1. Context
Gender identity disorder (GID), gender dysphoria, or transsexualism are terms defined by the diagnostic and statistical manual of mental disorders (DSM) to describe an individual’s continuous distress about his/her biological sex or assigned gender (1, 2). The International Classification of Diseases (ICD) has defined transsexualism as a complex mental disorder (3). Although the major causes of GID are not completely understood, genetics, psychosocial factors, and neurodevelopment might be involved (1). GID is potentially associated with the high prevalence of anxiety disorders, mood disorders, and suicidality in adults (1). In a meta-analysis, the prevalence of transsexualism was 4.6 per 100,000 individuals, i e, 6.8 for male-to-female (MtF) and 2.6 for female-to-male (FtM) transsexuals (2). Iran is the first country in the Middle East and the second country in the world following Thailand to perform sex reassignment surgery (SRS) (4, 5).
In many countries, transsexual people are treated according to the standards of care by Harry Benjamin International Gender Dysphoria Association (6). Treatment for transsexual people includes a set of hormonal and surgical procedures, which changes the physical appearance and function of sexual organs in order to facilitate transition to the opposite sex (7).
SRS is a surgical procedure usually necessary for both MtF and FtM transsexuals in order to reduce their distress caused by physical appearance. SRS, as a controversial medical intervention, is performed in 29% - 93% of transsexuals, using different methods (8, 9). This intervention, which involves psychological, social, and legal aspects, is the most important step in changing the sexual characteristics of a transsexual individual to resemble those of the opposite gender (9, 10). SRS in MtF transsexuals involves implantation of breast prostheses, construction of a neovagina and clitoris, and other feminizing surgeries. On the other hand, surgeries for FtM transsexuals include hysterectomy with bilateral oophorectomy, construction of the neophallus, and mastectomy (11, 12). SRS is performed as part of the treatment of transsexuality for more than 70 years (13). It is also part of the treatment allowed in Iran since 1964 for transsexuality (14).
Some articles reported improvements in the surgical outcomes and quality of life (QoL) in transsexual individuals undergoing surgery (15-20). QoL includes different aspects of mental health, physical and social functions, and satisfaction (21). On the other hand, SRS may lead to several limitations in the personal and social life aspects of transgender individuals. According to the literature, this procedure can reduce the individual’s social capital and QoL.
In this regard, Javaheri and Hoseinzadeh reported that the mean social capital and QoL of transsexual individuals were lower than expected (22). On the other hand, several studies demonstrated that transsexuals have a higher QoL (13, 23-25) and personal satisfaction (26-28) after genital surgery. In a study, Vasegh Rahimparvar et al., reported that the QoL of MtF transsexuals was similar to that of ordinary females (29).
2. Objectives
Individuals who are candidates for SRS have little information about the overall outcomes and QoL following the surgery. Also, experts who serve as consultants for these cases have inadequate knowledge in this area (13). Despite the long history of treatment for transsexuality, there is a scarcity of information regarding its psychiatric morbidities (30). Some studies show that SRS has a positive effect on the individual’s wellbeing and sexual function (20, 31, 32). However, the outcomes of SRS vary in different countries and cultures. Therefore, the current systematic review and meta-analysis aimed at reviewing the literature, and evaluating different dimensions of QoL after SRS in transgender individuals.
3. Data Sources
3.1. Search Strategy
The current systematic review and meta-analysis included all articles published worldwide in the area of QoL after SRS. The search in the current study had no language limitation; however, all the three non-English language articles found by search were excluded based on their abstracts. A search was conducted in English databases, including PubMed, Scopus, PsycINFO, ScienceDirect, and Google Scholar in accordance with the PRISMA 2009 checklist without any time limitations. The final literature search was performed on 12 June 2017.
The authors used a search strategy by combining MeSH terms and keywords used in the article titles and abstracts. The keywords included sex OR gender AND reassignment surgery OR reassignment operation OR reassigned OR sex change OR sex reversal OR transpersonal OR sexual transition OR gender dysphoria OR transsexualism OR transsexual OR transgender OR gender identity OR male-to-female OR female-to-male OR MtF OR FtM AND quality of life OR QoL OR quality adjusted OR wellbeing. The reference lists of potentially relevant articles were also searched in order to find other possibly relevant studies.
4. Study Selection
In the current review study, all articles examining MtF and/or FtM transsexuals undergoing SRS in terms of QoL were retrieved. Studies were included regardless of the sample size, age of the participants, follow-up duration, or type of transsexualism. Two reviewers examined all titles and abstracts, simultaneously. Discrepancies between the reviewers were resolved by the third reviewer.
The exclusion criteria for articles were: (1) inadequate documentation of the methodology or results; (2) articles irrelevant to the topic of the study; (3) review articles, qualitative studies, editorials or letters, commentaries, case reports, dissertations, or conference proceedings; (4) duplicate publications; and (5) studies focused on the physical and psychological complications of transsexual people.
4.1. Quality Assessment
The methodological quality of studies was assessed by two authors independently, and disagreements were resolved by consensus. The 22-item STROBE 2007 (version 4) checklist (33) was used for the quality assessment of studies, with yes/no questions (“Yes/Y”, presence of the item; “No/N”, absence of the item). The total score is the sum of positive answers. Cohort studies scored ≥ 7, as well as cross sectional studies scored ≥ 6 were considered as high-quality. In the current review, all included studies were of high-quality (34) (Table 1).
| Study | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Papadopulos et al., 2017 (10) | Cardoso da Silva et al., 2016 (35) | Castellano et al., 2015 (36) | Davey et al., 2014 (37) | Jokic-Begic et al., 2014 (38) | de Vries et al., 2014 (39) | Motmans et al., 2012 (40) | Vasegh Rahimparvar et al., 2012 (29) | Wierckx et al., 2011 (41) | Javaheri and Hosseinzadeh, 2011 (22) | Parola et al., 2010 (42) | Kuhn et al., 2009 (13) | Weyers et al., 2009 (43) | Newfield et al., 2006 (24) | Lawrence, 2006 (44) | Rakic et al., 1996 (25) | |
| Title and Abstract | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Introduction | ||||||||||||||||
| Background/Rationale | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Objectives | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y |
| Method | ||||||||||||||||
| Study Design | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Setting | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y |
| Percipients | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Variables | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Data Sources/ Measurement | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y |
| Bias | N | N | N | N | N | Y | N | N | Y | N | N | N | Y | Y | N | N |
| Study Size | N | N | Y | Y | N | Y | Y | Y | Y | Y | N | N | Y | Y | Y | Y |
| Quantitative variables | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Statistical Methods | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y |
| Result | ||||||||||||||||
| Participants | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Descriptive Data | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Outcome Data | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Main Results | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Other Analyses | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Discussion | ||||||||||||||||
| Key Results | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y |
| Limitations | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | N | N | Y | Y | Y | Y |
| Interpretation | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y |
| Generalizability | Y | N | N | N | N | N | N | N | N | N | N | N | N | Y | Y | N |
| Other Information | ||||||||||||||||
| Funding | Y | Y | Y | N | N | Y | Y | N | N | N | N | N | Y | N | N | N |
| Total | 20 | 19 | 20 | 19 | 17 | 21 | 20 | 19 | 20 | 15 | 14 | 17 | 21 | 21 | 20 | 19 |
Abbreviations: Y, Yes; N, No or unclear.
5. Data Extraction
The following information was abstracted for each study: authors’ names, year of study, study setting, study design, population description (MtF or FtM transsexuals), mean sample age, sample size, instruments, and treatment duration (Table 2). In addition, QoL was extracted for each study (Table 3).
| Study | Country | Year | Study Design | MtF or FtM Transsexuals | Intervention/Control Group | Mean Age, y | Instrument | Hormonal Status | Treatment |
|---|---|---|---|---|---|---|---|---|---|
| Papadopulos et al. (10) | Germany | 2017 | Retrospective study | 47 MTF transsexuals | Results were compared with normative data | 38.3 (18 - 57) | A standardized self-assessment test on QoL | Use of hormone cream | SRS was performed between 2007 and 2013. |
| Cardoso da Silva et al. (35) | Brazil | 2016 | Prospective cohort study | 47 MtF transsexual | 47 MtF before and after SRS | 31.23 (16 - 54) | The WHOQOL-100 questionnaire | 100% | SRS, hormonal therapy, and supportive group therapy |
| Castellano et al. (36) | Italy | 2015 | Case-control study | 60 transsexuals (46 MtF transsexuals, 14 FtM transsexuals) | 60 transsexuals, 60 matched controls | 39.0 (18 - 65) | WHOQOL-100 test | 100% | SRS at least 2 years ago and hormonal therapy |
| Davey et al. (37) | The UK | 2014 | Case-control study | 103 individuals with gender dysphoria (63 females and 40 males) | 103 individuals with an age and gender matched non-clinical control group | 36.4 (18 - 72) | SF-36 (version 2) | No use: 19 (18.5%); Current use: 81 (78.6%); Previous use: 1(1%) | All participants were involved in the treatment at one of three phases of assessment, real-life experience (RLE), or post-surgery”. |
| Jokic-Begic et al. (38) | Croatia | 2014 | Quantitative and qualitative self-report methods | 3 MtF transsexuals and 3 FtM transsexuals | - | 33.8 | The SF-36 | NR | SRS in the last 15 years |
| de Vries et al. (39) | The Netherlands | 2014 | Longitudinal study | 22 MtF transsexuals and; 33 FtM transsexuals | - | 21; 20.5 | The WHOQOL-BREF (quality of life measure developed by the World Health Organization) | 100% | At least 1 year after GRS |
| Motmans et al. (40) | Belgium | 2012 | Cross sectional | 77 MtF transsexuals and; 63 FtM transsexuals | - | 42.26; 37.03 | SF-36 | 58 (96.7%) in transmale and 70 (94.6%) in transfemale | Hormonal therapy and trans-related surgery were not in the year of the study |
| Vasegh Rahimparvar et al. (29) | Iran | 2012 | Cross sectional | 46 MtF transsexuals | 184 women | NR | SF-36 | NR | At least 1 year after GRS |
| Wierckx et al. (41) | Belgium | 2011 | A single center, cross sectional | 49 transmale | 976 Dutch males and 976 Dutch females | 37 (22 - 54) | Dutch version of the SF-36 | 100% At least 2 years before SRS | SRS between 1987 and 2009; All participants underwent SRS (hystero-oophorectomy and mastectomy); 8 years ago on average (2 - 22 years) |
| Javaheri and Hosseinzadeh (22) | Iran | 2011 | Cross sectional | 93 MtF transsexuals and 75 FtM transsexuals | - | 26 | Self-structured questionnaire | NR | NR |
| Parola et al. (42) | France | 2010 | A personality study | 15 MtF transsexuals and; 15 FtM transsexuals | - | SF-36 | - | Hormonal-surgical reassignment at least 2 years ago | |
| Kuhn et al. (13) | Switzerland | 2009 | Case-control | 52 MtF transsexuals and; 3 FtM transsexuals | 20 controls | 51 | King’ s Health | 100% | SRS 15 years ago |
| Weyers et al. (43) | Belgium | 2009 | Cross sectional | 50 MtF transsexuals | 766 females | 43.06 | SF-36 | 94% | SRS ≥ 6 mn |
| Newfield et al. (24) | The USA | 2006 | Cross sectional | 376 FtM transsexuals | The US general population | 32.8 | SF-36 (during or in the past 4 weeks) | 67% received testosterone | Testosterone therapy and/or SRS |
| Lawrence (44) | The USA | 2006 | Prospective study | 232 MtF transsexuals | - | 47 | 21-point Likert scale | 100% | - |
| Rakic et al. (25) | Yugoslavia | 1996 | A follow-up study | 22 MtF transsexuals and 10 FtM transsexuals | - | 26.36 in MtF transsexuals and 27.8 in FtM transsexuals | Self-structured questionnaire | - | - |
Abbreviations: GRS, gender reassignment surgery; FFS, facial feminization surgery; SF-36, 36-item short form; SRS, sex reassignment surgery.
| Study | Quality of Life |
|---|---|
| Papadopulos, et al., 2017 (10) | Improvement of QoL was experienced by 91% after SRS |
| Cardoso da Silva et al., 2016 (35) | After SRS psychological and social relationships improved and physical health and level of independence worsened. The environment, and spirituality, religion and personal beliefs domains did not change |
| Castellano et al., 2015 (36) | The QoL scores in transsexuals were similar to those of the matched controls |
| Davey et al., 2014 (37) | Individuals with gender dysphoria displayed higher psychopathology, and lower QoL and life satisfaction compared with controls |
| Jokic-Begic et al., 2014 (38) | 3 transsexual individuals had lower QoL |
| de Vries et al., 2014 (39) | WHOQOLa physical: mean (SD): 15.22 (2.49) |
| WHOQOL psychological: 14.66 (2.44) | |
| WHOQOL social relations: mean (SD): 14.91 (2.35) | |
| WHOQOL environment: mean (SD): 15.47 (2.06) | |
| Modarresi Fard et al., 2014 (45) | The results showed that from the QoL dimensions, physical health (P < 0.000), psychological QoL (P < 0.005), and the gender roles of patients were significantly different before and after SRS |
| Motmans et al., 2012 (40) | The QOL of transgender females did not differ significantly from the general Dutch female population, although transgender males showed reduced mental health-related QoL compared to the general Dutch male sample |
| Transgender females had a lower QoL than transgender males for the subscales physical functioning and general health, but better QoL for bodily pain | |
| Vasegh Rahimparvar et al., 2012 (29) | Mean total score of QoL was 69.98 ± 17.4 and 68.87 ± 15.3 in MtF transsexuals and controls (P = 0.594) |
| The physical pain was higher in MtF transsexuals than controls (P = 0.01) | |
| Javaheri and Hosseinzadeh 2011 (22) | Only 20% of transsexuals were highly satisfied |
| 10% had a good level of mental health | |
| QoL was 29.51 ± 12.41 and 36.445 ± 12.28 in MtF transsexuals and FtM transsexuals, respectively (P < 0.001) | |
| Wierckx et al., 2011 (41) | Transsexual males generally had a good QoL and experienced satisfactory sexual function after SRS. |
| Physical functioning: 85.9, role-physical: 83.3, bodily pain: 75.8, general health: 70.9, vitality: 62.1, social functioning: 85.5, role-emotional: 83.0, mental health: 72.6 | |
| Parola et al., 2010 (42) | SRS improved the QoL |
| FtM transsexuals had better social, professional, friendly lifestyles than MtF transsexuals | |
| Kuhn et al., 2009 (13) | It was significantly lower in general health, personal, physical, and role limitations in transsexuals |
| Weyers et al., 2009 (43) | Engaged females got physical and mental component summary scores similar to those of transsexual females not currently engaged, although engaged females got higher scores in vitality (P = 0.049), social functioning (P = 0.008), and mental health (P = 0.025) |
| Newfield et al., 2006 (24) | QoL and concept of health were lower among the FtM transgender |
| participants compared to those of the MtF population (P < 0.01), particularly in mental health | |
| QoL reduced among the FtM transsexuals compared to the US males and females, particularly in mental health and social functioning | |
| Physical functioning and physical health scores were higher than the general population | |
| Physical role and bodily pain in transsexuals were not different from those of the general population | |
| Rakic et al., 1996 (25) | QoL was significantly different before and after SRS. Interpersonal relationship was better after surgery |
5.1. Statistical Analysis
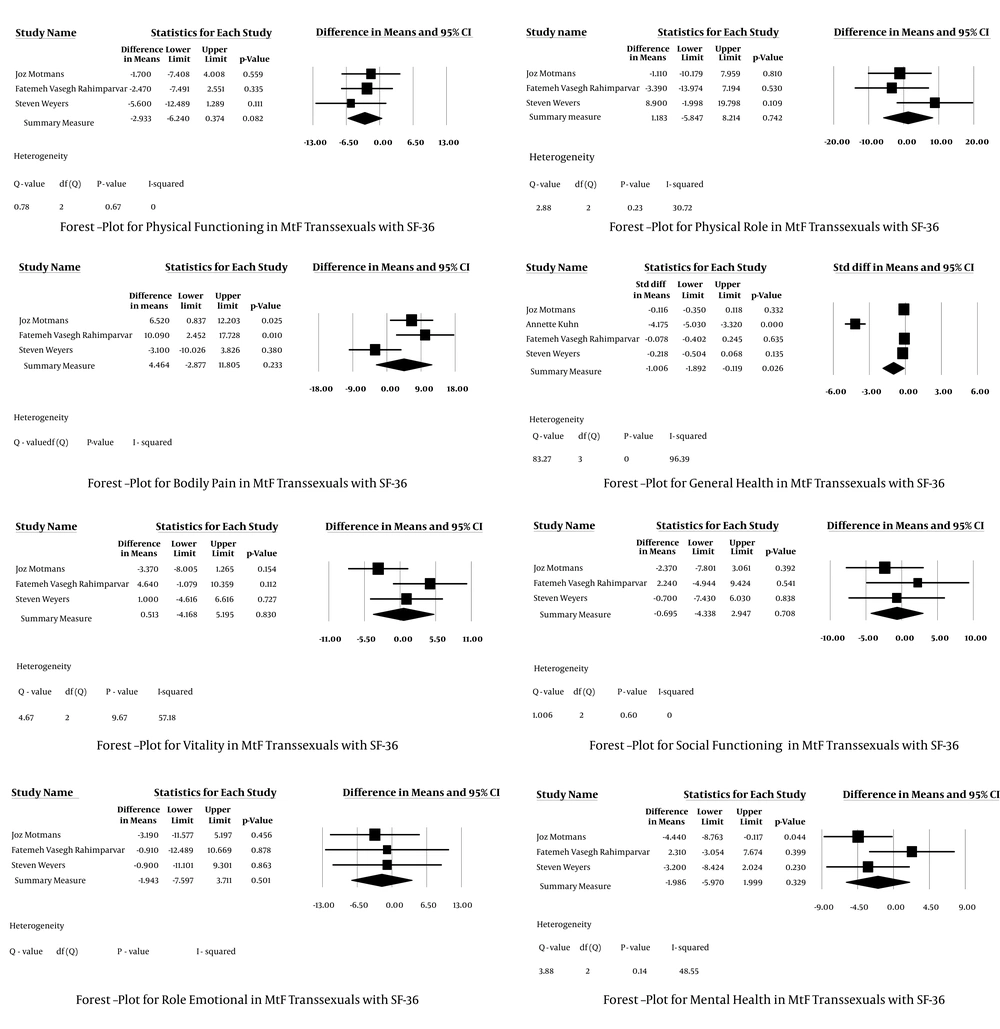
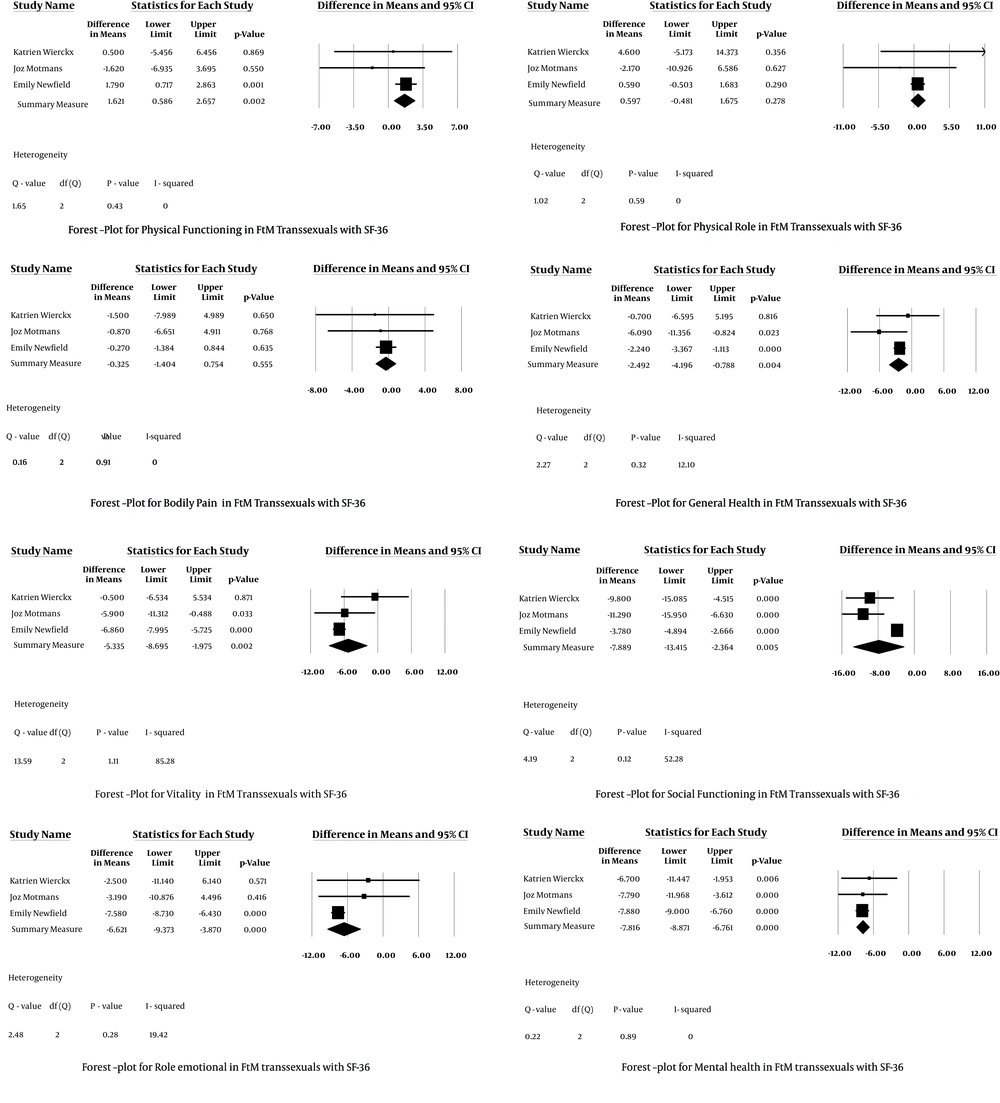
A meta-analysis of studies reporting adequate quantitative data after SRS was conducted. The main effect size indicated the difference in the mean scores of QoL after surgery. Forest plots were depicted for graphic presentation of the results (Figures 1 and 2). Cochrane Q test was also used to evaluate heterogeneity and P values less than 0.05 were considered statistically significant. The I2 index was also used to quantify heterogeneity. Data pooling was carried out separately for each aspect of QoL in transsexual females and males (six meta-analyses). The calculation was conducted using Comprehensive Meta-Analysis Software version 2. Meta-analyses were performed independently for FtM and MtF transsexuals.
6. Results
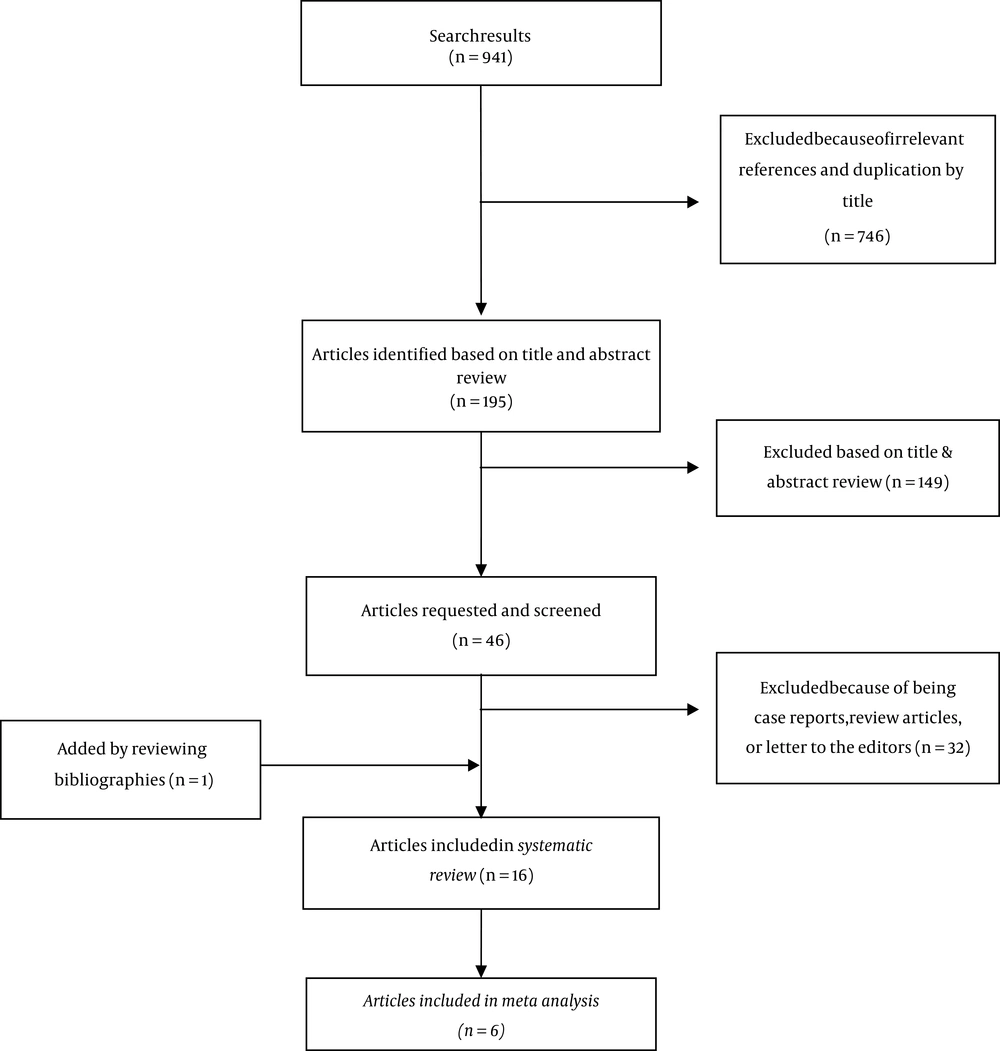
The literature search indicated 941 articles. The full-texts of 46 studies were screened after reviewing the articles based on their titles and abstracts, removing duplicate and irrelevant articles (deletion of 746 articles), and assessing the articles in detail (deletion of 149 articles). Finally, according to the inclusion criteria (deletion of 32 articles), 16 articles were retrieved in the current systematic review, and only six studies were included in the meta-analysis (Figure 3). In addition, one more article was found by checking the reference lists of the included articles.
Article search strategy based on PRISMA guidelines (46)
Out of 16 studies, two were conducted in the USA (24, 44), three in Belgium (40, 41, 43), two in Iran (22, 29), one in Switzerland (13), one in the UK (37), one in Croatia (38), one in Yugoslavia (25), one in France (42), one in Brazil (35), one in the Netherlands (39), one in Germany (10), and one in Italy (36). Six studies had a cross sectional design (22, 24, 29, 40, 41, 43), four were case-control studies (10, 13, 36, 37), four were cohorts (25, 35, 39, 44), and two had a mixed-methods design (quantitative data were assessed) (38, 42).
The samples in the review included a total of 1449 FtM and MtF transsexuals (768 MtF and 681 FtM transsexuals). Hormonal therapy was administered in transsexuals in 10 studies (67% to 100%). Based on the findings, SRS was performed from six months to 22 years ago. The mean age of the subjects ranged 20.5 to 37.3 years in FtM transsexuals and 21 to 56.9 years in MtF transsexuals.
QoL was measured using the short-form health survey (SF-36) in eight studies (24, 29, 37, 38, 40-43), WHOQOL-BREF questionnaire in three studies (35, 36, 39), King’s health questionnaire in one study (13), self-structured instruments in two studies (22, 25), a standardized self-assessment tool for QoL in one study (10), and a 21-point Likert scale in one study (44). Out of 15 studies evaluating the QoL, nine examined both FtM and MtF transsexuals (13, 22, 25, 36-40, 45), two focused on FtM transsexuals (24, 41), and four examined MtF transsexuals (29, 35, 43, 44). Also, there was a control group in eight studies (13, 24, 29, 36, 37, 40, 41, 43). QoL was evaluated before and after the surgery in only two studies (25, 35).
In terms of demographic variables, the number of single subjects was higher in MtF transsexuals compared to normal females (P < 0.09) (29). In fact, the number of married transsexuals was significantly lower than the general population (P = 0.019) (13). In addition, the level of income and insurance coverage were lower in MtF transsexuals compared to normal females (P < 0.05) (29); nevertheless, in a study, 74.8% of FtM transsexuals were under insurance converge (24). According to two studies, the level of education was high-school diploma or higher in 88% of FtM transsexuals and 89% of all transsexuals (24, 45).
Figures 1 and 2 represent the meta-analyses of mean differences in multiple aspects of QoL in comparison with the controls. General health was not significantly different between MtF transsexuals and the controls. Additionally, all aspects of mental health were significantly lower in FtM transsexuals rather than controls, except for physical role and bodily pain. Modarresi Fard et al., found that SRS can improve the QoL and physical and psychological health of individuals with GID (45). A study also reported that participants who received testosterone had a higher QoL (24). In another study, it was revealed that the level of education had a direct correlation with three dimensions of QoL (i e, physical function, mental health, and social functioning) in transsexuals (22), while another study did not report any significant differences between MtF transsexuals and normal females (29). Also, there was no significant difference between MtF transsexuals and the control group in terms of the mean age (29).
Social functioning, emotional role, and mental health were significantly lower in FtM transsexuals aged 44 years or younger, compared to normal males and females. Conversely, physical health was not significantly different between FtM transsexuals and females in any age group (24). Newfield et al., also found no significant difference in the duration of surgery (24).
7. Discussion
The current systematic review and meta-analysis was conducted to evaluate QoL in transsexual individuals undergoing SRS. The results showed that some dimensions of QoL were not significantly different between individuals undergoing SRS and the general population. QoL improved following SRS in some dimensions, including bodily pain, emotional role, and mental health in MtF transsexuals and physical function and physical role in FtM transsexuals. Conversely, bodily pain, general health, social function, vitality, mental health, and emotional role were lower in FtM transsexuals compared to the general population, similar to physical function and general health in MtF transsexuals.
Although gender had a major influence on the findings, the QoL dimensions in MtF transsexuals were similar to those of normal females, except for general health. On the other hand, QoL dimensions in FtM transsexuals were not similar to those of normal males, except for the dimensions of bodily pain and physical role. Therefore, it can be concluded that transsexual people have special needs and conditions that should be distinguished and taken into account.
Transsexuality and its impact on the individual’s life are observed in all cultures. Gender identity is a part of human rights, and accordingly, care is provided for transsexuals in Western European countries, the USA, and developed countries in Eastern Asia (38). Nonetheless, Jokic Begic found that transsexual people do not receive adequate support and have insufficient access to treatment, as medical professionals have inadequate knowledge about transgender health care (38). Additionally, it is important to support the partners, families, and friends of transgender people (26).
The complications of SRS may necessitate additional surgeries, with possible long-term outcomes on the mental health of transsexual people. Overall, the number of required surgeries for SRS complications (or other related factors) is high in FtM transsexuals (47), as well as MtF ones (48). In this regard, a study showed that transsexual females have a lower mental burden than transsexual males (40).
Additionally, demographic and socioeconomic characteristics have strong effects on the QoL of transsexual people. In this regard, Motmans et al., reported that age is negatively correlated with some dimensions of QoL, such as physical health. Moreover, they found that older transsexual people had lower SF-36 scores in some QoL dimensions, such as physical function and general health (40).
The QoL scores were significantly lower in transgender individuals with lower educational levels and household income, compared to those with higher education and household income. In addition, older, unemployed, and single transsexuals obtained lower QoL scores in comparison with younger, employed, and married transsexuals (40). Also, well-educated transsexuals could establish a better relationship with others and had a high QoL because of their extensive information in this area (22).
Some studies report that most transsexual people were single. However, the impact of civil status on QoL is a controversial topic, and its independent effects are not well-established (13). Based on the findings, FtM transsexuals experience a greater reduction in physical health in comparison with normal males, whereas no significant difference was found between FtM transsexuals and females from the same age category; it can be attributed to the fact that FtM transsexuals are biologically female and physically similar to females, not males (24).
One of the strengths of the current study was that the literature search was carried out without any time limitations among publications. Also, QoL was assessed using validated tools in most studies, which could by itself strengthen the quality of these studies (13). On the other hand, a limitation of the study was that only the studies focusing on QoL as the main objective were retrieved; therefore, some studies might be missed. In addition, numerous search criteria were used in the current review in order to identify QoL after SRS in the published literature.
Another limitation of the study may be that many instruments were not transgender-specific and might have lower sensitivity. The number and design of retrieved studies were among other shortcomings. Selection bias should also be considered in the current systematic review, since transsexual people, who agreed to participate in these studies, might have more satisfaction and better outcomes, compared to individuals who did not accept to participate (41).
It should be noted that in most of the articles, data were not compared before and after hormonal therapy and SRS. As the current review indicated, some transsexual people used hormonal therapy before and after SRS in eight studies; therefore, hormonal therapy might have affected the results. In fact, the literature suggests that gender-affirming hormonal therapy can improve the QoL of transgender adolescents (49). Also publication bias could be a potential threat for the validity of the findings so that the results should be interpreted with more caution (50).
Overall, patients with GID should be diagnosed as early as possible, and SRS should be carried out at younger ages. It should be noted that transsexual people are a vulnerable group, requiring economic, social, medical, and family support. Also, it is recommended to investigate other factors influencing the QoL of such people; i e, cultural, religious, social, and demographic variables.
8. Conclusions
Based on the findings, there were no significant difference between MtF transsexuals after SRS and the general population in some dimensions of the QoL, including physical role, vitality, and social function. The dimensions of bodily pain, emotional role, and mental health improved in MtF transsexuals, while physical function and physical role improved in FtM transsexuals. However, no improvement was observed in other dimensions, such as physical function and general health in MtF transsexuals, as well as bodily pain, general health, social function, vitality, mental health, and emotional role in FtM transsexuals. Overall, several factors may affect the QoL in transsexual people, such as demographic characteristics, socioeconomic factors, and hormonal therapy. In the majority of studies, data were not compared before and after SRS; therefore, further studies are needed to examine all aspects of QoL before and after SRS in MtF and FtM transsexuals. Also, factors affecting the QoL in such individuals should be examined.