1. Background
Mental health disorders are one of the leading causes of disability worldwide. According to WHO, about 10 - 20% of children and adolescents worldwide are diagnosed with mental health disorders. An overview of recent studies suggested that anxiety disorders are the most prevalent mental health disorders among children and adolescents, followed by behavioral problems, mood disorders, and substance abuse, in sequence (1). In the US, out of 10,000 children and adolescents, 55 were admitted to psychiatric wards in 2012, accounting for 500,000 pediatric admissions due to behavioral disorders (2). Other recent epidemiological studies in Brazil and Lithuania suggested that the prevalence of psychiatric disorders was about 13% among children and adolescents (3, 4). On the other hand, epidemiological studies from 51 Asian countries in 2010, showed that although, some countries reported different prevalence of specific mental disorders, however, on the whole, the same range of 10 - 20 % of child and adolescent mental disorders were also suggested (5). Also, a meta-analysis in India demonstrated the rates of child and adolescent psychiatric disorders from 6.64% (in community-based studies) to 23% (in school-based studies); however, it was emphasized that the reporting system of pediatric psychiatric disorders in this country was defective (6).
In Iran, like other developing countries, such disseminated studies have been done in different cities, but the provided data cannot be generalized to the entire country. For example, one study on a randomized sample of 2,000 children and adolescents of the urban population of Tehran suggested a higher rate of psychiatric disorders than in other countries (7). However, this need can be met by an epidemiological study with a larger randomized sample from rural and urban areas of Iran.
With about two million people, Kermanshah Province is located in the west end of Iran. Although, according to the 2016 census, about 22% of this population is made up of children and adolescents, most investigators have studied psychiatric disorders over time and in clinical or school settings. For instance, one randomized study on 475 urban students from 17 primary and secondary schools of Kermanshah suggested that 57.5% of 7-15-year-old students had experienced at least a lifetime traumatic event, and on average, 30% of them had a variety of externalizing and internalizing problems (8). Therefore, considering the global prevalence of child psychiatric disorders and insufficient awareness of people regarding psychiatric disorders among children and adolescents, it may be possible that most child psychiatric disorders are not recognized or underestimated in Kermanshah. On the other hand, compared to other Iranian cities, socioeconomic status in Kermanshah has been under the adverse effects of many risk factors, like the vicinity to the Iraq War, lower level of literacy, higher incidence of addiction, and unemployment. As known, social, cultural, economic, and political changes of societies could affect people's psychological health. Besides, 38% of Iranian adults need clinical psychology services (9), and most psychiatric disorders root in childhood. Thus, we need to recognize the psychological problems of children by studies using large randomized samples and proper methodologies.
A large sample of Iranian children and adolescents living across Kermanshah was assessed in the current study. To do this research, we utilized the Iranian child and adolescent psychiatry (IRCAP) study in which a standardized research design has been used to assess the predictors of the leading psychiatric problems in children and adolescents. Thus, this study was designed to achieve two main aims: (1) investigating the prevalence of child and adolescent psychiatric disorders and determining their comorbidity patterns in Kermanshah and (2) indicating the frequency of child and adolescent psychiatric disorders according to demographic data (age, gender, education, and parents’ education and socioeconomic status) in urban and rural areas of Kermanshah.
2. Objectives:
This study aimed to assess the child and adolescent mental health status in the Kermanshah Province of Iran.
3. Method
3.1. Study Design
This is a community-based cross-sectional survey conducted as part of a national study of the epidemiology of psychiatric disorders in Iranian children and adolescents (IRCAP) (10). Data were collected under the supervision of two faculty members (HA and NJG) by nine instructed postgraduate male and female psychologists. After obtaining consent, examiners gathered the data in the screening and diagnostic phase, in which a random sample of children and their parent(s) or the primary care taker completed the demographic checklists and participated in semi-structured interviews for K-SADS-PL. For this purpose, the interviewers referred to the participants’ homes and held the semi-structured interviews for 30 - 40 min.
3.2. Criteria for Selecting the Participants
In this study, 993 urban and rural children and adolescents aged 6 - 18 years in Kermanshah City and its outskirts were selected by multistage cluster sampling method. For this purpose, 170 blocks were randomly selected according to postal codes, and then six cases were selected from each cluster head, with three cases from each gender in different age groups (6 - 9 years, 10 - 14 years, and 15 - 18 years). Inclusion criteria were living in Kermanshah City and its outskirts and being in the age range of 6 to 18 years. The exclusion criteria included the lack of willingness to participate and not being at home at visits (parent or child). Also, children and adolescents with severe physical illnesses were excluded.
3.3. Tools
Kiddie-SADS-Present and Lifetime version (K-SADS-PL): This is a semi-structured psychiatric interview based on the DSM-IV criteria. It contains five diagnostic groups: (1) Affective disorders including depression disorders (major depression and dysthymia), mania, and hypomania, (2) psychotic disorders, (3) anxiety disorders including social phobia, agoraphobia, specific phobia, obsessive-compulsive disorder, separation anxiety disorder, generalized anxiety disorder, panic disorder, and posttraumatic stress disorder, (4) disruptive behavioral disorders including ADHD, conduct disorder, and oppositional defiant disorder, and (5) substance abuse, tic disorders, eating disorders, and elimination disorders (enuresis/encopresis). The interview started with questions about demographics. Moreover, information about present complaints and prior psychiatric problems was also obtained (10). Ghanizadeh reported the reliability of the Persian version of the questionnaire to be 0.81 and the inter-rater reliability to be 0.69 using the test-retest method. The sensitivity and specificity of the Persian version were found to be high (11). In a study by Polanczyk et al., the kappa coefficients were 0.93 (P < 0.001) for affective disorders, 0.9 (P < 0.001) for anxiety disorders, and 0.94 (P < 0.001) for ADHD and disruptive behavior disorders. The present study assessed the interrater agreement for K-SADS (12).
Sociodemographic form: It was designed by the study principal investigators consisting of questions such as sex, age, residence place, parental history of hospitalization, education, vocation, etc.
3.4. Data Analysis
To describe the sample's demographic characteristics and psychiatric disorders, we used absolute and relative frequencies. The adjusted odds ratio (AOR) and 95% CI were employed to determine risk factors for any psychiatric disorder.
3.5. Ethical Considerations
Informed consent was obtained from children and adolescents. For participants younger than 15 years, the informed consent form was completed by their parents, and for participants aged 15 to 18 years, it was done by parents or the adolescents themselves. The information about children and adolescents and their families was kept confidential. If children or adolescents were diagnosed with a psychiatric disorder, the child and adolescent psychiatrist, who collaborated on the IRCAP project, were ready to treat them free of charge. The project was approved by the Ethics Committee of the National Institute for the Development of Medical Research, NIMAD (IR.NIMAD.REC.1395.001).
4. Results
Of 993 participants, 527 (53.1%) were females, and 856 (86.2%) were from urban areas. Also, 475 (47.8%) fathers and 447 (45%) mothers had a college diploma or higher academic degree. Besides, 636 (66.3%) fathers were working in the private sector, and 875 (89.7%) mothers were unemployed (housewives). The psychiatric frequency of their children was 11.3% and 12%, respectively (Table 1).
| Variables | Total, No. (%) | With a Disorder, No. (%) | CI (95%) |
|---|---|---|---|
| Sex | |||
| Boy | 466 (46.9) | 47 (10.1) | 7.7 - 13.2 |
| Girl | 527 (53.1) | 67 (12.7) | 10.1 - 15.8 |
| Age | |||
| 6 - 9 | 349 (35.1) | 35 (10) | 7.3 - 13.6 |
| 10 - 14 | 333 (33.5) | 43 (12.9) | 9.7 - 16.9 |
| 15 - 18 | 311 (31.3) | 36 (11.6) | 8.5 - 15.6 |
| Place of residence | |||
| Urban | 856 (86.2) | 94 (11) | 9.1 - 13.2 |
| Rural | 137 (13.8) | 20 (14.6) | 9.6 - 21.5 |
| Father's education | |||
| Illiterate | 63 (6.6) | 7 (11.1) | 5.5 - 21.2 |
| Primary school | 172 (18) | 20 (11.6) | 7.7 - 17.3 |
| Secondary or high school | 248 (25.9) | 33 (13.3) | 9.6 - 18.1 |
| Diploma | 271 (28.3) | 27 (10) | 6.9 - 14.1 |
| Bachelor | 155 (16.2) | 20 (12.9) | 8.5 - 19.1 |
| MSc or higher | 49 (5.1) | 5 (10.2) | 4.4 - 21.7 |
| Missing | 35 (-) | 2 (-) | |
| Mother's education | |||
| Illiterate | 89 (9.1) | 12 (13.5) | 7.9 - 22.1 |
| Primary school | 256 (26.3) | 36 (14.1) | 10.3 - 18.8 |
| Secondary or high school | 203 (20.8) | 20 (9.9) | 6.5 - 14.7 |
| Diploma | 287 (29.4) | 33 (11.5) | 8.3 - 15.7 |
| Bachelor | 111 (11.4) | 10 (9) | 5 - 15.8 |
| MSc or higher | 29 (3) | 3 (10.3) | 3.6 - 26.4 |
| Missing | 18 (-) | 0 (-) | |
| Father's job | |||
| Public sector | 270 (28.2) | 34 (12.6) | 9.1 - 17.1 |
| Private sector | 636 (66.3) | 72 (11.3) | 9.1 - 14 |
| Unemployed | 53 (5.5) | 6 (11.3) | 5.3 - 22.6 |
| Missing | 34 (-) | 2 (-) | |
| Mother's job | |||
| Public sector | 84 (8.6) | 7 (8.3) | 4.1 - 16.2 |
| Private sector | 16 (1.6) | 2 (12.5) | 3.5 - 36 |
| Unemployed (housewife) | 875 (89.7) | 105 (12) | 10 - 14.3 |
| Missing | 18 (-) | 0 (0) | |
| Total | 993 (100) | 114 (11.5) | 9.6 - 13.6 |
According to Table 2, the odds of total psychiatric disorders were higher among participants with female gender (AOR = 1.384; 95% CI = 0.923 - 2.075), a parental Bachelor’s degree (AOR = 1.681; 95% CI = 0.474 - 5.964), and maternal job in the private sector (AOR = 1.846; 95% CI = 0.314 - 10.867). However, none of the given scores were significant.
| Variables | OR (Crude) | CI (95%) | P-Value | OR (Adjusted) | CI (95%) | P-Value |
|---|---|---|---|---|---|---|
| Sex | ||||||
| Male | 1.00 reference | |||||
| Female | 1.298 | 0.874 - 1.929 | 0.196 | 1.384 | 0.923 - 2.075 | 0.116 |
| Age group | ||||||
| 6 - 9 | 1.00 reference | |||||
| 10 - 14 | 1.330 | 0.828 - 2.137 | 0.238 | 1.345 | 0.826 - 2.191 | 0.233 |
| 15 - 18 | 1.174 | 0.718 - 1.922 | 0.522 | 1.116 | 0.666 - 1.869 | 0.677 |
| Place of residence | ||||||
| Urban | 1.00 reference | |||||
| Rural | 1.386 | 0.824 - 2.332 | 0.219 | 1.352 | 0.771 - 2.371 | 0.293 |
| Father's education | ||||||
| Illiterate | 1.00 reference | |||||
| Primary school | 1.053 | 0.422 - 2.625 | 0.912 | 1.133 | 0.421 - 3.049 | 0.805 |
| High school | 1.228 | 0.516 - 2.922 | 0.643 | 1.593 | 0.578 - 4.394 | 0.368 |
| Diploma | 0.885 | 0.367 - 2.135 | 0.786 | 1.259 | 0.417 - 3.802 | 0.682 |
| Bachelor | 1.185 | 0.475 - 2.960 | 0.716 | 1.681 | 0.474 - 5.964 | 0.422 |
| MSc or higher | 0.909 | 0.270 - 3.060 | 0.878 | 1.341 | 0.269 - 6.678 | 0.720 |
| Mother's education | ||||||
| Illiterate | 1.00 reference | |||||
| Primary school | 1.050 | 0.520 - 2.121 | 0.892 | 1.008 | 0.442 - 2.300 | 0.985 |
| High school | 0.701 | 0.327 - 1.505 | 0.362 | 0.616 | 0.239 - 1.590 | 0.317 |
| Diploma | 0.834 | 0.411 - 1.693 | 0.615 | 0.757 | 0.287 - 1.997 | 0.574 |
| Bachelor | 0.635 | 0.261 - 1.547 | 0.318 | 0.548 | 0.154 - 1.945 | 0.352 |
| MSc or higher | 0.740 | 0.194 - 2.830 | 0.660 | 0.715 | 0.121 - 4.211 | 0.711 |
| Father's job | ||||||
| Public sector | 1.00 reference | |||||
| Private sector | 0.886 | 0.573 - 1.369 | 0.586 | 0.759 | 0.406 - 1.419 | 0.388 |
| Unemployed | 0.886 | 0.352 - 2.229 | 0.797 | 0.786 | 0.275 - 2.244 | 0.653 |
| Mother's job | ||||||
| Public sector | 1.00 reference | |||||
| Private sector | 1.571 | 0.295 - 8.360 | 0.596 | 1.846 | 0.314 - 10.867 | 0.498 |
| Unemployed (housewife) | 1.500 | 0.674 - 3.339 | 0.321 | 1.358 | 0.463 - 3.986 | 0.577 |
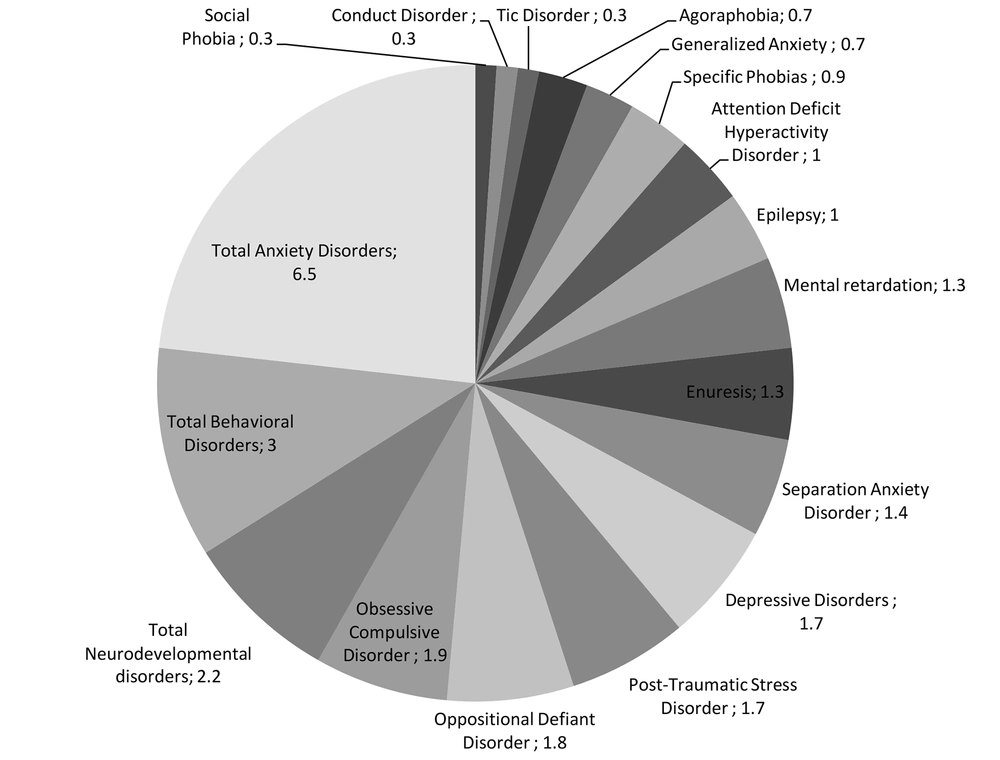
According to Table 3 and Figure 1, out of 993 participants in this study, 114 (11.5%) had at least a kind of psychiatric disorder. Anxiety disorders (n = 65, P = 6.5%; 95% CI = 5.2 - 8.3) were most prevalent, followed by behavioral disorders (n = 30; 95% CI = 2.1 - 4.3), neurodevelopmental disorders (n = 22; 95% CI = 1.1 - 2.7), and depressive disorders (n = 17). However, the most frequent disorder was obsessive-compulsive disorder (n = 19; 95% CI = 1.2 - 3) and the least one was social phobia (n = 3; 95% CI = 0.1 - 0.9). The most frequent comorbid diagnosis was mood disorder with 29.4%, 17.6%, and 11.8% among participants with anxiety disorders, behavioral disorders, and neurodevelopmental disorders, respectively (Table 4).
| Psychiatric Disorders | No. (%) | CI (95%) |
|---|---|---|
| Depressive disorders | 17 (1.7) | 1.1 - 2.7 |
| Anxiety disorders | ||
| Separation anxiety disorder | 14 (1.4) | 0.8 - 2.3 |
| Social phobia | 3 (0.3) | 0.1 - 0.9 |
| Specific phobias | 9 (0.9) | 0.5 - 1.7 |
| Agoraphobia | 7 (0.7) | 0.3 - 1.4 |
| Generalized anxiety | 7 (0.7) | 0.3 - 1.4 |
| Obsessive-compulsive disorder | 19 (1.9) | 1.2 - 3 |
| Post-traumatic stress disorder | 17 (1.7) | 1.1 - 2.7 |
| Total anxiety disorders | 65 (6.5) | 5.2 - 8.3 |
| Behavioral disorders | ||
| Attention deficit hyperactivity disorder | 10 (1) | 0.6 - 1.8 |
| Oppositional defiant disorder | 18 (1.8) | 1.1 - 2.8 |
| Conduct disorder | 3 (0.3) | 0.1 - 0.9 |
| Tic disorder | 3 (0.3) | 0.1 - 0.9 |
| Total behavioral disorders | 30 (3) | 2.1 - 4.3 |
| Neurodevelopmental disorders | ||
| Mental retardation | 13 (1.3) | 0.8 - 2.2 |
| Epilepsy | 10 (1) | 0.6 - 1.8 |
| Total neurodevelopmental disorders | 22 (2.2) | 1.5 - 3.3 |
| Enuresis | 13 (1.3) | 0.8 - 2.2 |
| Total psychiatric disorders | 114 (11.5) | 9.6 - 13.6 |
| Main Disorder | Comorbid | ||||
|---|---|---|---|---|---|
| Mood Disorders | Anxiety Disorders | Behavioral Disorders | Neurodevelopmental Disorders* | Elimination Disorders | |
| Mood disorders | 5 (29.4) | 3 (17.6) | 2 (11.8) | 0 | |
| Anxiety disorders | 5 (7.7) | 3 (4.6) | 2 (3.1) | 1 (1.5) | |
| Behavioral disorders | 3 (10) | 3 (10) | 2 (6.7) | 0 | |
| Neurodevelopmental disorders | 2 (9.1) | 2 (9.1) | 2 (9.1) | 1 (4.5) | |
| Elimination disorders | 0 | 1 (7.7) | 0 | 1 (7.7) | |
a Values are expressed as No. (%).
5. Discussion
This study was part of a national survey of the epidemiology of psychiatric disorders in Iranian children and adolescents (IRCAP)10, conducted in Kermanshah and its outskirts to evaluate a representative randomized sample of 993 children aged 6-18 years. Using the Kiddie-SADS-Present and Lifetime version (K-SADS-PL), we found that, overall, 11.5% of them had at least one kind of psychiatric disorder according to DSM-IV, which corresponds well with the global prevalence of 10 - 20% of psychiatric disorders among children and adolescents (1, 5). However, there are also some contradictory results; for instance, the study of Molavi et al. reported a much higher total prevalence of child and adolescent psychiatric disorders in the Ardabil Province of Iran (13). On the other hand, considering the national census of Iran in 2017, the number of persons below 18 years was about 400,000 in Kermanshah Province (14). Therefore, the 11.5% prevalence rate means that out of 400,000 children and adolescents, 46,000 suffer from at least one form of psychiatric disorder in a given time. However, considering the limited psychiatry, psychology, and wellbeing resources in Kermanshah, accompanied by the slow development of pediatric psychiatry, this considerable present and the future problem cannot be dealt with very easily.
Several children and family characteristics were examined to explore the relationship between them and the prevalence of psychiatric disorders. The results have suggested a non-significantly higher prevalence of psychiatric disorders among children whose mothers or fathers were unemployed or had a job in the private sector (considering their low payment and inconstant job) or had a lower educational level. It might suggest the effect of socioeconomic status on psychiatric disorders among children. This result is in line with other studies showing that parents' lower education and financial condition are critical family risk factors for poorer mental health in children (4). On the other hand, although in Kermanshah, mothers of participants suffering from mental disorders were primarily housewives, this result is inconsistent with Mohammadi et al. at the national level across Iran (IRCAP), who found that mothers' job could not predict depression disorder among children (15). Besides, the non-significant relationship of some participants’ demographic characteristics with disorders including female gender, age of 10 - 14, and urban residence is consistent with Mohammadi et al. (15), indicating that these characteristics could be the predictors of depression among children. It is also in line with the meta-analysis of La Maison et al. that indicated a higher frequency of psychiatric disorders among adolescents (3).
The psychopathological rate of psychiatric disorders was comparable with other similar investigations worldwide, as the most prevalent psychiatric disorder was anxiety disorders, followed by behavioral, neurodevelopmental, and depressive disorders (1). The most common anxiety diagnosis in this sample was obsessive-compulsive disorder, and the least prevalent one was a social phobia.
The most common comorbidity pattern was a mood disorder with anxiety disorder, behavioral and neurodevelopmental disorders, in sequence, comparable with prior research that assessed psychiatric disorders in early adolescents in Brazil (3). Interestingly, it can be said that anxiety and depression are related to behavioral disorders as the chief complaints of disordered children. Likewise, Ranoyen et al. found that anxiety and depression are the most common comorbid disorders (16).
The strengths of this study were recruiting a population-based sample and conducting face-to-face interviews with a large randomized sample of urban and rural children and adolescents. Using a validated diagnostic instrument of semi-structured interview (K-SADS-PL) in Iran applied by trained MA psychologists was another advantage that made the data more generalizable. Another essential point was interviewing parents or guardians and children or adolescents simultaneously, making the data more reliable. Some limitations may have influenced the interpretation of the results. Although participants were all in school-age and getting reports from teachers could definitely reveal significant symptoms not recognized by mothers, they were not involved in gathering stages. Long interviews that mainly were done with low educated mothers included another limitation. The K-SADS-PL instrument was based on DSM-IV, so we could not employ the criteria of DSM-V, which has the most internationally accepted criteria.
5.1. Conclusions
This study indicated that about 11.5% of 6-18-year-old children and adolescents in Kermanshah suffer from a kind of mental health disorder. In addition to mental health care, a combination of health and social services should be available for young people, resulting in protection against known risk factors such as low socioeconomic status of families and prevention from hospitalization (17). Yet, as pediatric psychiatric disorders have not gotten appropriate attention from health politicians and by considering social, mental, and physical needs of the youth experiencing mental distress, easily accessible mental health and evidence-based psychological services are strongly recommended to deal with this critical present and future problem.