prevalence. The pooled prevalence of PTSD in these studies was 30% [95% CI (4 - 66)]. Moreover, Begg’s test (z = 1.65, P value = 0.1) showed that there was no publication bias in results. Figure 2 depicts the prevalence of PTSD in all included studies.
3.2.3. Earthquake
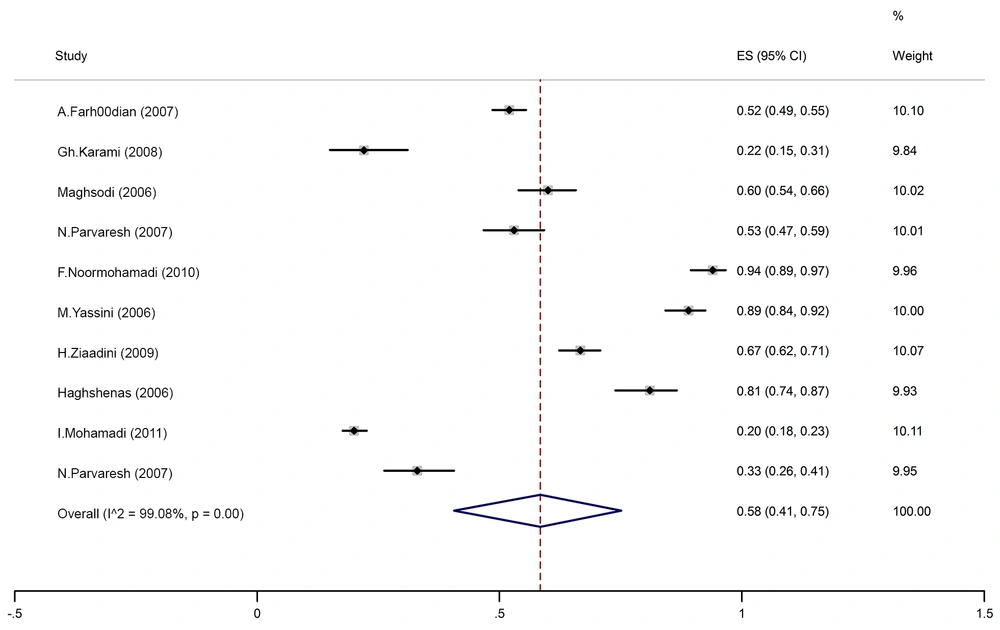
Nine studies investigated PTSD following earthquakes. Based on testing the heterogeneity (χ2 = 974.7, chi-square DF = 9, P ≤ 0.001) and heterogeneity indices (I2 = 99.08% and tau-squared = 0.32), we used a random-effects model to calculate the prevalence. The pooled prevalence of PTSD in these studies was 58% [95% CI (41 - 75)]. Moreover, Begg’s test (z = -0.8, P value = 0.42) showed that there was no publication bias in results. Figure 3 depicts the prevalence of PTSD in all included studies.
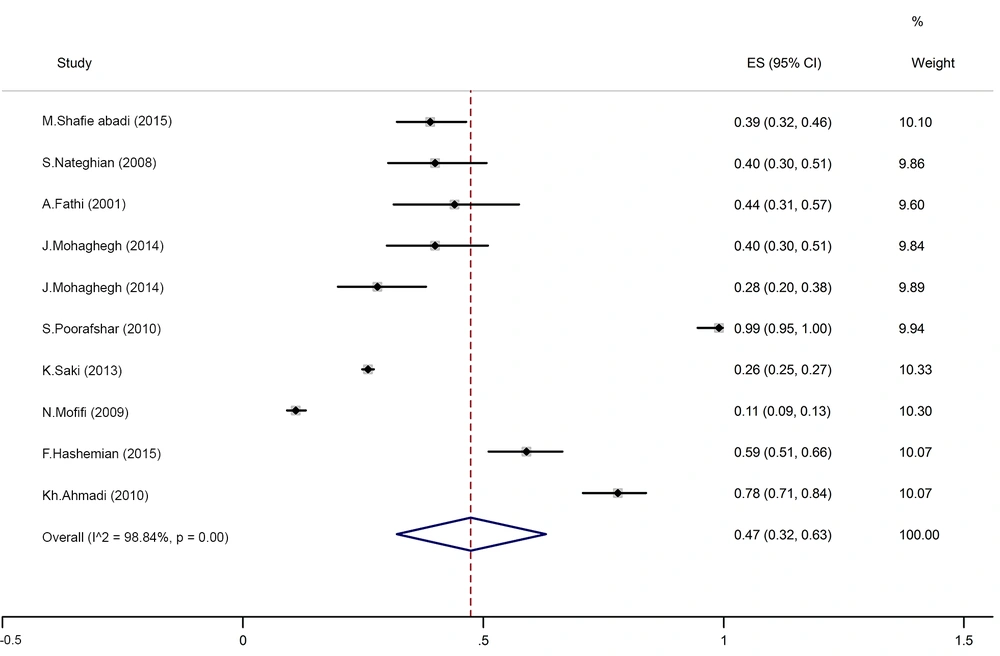
3.2.4. War
Nine studies investigated PTSD following the war. Based on the test of heterogeneity (χ2 = 772.9, chi-square DF = 9, P ≤ 0.001) and heterogeneity indices (I2 = 98.84% and tau-squared = 0.25), we used a random-effects model to calculate the prevalence. The pooled prevalence of PTSD in these studies was 47% [95% CI (32 - 63)]. Moreover, Begg’s test (z = 0.45, P value = 0.65) showed that there was no publication bias in results. Figure 4 depicts the prevalence of PTSD in all included studies. In addition, among these studies, the prevalence of PTSD in four studies (one study reported two prevalence rates) related to the war veterans was 46% [95% CI (27 - 66)] and in three studies related to the civilians was 30% [95% CI (14 - 48)].
3.2.5. Others
Two studies were related to burns and its prevalence was 40% [95% CI (32 - 49)]. Two studies were related to accidents with the prevalence of 11% [95% CI (5 - 21)] and two studies were related to rape victims with the prevalence of 74% [95% CI (67 - 80)].
4. Discussion
In the current research, the highest prevalence of PTSD was found among earthquake survivors (58%). An earthquake with a magnitude of 6.3 on the Richter scale struck Bam city in Iran on December 27, 2003, that was one of the worst disasters of the century. It was disastrous and left more than 40,000 dead and about 30,000 injured people (22, 39, 42, 52). In some studies on adults survived after a disaster, the PTSD prevalence was reported between 30 and 60% (60-62). The results of our study are in agreement with these results.
According to a study by Dai et al. while the reported incidence of PTSD in survivors recognized < 9 months after an earthquake was 28.76%, the incidence of PTSD was 19.48% for survivors evaluated > 9 months after the earthquake for PTSD (63).
Sex and education level are also explanatory variables for the onset of PTSD after earthquakes. Women and those of low education level were more expected to develop PTSD, less expected to use strategies against distress, more susceptive to threats, and more expected to evaluate disasters more negatively (63, 64).
In the current study, there were nine studies associated with wars that reported a prevalence of 47%. Furthermore, PTSD in war veterans was 46% and in the civilians was 30%. The Iran-Iraq War continued from September 1980 to August 1988, with air attacks and heavy artillery fire (37, 53). Exposure to air attacks and massive artillery fire were devastating as they were irregular and people could not avoid or predict its devastating consequences (65). In addition, based on a systematic review in Lebanon during several wars between 1975 and 2006, reported PTSD rates were between 3.7 and 35% (65). According to the mentioned studies, PTSD rates have been increased with time, which is in line with our results.
The rate of PTSD in US military veterans following the Vietnam War varied between 2 and 17% (66). The PTSD prevalence in Australian Vietnam veterans was estimated at 21% in the lifetime and 12% at present (67).
Another study reported that the PTSD rate was 21.6% in the grapes of Wrath War in 1996 and ranged from 15.4 to 35.0% in July 2006 (65). Some of these variations may be associated with the approval of various measures based on various DSM diagnostic measures for PTSD. The gap between exposure to war violence and data gathering, exposure to different types of war events, and the severity of such exposures can be considered as other factors.
In our study, the prevalence of job-related PTSD was 30%. Our literature review showed that the prevalence of PTSD in rescue workers, in general, ranged from 14% to 36%. In addition, we observed higher PTSD rates in studies carried out among ambulance workers. This is consistent with other studies (68). Several studies have confirmed that rescue operations have a higher risk of PTSD incidence (69, 70). These observations confirm that rescue workers comprise a susceptible group for the incidence of PTSD (71, 72).
According to another study, various occupational groups had different rates of risks for PTSD incidence (68, 73). However, the current study confirms the results of previous studies that ambulance workers have the highest PTSD rates among the occupational population of rescuers (68). The very high rate may be because ambulance workers are exposed to higher anxiety at work compared to other rescue groups (74). A study reported that rescuers from Asia, at least partially, have a higher PTSD prevalence compared to the European counterparts (68).
In our study, seven studies investigated PTSD following childbirth and the prevalence of PTSD in these studies was 25%. PTSD after childbirth was first defined by Bydlowski and Raoul-Duval (75) with painful experiences during labor leading to tocophobia and recurrence of tension, nightmares, and flashbacks towards the end of the next pregnancy. Numerous authors afterward suggested that PTSD may occur after distressing labor or delivery (76, 77).
A difficult or traumatic birth may be an important stressor, similar to the known stressors such as violence or war causing PTSD symptoms. The stressful experience is often a pain but loss of control and fear of death can also be a kind of pain (78). Studies accomplished in the USA, Sweden, Germany, the UK, Australia, and Canada have reported a prevalence ranging from 0.9 to 5.6%. There is a meaningful relationship between the creation of PTSD and the control source, the level of social support, and the previous experience of injuries in these studies (75).
In the current study, two studies were related to burn cases, and the reported prevalence was 40%. In other studies, the pain was also associated with PTSD incidence in injured patients including burn patients (79, 80). Moreover, in our study, two studies were related to accidents with the prevalence of 11% and two studies were related to rape victims with the prevalence of 74%.
Post-traumatic stress disorder in events that cause significant damage should be checked as this disorder develops especially two months after the accident. Driving accidents are responsible for more than 50% of deaths worldwide at the age of 15 - 44 (81). In Iran, driving accidents are the second leading cause of death (82). In a systematic review by Olofsson et al. which examined 12 studies on post-traumatic stress disaster related to accidents, 29% of post-traumatic stress was reported to reduce to 13% after 3 - 6 months of injury (83).
Violence and sexual harassment are of important issues that are considered in many perspectives such as psychological, social, cultural, demographic, political, and health viewpoints, and are observed in all countries and all social, cultural, and religious groups as they affect thousands of women every year. However, it is believed that over 80% of sexual harassment cases are not reported and the actual incidence is higher than what is now reflected (21). The results of a study by Zinzow et al. showed about 30% to 50% of victims developed PTSD after the onset of PTSD symptoms (84). In addition, in a study by Alynch, the prevalence of PTSD was reported to follow completely different rates. In victims with less experience of sexual harassment, this rate was 4%, and in those with a higher degree of sexual harassment, it was 80% (85).
In this study, our purpose was to carry out a systematic review of the evidence regarding PTSD following the war and disasters that might recommend a direction for research and intervention. Arguably, the available information is sufficient to suggest plausible ranges of PTSD prevalence that can be expected after war and disasters, within the particular exposure groups.
The current study had some limitations. We opted to include a wide range of PTSD studies, with differences in methodologies. In addition, this meta-analysis only included cross-sectional studies, making to understand the temporal order of correlations between explanatory variables and PTSD. This study has several strengths including the fact that this is the first systematic review of PTSD prevalence in the Iranian population.
5. Conclusions
The results suggest that the burden of PTSD among Iranian populations exposed to war and disasters is substantial. PTSD is correlated with a range of factors including sociodemographic and background factors and event exposure characteristics. It is suggested that counseling and treatment services at hospital and community levels be provided to improve the deleterious consequences of war and disasters in these vulnerable groups in the Iranian population.