1. Background
Depression is a major public health concern that accounts for a high global disease burden; despite its high prevalence and partly due to the high costs of treatment, 90% of those affected do not receive the needed treatment (1, 2). The result of the Iranian Mental Health Survey that was conducted from 2010 to 2011 nationwide, showed that 12.7% of the general population are depressed (3), However, unlike many other countries in the region, Iran saw a decrease in the percentage of injury-related DALYs (Disability-adjusted life year) between 1990 and 2010 from 19% in 1990 to 15% in 2010 (4) Studies have increasingly shown that ethnic and cultural factors have a major impact on the presentation, diagnosis and assessment of the prevalence of major depression (5-7).
Presentations of major depression differ by setting and culture and are determined particularly by how bold somatic, emotional or psychological expressions are in that culture (8). In non-western countries, a diagnosis of depression might be morally unacceptable and its clinical manifestation may cause family, religious or social conflicts, as patients and their relatives tend not to consider it a biologically-determined disease and therefore do not seek professional help for it (9) and the recognition of depression becomes complicated.
The lack of culturally-appropriate instruments and the inadequate word-for-word translation of the available screening instruments are among the barriers of screening major depression in different cultures, especially in non-western countries. The mere reproduction of questionnaires from one language to another causes misleading and inaccurate interpretations (10, 11). Developing and improving screening tools for major depression in different settings, especially in non-western countries, is therefore critical. There is some instrument for screening or diagnostic of depression such as, the geriatric depression scale (GDS), Center for Epidemiological Studies Depression Scale, general health questionnaire, patient health questionnaire (PHQ), the Hamilton depression rating scale (HAM-D), Beck depression inventory, but they each have some limitation; for example GDS is designed to minimize the impact of somatic symptoms associated with aging and illness. Beck inventory is designed to assess the intensity of symptoms associated with psychoanalytic aspects of depression but for certain demographic groups and cultures, they have limited predictive power and validity because of the effects of translation from English to other languages, patients’ different interpretations of its emotional terms, and various cultural factors, such as perceptions of racial prejudice and a cultural group’s work ethic. These biases are observed with other screening tools used in primary care, including the Center for Epidemiological Studies Depression Scale, designed for diverse demographic groups, and the general health questionnaire and PHQ, which are used to identify short-term changes in mental health (12).
In Iran, too, depression is a dire health issue that needs to be systematically and continuously studied. In a survey of the twelve-month prevalence and severity of psychiatric disorders on people aged 15 - 64 years residing in Iran, 23.6% met the criteria for at least one DSM-IV psychiatric disorder. The group of anxiety disorders (15.6%) was the most prevalent group of disorders, followed by mood disorders (14.6%). The most prevalent DSM-IV disorder was major depressive disorder (12.7%), followed by generalized anxiety disorder (5.2%) and obsessive-compulsive disorder (5.1%); (13).
As a middle eastern country, Iran has used translations of western instruments to screen for depressive disorders. Although some of these translated and adapted questionnaires have demonstrated a suitable validity in various ethnic contexts, considering the differences in cultural values between Western cultures and others, it is still unclear whether a realistic picture has been drawn of this phenomenon in each setting (14) such as Iran.
When designing a tool or questionnaire, the items can be developed through a review of literature on the intended concept, clinical observations and interviews, qualitative research such as grounded theory studies, selections from items in other existing tools or a combination of all these methods (15).
2. Objectives
A local inventory was developed of the common symptoms of depression using a standardized translation of Beck’s depression inventory. This functional assessment tool was validated with the aim of improving the screening and evaluation of major depression in adults in three major ethnic groups in Iran. This paper presents the validity assessment of the inventory in the Fars ethnicity.
3. Materials and Methods
3.1. Design
The present study is part of a project aimed to design a tool for screening depression tailored to the Iranian culture in three ethnic groups, namely the Fars, Turk and Azerbaijani ethnicities. This report presents the results of the depression screening tool in the Persian ethnicity. The research was carried out using a combined (multi-stage) method in a qualitative and a quantitative stage.
3.2. First Stage: Tool Development
First, in order to investigate the concept and symptoms of depression, individual interviews were conducted in Tehran, Iran, with depressed patients, the patients’ relatives or friends and key informants (psychologists/psychiatrists). The inclusion criteria consisted of a self-declared Fars ethnicity, being born in Tehran and speaking Persian. The interviews continued until data saturation occurred and when no new categories of data could be extracted (16). A total of 20 male and female patients with depression entered the study and the samples were from all the different age groups in the 18 - 60 age range. After the content analysis, a list of the signs and symptoms of depression in the patients and their relatives/friends was prepared for the Fars ethnicity. The cases were then finalized after individual interviews with the key informants. In the next stage, a 28-item tool was designed based on the Likert scale in group discussions held among the research team. This tool examines additional domains over the 21-item Beck depression inventory (BDI) standardized in Iran (17), including beliefs and the use of the social networks or communication devices (cellphone, TV, etc.) (18).
3.3. Second Stage: Psychometric Assessment of the Tool
The face, content, criterion and construct validity (confirmatory factor analysis) of the designed tool were assessed in order to determine its validity. Since the purpose of the designed tool was to screen for depression in the society, sampling was carried out in the community.
3.3.1. Face Validity
Face validity was determined using both a qualitative and a quantitative method. To determine the qualitative face validity, ten members of the general public were selected using convenience sampling and face to face interviews were held to examine the level of difficulty of the items (difficulty understanding the statements and words). After modifying the items according to the points of view expressed by the public, a quantitative method (the impact score) was used to reduce the number of the items, eliminate inappropriate ones and determine the importance of each. In the impact score method, if the score was equal to or greater than 1.5, the item was deemed appropriate for the subsequent analysis and was kept in the tool.
3.3.2. Content Validity
The content validity was determined using a qualitative and a quantitative method. First, based on the judgments of knowledgeable experts in tool design and psychologists and psychiatrists, the content validity of the tool was assessed. In the qualitative content validity assessment, the researchers asked ten experts to express their opinions after carrying out a qualitative assessment of the tool in terms of grammar, wording, necessity, importance, item allocation and proper scoring (19). The quantitative content validity was determined using the content validity ratio (CVR) and the content validity index (CVI).To measure the CVR, the said ten experts were asked to rate each item based on a 3-point scale (from ‘necessary’ to ‘not necessary’). Then, if the number obtained from Lawshe’s table for determining the minimum value of the index was greater than 0.62, the item was deemed necessary and important for the tool at the statistical significance level of P < 0.05 (20). The CVI was evaluated based on the Waltz and Bausell CVI (19). The experts were asked to determine the relevance, simplicity and clarity of each item in the questionnaire. These three criteria were separately assessed by the experts for each item using a 4-point Likert scale. If the CVI of an item was greater than 0.79, the item was deemed appropriate, if the score was 0.75 - 0.80, the item was deemed questionable, and if the score was less than 0.70, the item was deemed unacceptable and had to be eliminated from the tool (21). In the next step, based on the mean CVI of all the questionnaire items, the mean scale-level content validity index/average(S-CVI/Ave) of the questionnaire was calculated. Polit et al. have recommended a score of 90% or higher for accepting the S-CVI/Ave (22).
3.3.3. Criterion and Construct Validity
To determine its criterion validity, this tool was compared with BDI. The correlation coefficient between the scores obtained from the two inventories was calculated as the predictive validity index of the said tool. In this study, the main concept used for designing the depression screening tool was Beck's inventory. Given that this concept was the basis of the development of this tool, a confirmatory factor analysis was used to determine the construct validity.
Determining the minimum sample size required to collect data on structural equation modeling is very important (23). Shah and Goldstein (24) and Schoenberg (25) have recommended a sample size of about 150 for confirmatory factor analysis. In this study, the data of 150 individuals from the general public was collected. Data were analyzed by Amos 24 and SPSS 16.
3.4. Third Stage: Reliability of the Tool
The reliability of the questionnaire was determined using the internal consistency method. Cronbach’s alpha is the most commonly-used method for examining the internal consistency of a tool (22). The sample size needed for determining the tool’s reliability was estimated as 50.
3.5. Ethical Code
The research project was approved with two codes of ethics -IR.USWR.REC.1395.104 from the University of Social Welfare and Rehabilitation Sciences, and Abzums.Rec.1394.48 from Alborz University of Medical Sciences.
3.6. Moral Considerations
The study objectives and obtained their written consent if they were willing to participate in the project data gathering was.
4. Results
This study was conducted on 150 individuals selected from the general public through convenience sampling with a mean age of 35.28 ± 12.38 (Table 1).
| Variable | F (%) |
|---|---|
| Gender | |
| Male | 67 (45) |
| Female | 82 (55) |
| Age | |
| < 20 | 11 (7.4) |
| 21 - 40 | 96 (64.4) |
| ≥ 41 | 42 (28.2) |
| Education | |
| Under diploma | 41 (27.5) |
| BS | 70 (47) |
| MS | 30 (20.1) |
| PhD | 8 (5.4) |
| Income | |
| Unpleasant | 28 (18.8) |
| Almost good | 78 (52.3) |
| Favorable | 43 (28.9) |
| Marriage status | |
| Permanent marriage | 101 (67.8) |
| Widow | 5 (3.4) |
| Divorce | 1 (0.7) |
| Single | 42 (28.2) |
| Family member | |
| One person | 6 (4) |
| Two person | 37 (24.8) |
| 3 - 4 person | 86 (57.7) |
| > 4 person | 20 (13.4) |
4.1. Face Validity
The findings of the qualitative validity assessment led to changes in the content of some of the items, and the impact score for all the items was between 1.8 and 5, and all the items were thus kept for performing the next stage.
4.2. Content Validity
In the qualitative content validity assessment, changes were made to the content of some of the items based on the experts’ opinions. In the quantitative content validity assessment, CVR was between 0.7 and 1 for all the items, and no item was thus eliminated from the next step. According to the CVI, the mean relevance, mean clarity, mean simplicity and S-CVI/Ave were 98.2 ± 1.9, 96.73 ± 0.70, 97.64 ± 0.61 and 97.09 ± 0.63, respectively. As a result, none of the items were removed and the questionnaire entered the next stage with 28 four-choice items.
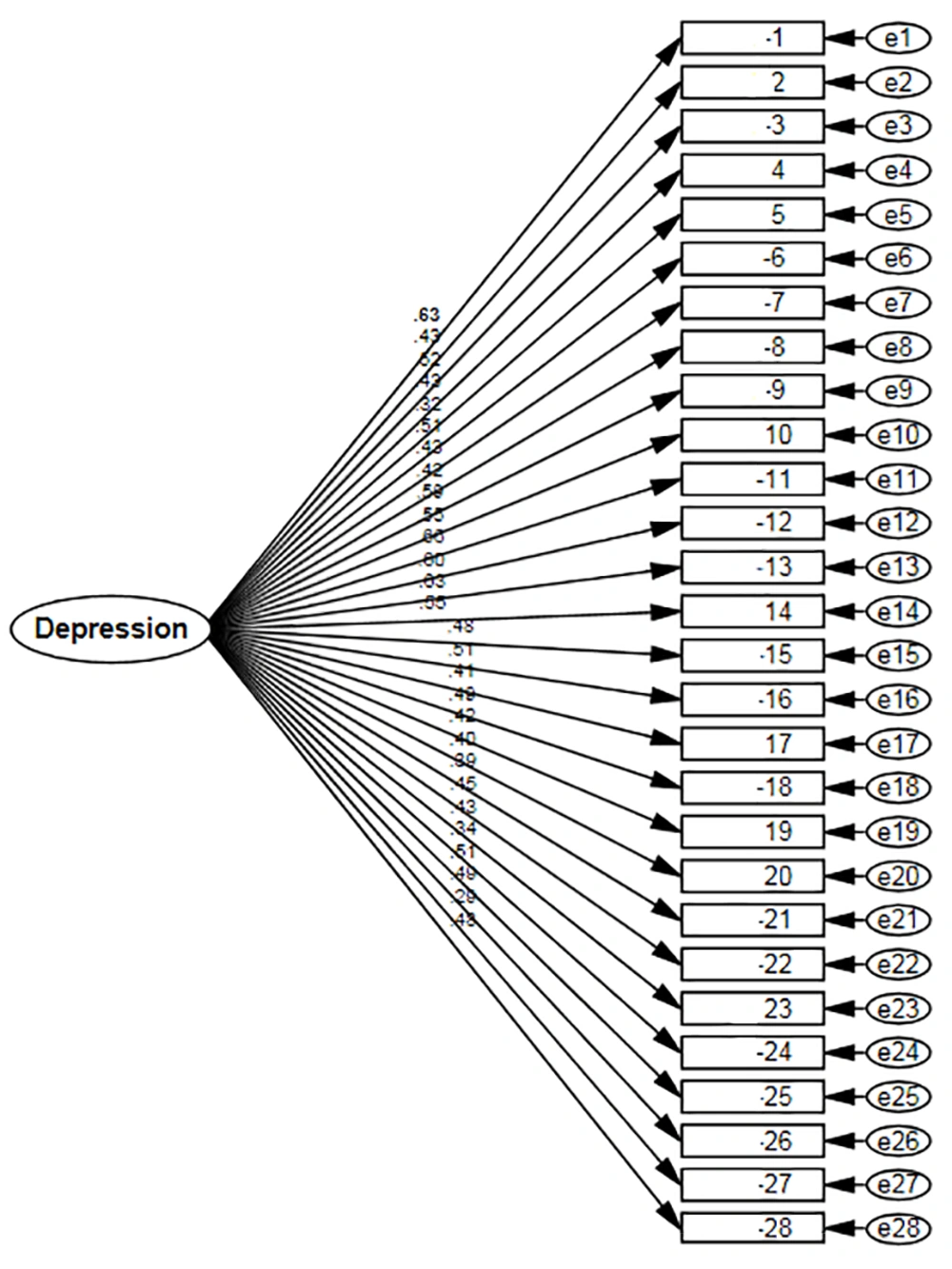
4.3. Construct Validity
As previously stated, single-factor confirmatory factor analysis was performed in order to confirm the homogeneity of the items in the questionnaire in terms of content and underlying dimensions. There are several goodness-of-fit indices for evaluating confirmatory factor analysis models. According to the model fit coefficients, the CMIN/DF was calculated as 1.93. In single-factor models, a CMIN/DF less than 3 indicates the favorability of the model (26). The closer are the NFI, CFI and GFI (0.70, 0.54 and 0.73 respectively) to 1 and the closer is RMSEA (0.79) to zero, the more favorable is the model, and the results obtained in this study show the relatively favorable fit of the model (Table 2).
| Model | CMIN/DF | RMR | GFI | NFI | CFI | RMSEA |
|---|---|---|---|---|---|---|
| 1.933 | 0.044 | 0.737 | 0.543 | 0.704 | 0.079 |
Based on the results of the confirmatory factor analysis, all the components were approved as factors used to screen for depression (Figure 1). Of these components, item 11 on decision-making power (0.661), item 1 on sadness (0.629) and item 13 on feeling guilty (0.626) had the highest regression weight or impact in terms of depression screening, and item 27 on the use of social networks had the lowest impact (0.292) (Table 3).
| Estimate | S.E. | C.R. | β | P Value | |
|---|---|---|---|---|---|
| 1 | 1.000 | 0.150 | 5.86 | 0.629 | *** |
| 2 | 0.581 | 0.122 | 4.755 | 0.433 | *** |
| 3 | 0.748 | 0.134 | 5.598 | 0.521 | *** |
| 4 | 0.585 | 0.125 | 4.690 | 0.427 | *** |
| 5 | 0.406 | 0.111 | 3.639 | 0.324 | *** |
| 6 | 0.710 | 0.130 | 5.457 | 0.506 | *** |
| 7 | 0.582 | 0.124 | 4.677 | 0.425 | *** |
| 8 | 0.733 | 0.158 | 4.624 | 0.420 | *** |
| 9 | 0.910 | 0.146 | 6.246 | 0.593 | *** |
| 10 | 1.020 | 0.173 | 5.908 | 0.555 | *** |
| 11 | 1.079 | 0.158 | 6.822 | 0.661 | *** |
| 12 | 0.906 | 0.143 | 6.319 | 0.601 | *** |
| 13 | 0.889 | 0.136 | 6.535 | 0.626 | *** |
| 14 | 0.850 | 0.145 | 5.867 | 0.550 | *** |
| 15 | 0.688 | 0.133 | 5.189 | 0.478 | *** |
| 16 | 0.331 | 0.060 | 5.506 | 0.511 | *** |
| 17 | 0.585 | 0.130 | 4.494 | 0.407 | *** |
| 18 | 0.755 | 0.143 | 5.262 | 0.485 | *** |
| 19 | 0.638 | 0.138 | 4.627 | 0.420 | *** |
| 20 | 0.905 | 0.203 | 4.462 | 0.404 | *** |
| 21 | 0.741 | 0.171 | 4.347 | 0.392 | *** |
| 22 | 0.698 | 0.141 | 4.940 | 0.452 | *** |
| 23 | 0.687 | 0.144 | 4.760 | 0.434 | *** |
| 24 | 0.441 | 0.117 | 3.775 | 0.337 | *** |
| 25 | 0.900 | 0.163 | 5.532 | 0.514 | *** |
| 26 | 0.676 | 0.127 | 5.339 | 0.493 | *** |
| 27 | 0.495 | 0.150 | 3.295 | 0.292 | *** |
| 28 | 0.981 | 0.188 | 5.213 | 0.480 | *** |
4.4. Reliability
Cronbach’s alpha was calculated as 0.88. An internal consistency coefficient that is 0.7 or higher is considered acceptable; therefore, the questionnaire was approved for large-scale research (27) (Table 4).
| Cronbach’s Alpha | No. of Items |
|---|---|
| 0.888 | 28 |
5. Discussion
The study of any subject requires a suitable tool for collecting the required information with utmost precision and the least amount of error (28). A tool designed in a particular country only reflects the culture of that country, and if used elsewhere, even if by way of a precise translation, it may be problematic due to the content not being a good fit (29).
The present study was conducted to assess the psychometric properties of a depression screening tool for the Fars ethnicity in Iran. The results of the study confirmed the validity and reliability of the tool. The face and content validity, simplicity and clarity of the items were also confirmed. The evidence on the “relevance” of the items in the CVI showed a significant degree of agreement between the experts (mean = 98.2%).
The results of the single-factor confirmatory factor analysis showed the good fit of the model. In this tool, sadness and feeling guilty were the variables with the greatest impact on depression screening. The review of literature showed no studies on the effects of each of the signs of depression on its incidence. There were also no studies that had investigated the cross-cultural and cross-language characteristics of depressed speech (30).
Nonetheless, recent studies suggest that, in addition to studying the mean scores, the emphasis in research has to be on the dynamic relationships between the signs and symptoms of depression (31). Sepehrmanesh and Moraveji found that despair and suicidal thoughts are the most common depression symptoms (32). Bringmann et al. reported the absence of pleasure and discontent as the most central components of the BDI (31). Ethnic differences likely affect the formation and expression of depression symptoms (33, 34). Therefore, knowing which item has the biggest impact on the score obtained in a screening tool can contribute to the effective use of the tool for a better and faster diagnosis by service providers.
In this study, Cronbach's alpha coefficient of the designed questionnaire showed a high internal consistency among the items, which confirms the reliability of the depression screening tool for the Fars ethnicity in Iran.
In depression, the way the affected person presents his symptoms can be fundamentally different from the symptoms with which the disease is manifested or presented. The symptoms expressed by the patient depend on his perception of the disease and judgment and responses to psychological symptoms, while the symptoms manifested by the patient are concerned with the psychiatrist’s judgement and the patient's condition during the clinical examination and interview (35). Unlike the BDI, the tool designed based on the findings of this qualitative study in the Fars ethnicity of Iran has 28 items that have been designed based on the descriptions of depression symptoms within the language and cultural context of Iran. In addition, this tool contains seven added items that are not measured in the BDI: Too much thinking, Beliefs, thinking of death, being sensitive, self-confidence, use of the social networks and communication devices. For instance, the use of social networks is one of the items that were mentioned in the interviews. Although it had the lowest impact in terms of screening for depression, the patients discussed it as a symptom of depression due to the changes that have recently taken place in societies. A strength of this tool was its use of the opinions of the patients and their relatives/friends, who were directly involved with the presenting symptoms (Supplementary File Appendix 1)
5.1. Limitations
The lack of studies on the effect of each depression symptom on depression screening limited the further comparison of the results with other studies.
5.2. Conclusions
This depression screening tool for the Fars ethnicity was designed based on the Fars ethnicity and the Iranian culture and appears to be an appropriate tool due to its good reliability, validity, simplicity and applicability in different situations. The researchers hope that this tool can be used by general practitioners or psychologists in health screening centers to help improve the timely diagnosis of depression, which is a prevalent but underdiagnosed disease in these centers. The designed tool is recommended to be used to evaluate the impact of interventions on depression treatment in psychologic intervention studies or in minimal surveys in Persian-speaking groups.