1. Background
As a major health challenge, burns are among the most common health-related incidents in different societies (1). According to World Health Organization statistics, 1.3 in 100,000 burns occur in underdeveloped or developing countries, and the rate is 0.14 in developed countries (2). Half of all burns worldwide, 3.8 million burns, occur in Asia (3). In Iran, 24000 - 28000 burn victims require hospitalization annually, and their annual mortality rate is 4.6 - 5.6 per 100,000 individuals. Furthermore, permanent disabilities remain in 8% of burn survivors (4). Burns of 15% or more in adults and 10% or more in children lead to a poor prognosis (5).
Burn injuries affect not only physical health but also mental health, causing long-term changes, affecting patients’ quality of life, and placing a great burden on families and the healthcare system (6). Following burns, 25 - 50% of burn victims suffer from psychological problems (7). Depression and posttraumatic stress disorder (PTSD) are two major problems that affect a significant percentage of burn survivors of various stages (8). There is an association between burn injuries and mental health issues, such as substance abuse, sleep disorders, impaired body image, and anxiety (7). Acute stress disorder (ASD), PTSD, and mild depression are observed in about 30%, 45%, and 54% of burn survivors, respectively. In addition, the suicide rate in burn survivors is five times higher than in the general population. Burn-related mental health issues can affect victims’ physical functioning and quality of life (9).
Despite numerous post-burn problems, the need for psychological care has not changed over time, and functional limitations, scars or deformities, chronic pain, or traumatic stress associated with initial injuries are at the heart of post-hospital recovery for burn victims (10, 11). Meanwhile, improving the quality of life for burns, increasing compliance with the rehabilitation program, and psychosocial adjustment can be achieved based on proper and timely screening and appropriate psychological interventions (8). An early post-discharge follow-up program reduces the risk of readmission in patients admitted for acute medical conditions (12). Home visits and follow-ups by telephone are two options for follow-up care (13). Nursing home care can be a source for the delivery of rehabilitation programs and the exploration of patients’ demands and educational needs (14). Achieving this goal is possible through ongoing interaction between the patient and care providers (15).
In Iran, the healthcare system gives high priority to hospital-based services over community health services (16). A study showed that home healthcare can preserve health and is viewed as a way of managing social resources (17). Based on the different factors from policy-making decisions to changes in users’ attitudes, home care has become a necessity in the healthcare system (18). It was necessary to conduct the present study in western Iran, Kermanshah, for several reasons. Firstly, the psychological problems, changes in health status, and body image will be challenging in the first year after burn injuries (19). Secondly, self-immolation is common in Iran’s western and northwestern regions, such as Kermanshah (20). Considering that no study has been conducted on the home care of burn survivors in Kermanshah, the present study was carried out.
2. Objectives
The present study aimed to determine the effectiveness of a home care plan in the mental health status of burn survivors 3 and 6 months after hospital discharge.
3. Methods
This randomized clinical trial (RCT) by a pretest-posttest design with intervention and control groups was carried out from July 2016 to April 2018. This study was conducted in a burn department of an educational hospital in Kermanshah, west of Iran. The inclusion criteria were the age range of 18 - 80 years, the severity of the burn greater than 15% (grades II and III), being oriented to time, place, and person, having the ability to respond to the study questionnaires and communicate with the nurse, and no history of burn injuries. The exclusion criteria were survivors’ death or migration to other cities during the study process, no response to the nurse’s phone calls during the follow-ups, and a drop out of communication with the nurse researcher.
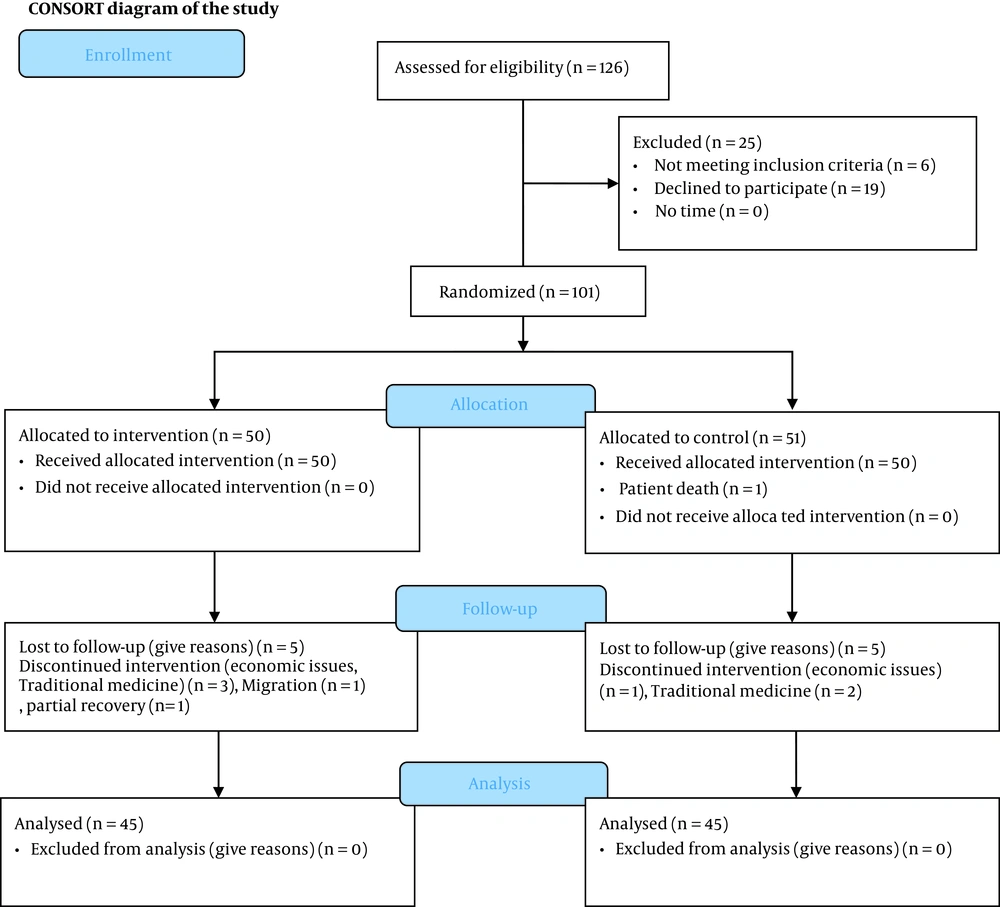
The sample size was defined based on the results of previous studies, including mean quality of life (21) and the prevalence of mental health problems in burn survivors (22). Then, based on the formula at a confidence level of 95%, a power of 80%, and d = 7 (21), and with an attrition risk of 20%, 45 samples were determined for each group (total sample, n = 90). The eligible samples were recruited in the study during the hospital discharge based on the inclusion criteria and then were randomly divided into two groups. A randomized block design was used to ensure an equal distribution of samples into the two groups with different depths and severity of burns. A randomization list was created by PASS software (version 11) for random allocation. There were an intervention and a control group with block size 8, list length 90, and two strata (category A: burn severity within 15 - 25%; category B: > 25%; the percentage of burns was based on the Lund and Browder chart in the patient’s file). A randomization list for 90 samples was produced based on the burn percentage. Figure 1 depicts the CONSORT flowchart of the most common reasons for the dropout of the samples. A blind approach was used, and the samples and burn clinic staff were unaware of the sample assignment to the intervention or control group.
A specific home care plan was developed for burn survivors in the intervention group. This plan was a dynamic and continuous care process that included mental health screening based on the General Health Questionnaire-28 (GHQ-28), education, and referral to specialists (psychologists and psychiatrists or psychiatric centers) and follow-ups. Follow-ups and psychological status reassessments were planned after referring the survivors to psychiatric centers. The survivors in the intervention group received a collection of information about ASD, PTSD, depression, pharmacological information, signs and symptoms that were clues for admission to a psychiatric center, education of family members, need for psychological consultations, need for emergency medical visits, and time and place that they can call to request home care visits. In cases of committing suicide, an emergency home visit and coordination for emergency hospitalization were performed.
The GHQ-28 was developed by Goldberg in 1978 to screen mental health disorders. It is a 4-point Likert scale questionnaire with 28 items and four dimensions, including somatic symptoms (items 1 - 7), psychological symptoms, anxiety and insomnia (items 8 - 14), social dysfunction (items 15 - 21), and depression (items 22 - 28). Scores for all dimensions of the questionnaire range from 0 to 21 with a total score of 0 - 84. The higher score represents poor mental health status. Cut-off point 23 is used to determine mental health issues. In addition, a score above 6 represents the disruption in related dimensions (23-25). In this study, the psychological health of survivors was measured by a valid and reliable Persian questionnaire. It was used together with a demographic information questionnaire. Concurrent validity and internal consistency reliability of the Persian version of the GHQ-28 were confirmed in previous studies (24, 26). In the present study, the internal consistency reliability of the questionnaire was satisfactory (α = 0.81).
All burn survivors in both groups responded to the questionnaires at three time points, baseline (T1: hospital discharge) and 3 (T2), and six months (T3) after the intervention. In these three time points, the psychological status of survivors was assessed. The psychological needs of survivors were identified based on the GHQ-28 scores and a short interview with them. The survivors received home visits based on their needs and the severity of their psychological manifestations. Communication between the first author and survivors was maintained by telephone calls. Home visits were continued for six months.
3.1. Ethical Considerations
The project and the ethical issues of the study were approved by the Research Ethics Committee of Shahid Beheshti University of Medical Sciences, Tehran, Iran (ID: SBMU2.Rec.1394.168). All the survivors signed an informed consent form. They were informed of voluntary participation in the study and could withdraw whenever they wished.
3.2. Data Analysis
The data were analyzed by descriptive and inferential statistics using the chi-square test, independent t-test, repeated measures analysis of variance (ANOVA), and Tukey’s post-hoc test by SPSS software (version 20; SPSS Inc, Chicago, IL, USA). The normal distribution of the outcome variables was evaluated by the Kolmogorov-Smirnov test.
4. Results
Tables 1 and 2 show a summary of the demographic characteristics and burn-related details of burn survivors.
| Variables | Control Group | Intervention Group | P-Value |
|---|---|---|---|
| Age (y) | 34.46 ± 12.81 | 39.13 ± 14 | 0.103 b |
| Gender | 0.414 c | ||
| Male | 16 (17.8) | 18 (20) | |
| Female | 29 (32.2) | (30)27 | |
| Marriage | 0.367 c | ||
| Single | 8 (8.9) | 11 (12.3) | |
| Married | 27 (30) | 30 (33.3) | |
| Divorced | 3 (3.3) | 1.1)) 1 | |
| Widow/Widower | 5 (5.6) | (1.1)1 | |
| Divorced after burn | 2 (2.2) | 2 (2.2) | |
| Employment | 0.312 c | ||
| Housekeeper | 23 (25.6) | 25 (27.8) | |
| Employed | 17 (18.9) | 12 (13.4) | |
| Unemployed | 5 (5.5) | 5 (5.5) | |
| Retired | 0 | (3.3) 3 | |
| Education | 0.091 c | ||
| Illiterate | 3 (3.3) | 7 (7.8) | |
| Elementary | 27 (30) | 18 (20) | |
| Diploma | 10 (11.1) | 16 (17.8) | |
| University | 5 (5.6) | 4 (4.4) | |
| Living place | 0.069 c | ||
| Urban area | 21 (23.3) | 29 (32.2) | |
| Rural area | 24 (26.7) | 16 (17.8) |
a Values are expressed as mean ± standard deviation or No. (%).
b Independent t-test
c Chi-square test
| Variables | Control Group | Intervention Group | P-Value |
|---|---|---|---|
| Burn severity (%) | 30.21 ± 12.21 | 31.31 ± 14.09 | 0.70 b |
| Burn degree | 0.094 c | ||
| II | 5 (5.6) | 7 (7.8) | |
| II, III | 39 (43.3) | 37 (41.1) | |
| III, IIII | 1 (1.1) | 1 (1.1) | |
| Burn areas | 0.137 c | ||
| Face and upper extremities | 17 (18.9) | 15 (16.7) | |
| Lower extremities | 4 (4.4) | 11 (12.2) | |
| Several parts | 24 (26.7) | 19 (21.1) | |
| Burn agent | 0.751 c | ||
| Scald | 4 (4.4) | 7 (7.8) | |
| Flame | 37 (41.2) | 35 (38.9) | |
| Chemical | 2 (2.2) | 1 (1.1) | |
| Electrical | 2 (2.2) | 2 (2.2) | |
| Attempt suicide | 0.250 c | ||
| Yes | 16 (17.8) | 11 (12.2) | |
| No | 29 (32.2) | 34 (37.8) | |
| Taking graft | 1 c | ||
| Yes | 36 (40) | 36 (40) | |
| No | 9 (10) | 9 (10) | |
| Burn place | 0.271 c | ||
| Home | 35 (38.9) | 36 (40) | |
| At work | 7 (7.8) | 3 (3.3) | |
| Out of home | 3 (3.3) | 6 (6.7) |
a Values are expressed as mean ± standard deviation or No. (%).
b Independent t-test
c Chi-square test
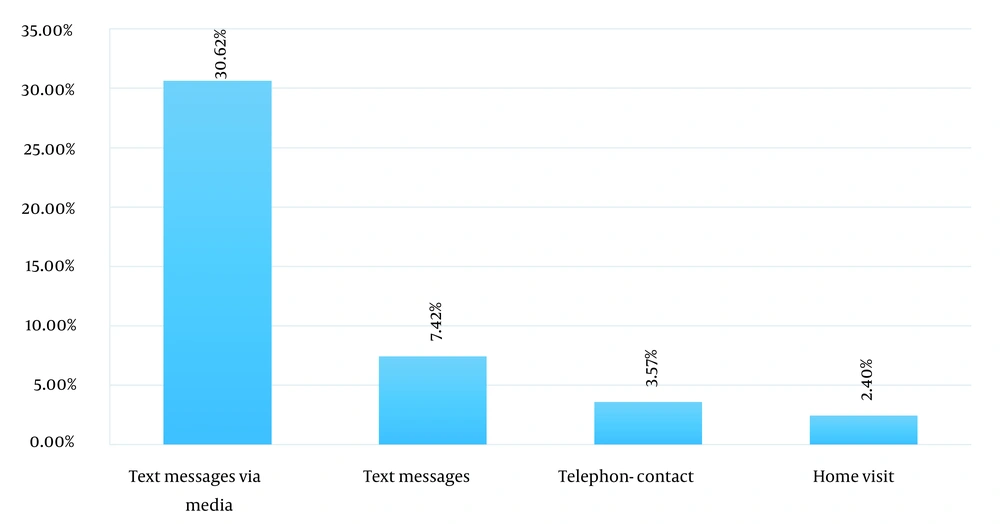
Figure 2 depicts the details of the communication between the nurse and burn survivors in the intervention group.
The results of the GHQ-28 showed that 65 (72.2%), 56 (62.2%), and 52 (57.8%) burn survivors at hospital discharge (T1), three months after hospital discharge (T2), and six months after hospital discharge (T3) had the mean scores higher than the cut-off point of the GHQ-28 (score 23), respectively. In addition, 61 (69.3%) and 73 (82%) survivors scored higher than six on the anxiety and social function subscales, respectively (Table 3).
| Variables | Intervention Group | Control Group | P-Value b |
|---|---|---|---|
| GHQ-28 | |||
| Discharge | 32.48 ± 15.83 | 32.29 ± 16.23 | 0.906 |
| 3 months | 25.15 ± 15.11 | 39.35 ± 14.59 | < 0.001 |
| 6 months | 19.37 ± 14.11 | 40.44 ± 15.59 | < 0.001 |
| GHQ subscales | |||
| Physical | |||
| Discharge | 7.33 ± 4.48 | 6.50 ± 3.87 | 0.186 |
| 3 months | 5.90 ± 4.62 | 8.90 ± 4.1 | 0.001 |
| 6 months | 4.6 ± 4.15 | 8.86 ± 3.99 | < 0.001 |
| Anxiety | |||
| Discharge | 9.86 ± 5.58 | 8.95 ± 4.76 | 0.363 |
| 3 months | 7.95 ± 5.19 | 9.60 ± 3.10 | < 0.001 |
| 6 months | 5.97 ± 4.51 | 11.68 ± 4.74 | < 0.001 |
| Social function | |||
| Discharge | 8.82 ± 4.12 | 8.77 ± 3.69 | 0.957 |
| 3 months | 7.5 ± 3.7 | 9.60 ± 3.10 | 0.006 |
| 6 months | 5.44 ± 3.58 | 9.93 ± 3.86 | < 0.001 |
| Depression | |||
| Discharge | 5.84 ± 5.41 | 7.93 ± 6.40 | 0.098 |
| 3 months | 4. 02 ± 4.64 | 8.17 ± 5.73 | < 0.001 |
| 6 months | 3.37 ± 4.04 | 9.15 ± 5.64 | < 0.001 |
Abbreviation: GHQ-28, General Health Questionnaire-28
a Values are expressed as mean ± standard deviation or No. (%).
b Independent t-test
Repeated measures ANOVA showed that the mean scores of the GHQ-28 were reduced over time in the intervention group compared to the controls. However, contradictory results were obtained in the control group. Tukey’s post-hoc test showed a difference in the mean scores of the GHQ-28 between the survivors of the two groups at 3 and 6 months after hospital discharge (P = 0.044).
There were significant differences between the intervention and control groups in the physical (P = 0.002) and anxiety (P < 0.001) subscales, respectively. Tukey’s post-hoc test showed a significant difference between the three time-point measurements in the physical subscale. In addition, Tukey’s post-hoc test showed that this difference was reported in the mean scores of the GHQ-28 between the survivors at 3 and 6 months after hospital discharge for the anxiety subscale (P = 0.019).
The results of repeated measures ANOVA on the social subscale showed significant differences between the intervention and control groups in the social subscale (P < 0.001). Tukey’s post-hoc test showed a significant difference between these results at 3- and 6-month measurements (P = 0.036). Furthermore, the results of repeated measures ANOVA for the depression subscale showed no significant differences between survivors within the groups in the depression subscale’s mean scores from hospital discharge to 6 months later (P = 0.235), and the interaction effect was not significant (P = 0.095). Nevertheless, there were significant differences between the intervention and control groups in the depression subscale (P < 0.001).
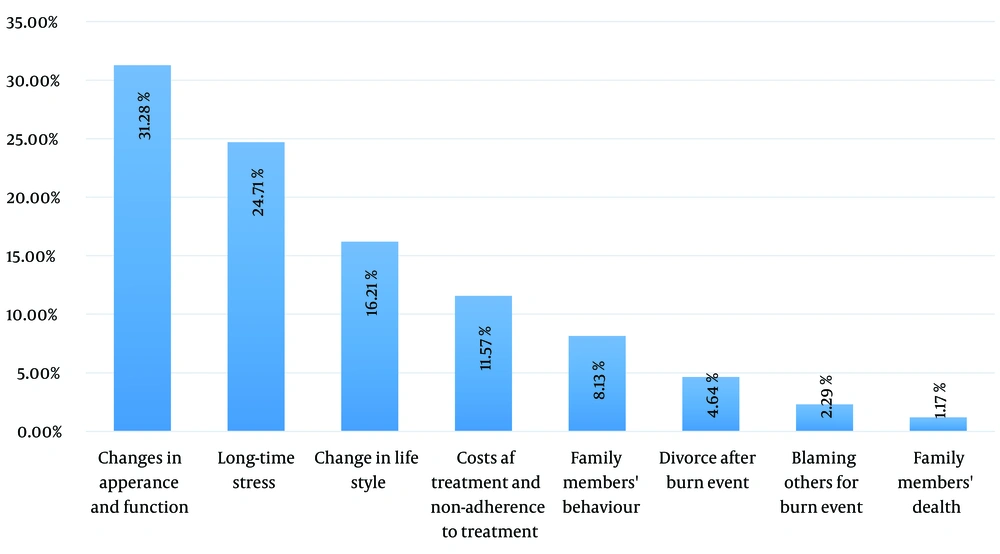
Figure 3 depicts the causes of mental health problems in burn survivors. Changes in appearance, including amputation of limbs, skin discoloration, and hypertrophic scars, and changes in lifestyle, including loss of job, changing in wearing style, quitting sport and exercise due to physical changes, and changes in sleep patterns. The mental health problems of most survivors were multifactorial.
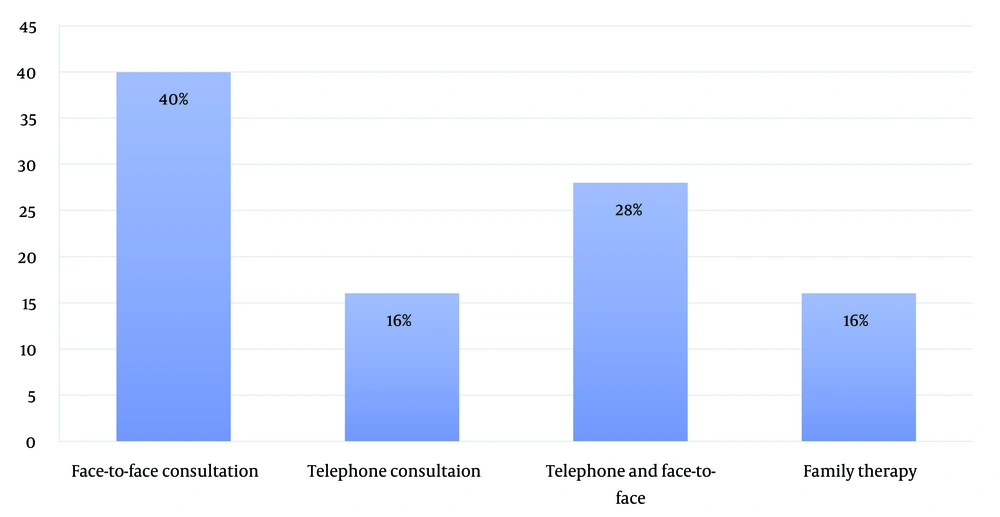
The results showed that 58.1% (n = 27) of burn survivors in the intervention group needed some kind of psychological support. Serious cases were two survivors (8%) referred to a psychiatrist at a hospital due to suicidal thoughts. There was one case (4%) with readmission to a psychiatric center and one case (4%) who did not accept being hospitalized. Figure 4 depicts the different types of interventions for the survivors in the intervention group.
The average number of home visits was 2.4 ± 2.53. The mean number of consultation meetings with psychologists and psychiatrists was 3.28 ± 3.38 and 0.97 ± 1.14, respectively. In addition, 11 survivors (24.4%) in the intervention group received pharmacological treatment.
5. Discussion
This RCT was carried out to determine the effectiveness of a home care plan in the mental health status of burn survivors six months after hospital discharge. The results showed that this home care plan after hospital discharge could improve the mental health status of burn survivors. The mean score of the GHQ-28 improved in the survivors of the intervention group 6 months after home care, compared to the control group. Goncalves et al. applied an educational program using telephone reinforcement for burn survivors in their study (19). The results showed improvement in anxiety symptoms and a reduction in the mean scores of the Impact of Event Scale in burn survivors in the intervention group at the 6-month follow-up. This education program started during hospitalization and continued for six months after hospital discharge (19). The study showed that the majority of burn survivors, more than 90%, suffered from stress symptoms in the form of ASD and PTSD. In addition, depression, sleep disorders, and nightmares were reported by the burn survivors (27).
The evidence showed that anxiety experienced by burn victims originates from ineffective pain management, the presence of itching, disruption in skin integrity, loss of function, hospitalization, and fear of the surrounding environment. Survivors’ personalities, lack of social support systems, and dependency have also been described as sources of anxiety after burn injuries (28). Therefore, burn survivors require the psychological and affective support that begins upon discharge from the hospital and continues throughout the rehabilitation phase (29).
Heydarikhayat et al. showed that post-hospital discharge follow-up is necessary to increase burn survivors’ mental health (30). Although, based on an earlier study by Karashchuk et al., psychiatric issues, substance abuse, and educational levels are several reasons why burn patients miss the follow-up program 6 to 12 months after burn events (31). Therefore, educational programs for knowledge, anxiety, and treatment adherence to pressure garments can alleviate the anxiety of burn survivors during the rehabilitation phase after burn injuries (19).
The results of a study by Cleary et al. indicated that mental health issues should be considered in the care and follow-up of burn survivors with severe burn injuries (7). There are several reasons why post-hospital discharge follow-up improves burn survivors’ mental health. One of the reasons is the improvement in their quality of life, which was observed in a study by Lotfi et al. (32). They run a post-discharge follow-up program for burn patients with family-based care. The aforementioned study showed that family-based follow-up is of great help to burn survivors as it was associated with improved quality of life for patients and their families (32).
The present study showed that although the mean mental health score improved in the intervention group 6 months after the follow-ups, some patients were still above the cut-off point score and needed more support and care. The evidence in this regard shows that the patient’s recovery in the physical affective dimensions, depression, anxiety, and pain needs a long time, and psychological and physical support after burning is essential (33). It can be explained that burn injuries lead to chronic burn outcomes and, therefore, long-term psychological distress (34).
5.1. Study Limitations
The high dropout rate of the samples due to their belief in herbal treatments for burn treatment was one of the main barriers to the study. Living in remote rural areas, difficult access to the city, and misunderstandings about psychiatric treatments led to resistance to the treatment.
5.2. Conclusions
The present study showed that a 6-month home care plan intervention could improve the mental health of burn survivors. Considering that at the end of the 6-month program, some survivors’ mental health was still not satisfactory, a home care plan with longer regular follow-ups is suggested for burn survivors in the healthcare system of Iran.