1. Background
Pregnancy is one of the most sensitive and complex periods in a woman’s life. Although childbearing is considered an important and pleasant event for a couple and a family, however, it can be a critical time for women (1). Pregnancy leads to the physiological changes in body’s reproductive and endocrine systems and causes changes in appearance that are beyond the woman’s control. Therefore make her physically and mentally vulnerable (2, 3). Any factor that causes physical and mental tension and also the loss of balance is considered as a stressor (4). Stressful situations has been created a range of emotional reactions, from happiness (when an event is difficult, but manageable) to anxiety, anger, discouragement and depression (5). High and low levels of anger, tension, rage, pathological anxiety and depression are the most common psychological disorders which occurred in almost 50% of pregnancies (6). Psychological disorders during pregnancy can lead to undesirable outcomes such as miscarriage, preterm childbirth, still birth, intrauterine growth retardation, a low Apgar score, gestational hypertension and preeclampsia, impaired infant development and postpartum depression as well as can affect on the child’s health for the long term (7-13). Moreover, any psychological disorder during pregnancy leads to other psychological disorders and the combination of these disorders can worse the conditions for mother and neonate (14). Therefore mental health during pregnancy is a highly important issue.
The process of pregnancy can cause emotional instability in women (15). Some of factors such as being young, being a victim of sexual abuse, the unwanted pregnancy, not having a spouse, unprepared for pregnancy and delivery and having symptoms of depression, a history of psychiatric disorders can adversely effect on maternal mental health (16). Socioeconomic deprivation also affects the mental health of pregnant women and is associated with the increased risk of psychological diseases, especially depression during pregnancy (17, 18). In developing countries, a poor socioeconomic status is considered as a risk factor for psychological disorders in women (19), as 16% of pregnant women in low as and less than of average income countries are affected by one of the two most common psychological disorders during pregnancy, specifically depression and anxiety. However in high-income countries this rate has been reported as 10% (20, 21). In high income countries, factors such as unemployment, unfavorable neighborhood conditions, low income and social prestige, poor socioeconomic status and income inequalities are associated with adverse psychological consequences (22-25), which is suggested that the socioeconomic factors can effect on mental health. Psychological disorders during pregnancy are reportedly exacerbated by socioeconomic factors such as poverty, poor education, sexual violence and limiting or lack of access to health services and goods (26). Also some of risk factors for psychological disorders have a greater prevalence among poor socioeconomic groups, including poor coping styles when faced with major life events, exposure to stress and a poor social support system (27). In contrast, a favorable socioeconomic status does not only involve in material wealth, but also leads to a significant increasing in independence and encourages the individual to further control and overcome with life problems and subsequently protects person against depression (28).
Many studies have demonstrated the relationship between socioeconomic deprivation and psychological disorders in general public. Nevertheless, few studies have addressed the issue in pregnancy, and even then, they have conflicting results. In recent years, researchers come to further focus on this relationship and its causes.
Socioeconomic index is consisted of three factors, namely education, occupation, and income. This determinant can directly and indirectly effect on people well-being and health by providing vital skills and knowledge (29). Most studies have been conducted in this field which are addressed the relationship between these factors and pregnancy problems (9, 12, 17, 18). However, no study was found on direct and indirect effects of these factors, or their path analysis on women’s mental health. This indicates the necessity in order to conduct such studies.
2. Objectives
The present study is conducted to investigate the relationship between household socioeconomic status and mental health in Tehran on pregnant women from 2014 to 2015 by a path analysis.
3. Materials and Methods
In order to carry out this cross-sectional study, one public hospital was selected from each of the four geographical districts of Tehran (North, South, East and West) in 2014 - 2015.
In terms of sample size, various studies have considered 5 - 10 samples per item sufficient, and some have regarded even three samples per item sufficient (30). In the present study, there were 40 items in questionnaires, and given the above, 10 samples were selected per item making required sample size 400 people.
A total of 400 pregnant women in 24th to 32nd weeks of gestation were randomly selected from the hospitals and were briefed on the study objectives before they submitted their consent forms. Those meeting the study inclusion criteria was completed the demographic and obstetrics questionnaire, the household socioeconomic status (HSES) scale, the perceived social support scale (PSSS) and the short-form version of the depression, anxiety, and stress scales (DASS-21). The study inclusion criteria consisted of being in the 24th to 32nd weeks of gestation, having a singleton pregnancy and no history of known medical disorders before or during the pregnancy. The questionnaires were completed with the help of a trained team of individuals and exclusion criteria were; cancel continue research and filling incomplete form.
3.1. Data Collection Tools
3.1.1. The Demographic and Obstetrics Questionnaire
This questionnaire were consisted of items such as; mother’s age (date of birth), marital status, ethnicity, place of residence (city or village), maternal education, spouse’s level of education (paternal education), gravidity and parity, the number of miscarriages and stillbirths, the pregnancy being intended by the couple, history of previous or current pregnancy complications and floor space per person.
The participants’ socioeconomic status was assessed using a pre-designed questionnaire with items on the maternal education, paternal education, floor space per person, price per square meter of land and amenities. The correlation between these factors and the total score was calculated as 0.87 in this study. A factor analysis was used in order to calculate the total standardized score by measuring the summary index for all the participants, and its consistency with the conventional summary index which was verified using the Kappa test. In accordance with the agreement between the scores, the cut-off score that created a bivariate variable and divided the households into a group with favorable and a group with unfavorable socioeconomic statuses which was calculated as 16 using the summary index (31).
3.1.2. The DASS-21
This 21-item scale was measured symptoms of depression, anxiety and stress with seven items per each and scores the responses based on a 4-point Likert scale (0: Did not apply to me at all; 1: Applied to me to some degree, or some of the time; 2: Applied to me to a considerable degree, or a good part of time; 3: Applied to me very much, or most of the time). In each section of scale, a score of 1 - 7 indicates mild, 8 - 14 indicates moderate and 15 - 21 indicates severe depression, anxiety or stress. This scale was first introduced by Lovibond in 1995 and was used on a large sample of people. The scale has also been used in many domestic and foreign studies which its validity and reliability have been confirmed (32-35). Sahebi et al. reported the correlation coefficient of this scale as 0.7 using Beck’s test, as 0.67 by Zung anxiety test and as 0.49 using the perceived stress test; they also measured its internal consistency with a Cronbach’s alpha of 0.77 for the depression subscale, 0.79 for the anxiety subscale and 0.78 for the stress subscale (35).
3.2. The Multidimensional Social Support Scale
This 12-item scale was developed by Zimet et al. in 1988 in order to measure the perceptions of social support from three sources: friends, family and significant other. The scale is scored based on a 7-point Likert scale (from 1: very strongly disagree to 7: very strongly agree) and gets a minimum score of 12 and a maximum of 84. The scores of 13 - 48 indicate a poor social support, 49 - 68 indicate moderate support and 69 - 84 indicate high social support. The reliability of the scale has been reported in various studies with a Cronbach’s alpha of 0.86, and its validity has also been estimated as favorable using the content validity method (36-39).
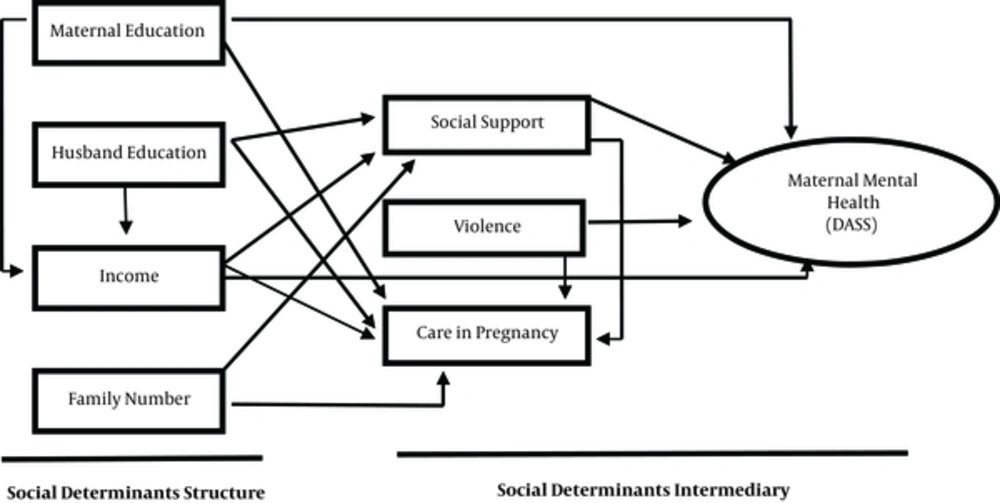
The present study has been developed a conceptual model (Figure 1) in order to determine the concurrent relationships between pregnancy depression, anxiety and stress and socioeconomic status plus perceived social support, and fit of the model and the percent variance were assessed using a path analysis. A path analysis is an extension of regression analysis that is able to show direct as well as, indirect and total effects of each variable on the dependent variable and to interpret rationally the correlations between them. As for the fit index of model in a path analysis, the chi-square to degree of freedom ratio (X2/df) is preferred to be less than 3, although some consider values of 4 or even 5 as indicator of a good fit. Other fit indices including the normed fit index (NFI), the comparative fit index (CFI) and the goodness of fit index (GFI), which are considered favorable if their value is above 0.9 (30). A root mean square error of approximation (RMSEA) value equal to or less than 0.05 also indicates a good fit, although values of up to 0.08 are also acceptable, and some sources even consider values of up to 0.11 as acceptable (40). Standardized Root Mean Square Residual (SRMR) values less than 0.08 indicates an acceptable fit (41).
The obtained data were analyzed using SPSS-22 and Lisrel-8.8 by a path analysis. In this study descriptive tests such as mean, standard deviation, Pearson’s correlation, and path analysis were used. This study was approved by the ethics committee of Shahid Beheshti University of Medical Sciences, Tehran, Iran (SBMU.REC.1393.633)
4. Results
According to obtained results, the mean age of the participating women and their spouses was 28.46 ± 4.97 and 32.73 ± 5.32 years, respectively, and the majority of both women (78%) and the men (81.3%) had a high school diploma (Table 1).
| Variable | F (%) |
|---|---|
| Mother education | |
| Illiterate | 4 (0.9) |
| Diploma | 351 (78) |
| BS | 91 (20.2) |
| ≥ MS | 4 (0.9) |
| Husband education | |
| Illiterate | 2 (0.4) |
| Diploma | 366 (81.3) |
| BS | 71 (15.8) |
| ≥ MS | 11 (2.4) |
| Family number | |
| 2 | 390 (86.7) |
| 3 - 5 | 54 (12) |
| 6 - 8 | 6 (1.3) |
| Care in pregnancy | |
| < 10 | 4 (0.9) |
| 11 - 20 | 202 (44.9) |
| ≥ 21 | 244 (54.2) |
Distribution of Demographic Pregnant Women Participating in the Study
In order to carry out the path analysis, bivariate analyses were first performed to determine the correlations between the variables. As shown in Table 2, household size had the highest direct correlation with the DASS score and social support the highest indirect correlation with this score.
| Variables | Social Support | DASS= Stress +Depression + Anxiety | Age Women | Age Husband | Education Women | Education Men | Family Number | Income, Toman | Violence | Care in Pregnancy |
|---|---|---|---|---|---|---|---|---|---|---|
| Social support | 1 | |||||||||
| DASS= Stress +depression + anxiety | -0.328b | 1 | ||||||||
| Age women | 0.079 | -0.008 | 1 | |||||||
| Age husband | 0.048 | 0.027 | 0.751b | 1 | ||||||
| Education women | 0.189b | -0.181b | -0.069 | -0.092 | 1 | |||||
| Education men | 0.218b | -0.191b | 0.019 | -0.016 | 0.584b | 1 | ||||
| Family number | -0.111c | 0.218b | 0.258b | 0.295b | -0.313b | -0.210b | 1 | |||
| Income, Toman | 0.156b | -0.146b | 0.102c | 0.100c | 0.255b | 0.184b | -0.084 | 1 | ||
| Violence | -0.053 | 0.056 | -0.065 | -0.044 | -0.121c | -0.071 | 0.049 | -0.004 | 1 | |
| Care in pregnancy | -0.046 | 0.029 | 0.073 | 0.121c | -0.024 | -0.018 | 0.010 | 0.028 | -0.114c | 1 |
Correlationsa Among Socioeconomic Factors and Maternal Mental Health
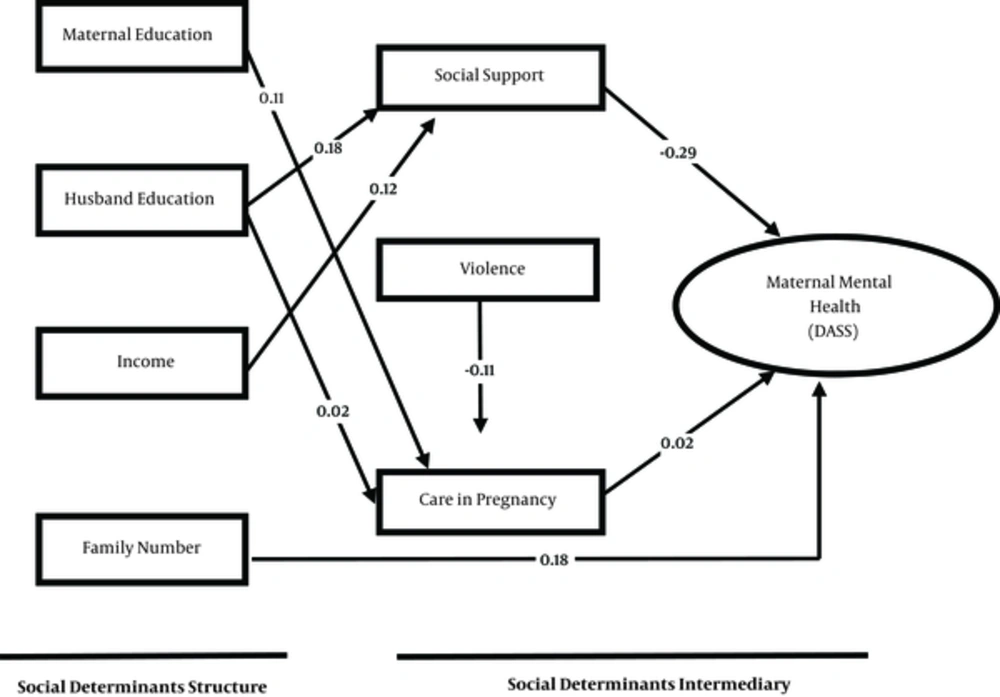
The effect of variables including maternal education, paternal education, income, household size, violence, pregnancy care and social support was examined on maternal mental health through the path analysis (Figure 2). According to the path diagram, among the direct paths, social support had the greatest negative effect (B = -0.29) and household size the greatest positive effect on maternal mental health as per the DASS score (B = 0.18); among the indirect paths, paternal education and income had the greatest negative effects (B = -0.053; B = -0.035) and maternal education the greatest positive effect (B = 0.002) on maternal mental health (Table 3).
| Predictor Variables | Effects | Model Coefficients | T Value | R2 | ||
|---|---|---|---|---|---|---|
| Direct | Indirect | Total | ||||
| Mother education | - | 0.002 | 0.002 | - | - | 0.15 |
| Father education | - | -0.053 | -0.053 | - | - | |
| Family number | 0.18 | - | 0.18 | 1.96 | 4.03 | |
| Violence | - | -.002 | -0.002 | - | - | |
| Social support | -0.29 | - | -0.29 | -0.26 | 6.61 | |
| Income | - | -0.035 | -0.035 | - | - | |
| Care in pregnancy | 0.02 | - | 0.02 | 0.19 | 2.01 | |
Path Coefficients for Social-Economic-Demographic Factors on Maternal Mental Health
According to the model, among the direct paths, mothers with an unfavorable social support experience a poor mental health, and among the indirect paths, paternal education affects social support and pregnancy care and thus exerts the greatest negative effect on maternal mental health. In other words, the lower is paternal education; the greater are the unfavorable conditions the mother experiences in terms of receiving pregnancy care and social support. Nevertheless, maternal education positively effects on maternal mental health by affecting how much pregnancy care the mother receives. That is, the higher is maternal education, the better is the pregnancy care she receives and the higher is her mental health.
The fit indices of the model showed a favorable status, a high goodness of fit and the existence of rational relationships between the variables based on the conceptual model. As a result, there are no significant differences between the fitted model and the conceptual model (Table 4).
| Model Index | Value |
|---|---|
| X2 | 4.05 |
| df | 3 |
| P Value | 0.25 |
| GFI | 0.98 |
| CFI | 0.97 |
| RMSEA | 0.02 |
Goodness of Fit Indices for the Model, N = 589
5. Discussion
According to the results of path analysis model, among the variables with a direct effect on maternal mental health, social support had the greatest negative effect. This finding was consistent with the results of many other studies like Giurgescu et al. and Morikawa et al., they found that mothers who enjoyed adequate social support during pregnancy experienced have a healthier pregnancy compared to those who did not have (42, 43). Family and husband support during pregnancy may effect on maternal and fetal health through unmeasured mediators such as improved maternal health behaviors (refraining from smoking and drinking, etc.), the communication of health information and receiving early pregnancy care or through biological mechanisms such as reducing stress reactions, improved healthier lifestyle and appropriate pregnancy weight gain. This factor also appears to act as a buffer that protects the mothers against stressful events and allows them in order to enjoy a greater mental health and well-being (44-46).
Among the variables with an indirect effect on maternal mental health, paternal education and income had the greatest negative effect. According to the results, paternal education adversely affects this aspect of maternal health by effecting on social support and pregnancy care. In other words, women who had spouses with lower education experienced less favorable conditions in terms of receiving pregnancy care and social support compared to others. Low paternal education is a major contributing factor of domestic violence. Some studies like Alizadeh et al. (2012) have shown that women with less-educated spouses experience less favorable conditions in terms of financial and emotional support, which affects their mental health (47). Education is important for career prospects and future income and is considered the most fundamental economic indicator. Education also is facilitated accession to information and health-promoting resources through improving knowledge and life skills. When the spouse is unemployed for any reason, he undergoes great financial difficulty and stress and not only can he no longer properly perform his responsibilities, but his wife inevitably experiences similar conditions and is affected by his unemployment too (48, 49). Income was another factor that had the greatest indirect negative effect on maternal health. The income is a major employment-related determinant of physical and mental health. Income inequalities can lead to health inequities. There are various explanations for the mechanism of the effect of income inequities on health. This variable can have personal effects through financial, structural, behavioral and lifestyle factors. For instance, malnutrition and its subsequent infectious diseases are caused by income inequities. In addition to the other effects of a poor income, these two consequences increase maternal, neonatal and infant mortality in and by themselves. In other words, these three types of death are poverty-induced. From the psychosocial perspective, the neuroendocrine mechanism explains the relationship between income inequities and health, as socioeconomic differences affect the individual’s perception of the social hierarchy and thereby her health. The difference between the rich and the poor diminishes social cohesion and trust. The perception of belonging to the lower social class generates negative emotions such as shame and distrust and leads to poor health behaviors through affecting the neuroendocrine system and encouraging unhealthy behaviors induced by stress, such as smoking (50).
Maternal education affects maternal mental health by affecting the amount and form of pregnancy care received. The mother’s length of education is an important determinant of pregnancy outcomes. This variable affects maternal physical and mental health by way of the educational experiences and skills gathered through years of education, such as how to improve the home environment, nutrition, self-care and cognitive simulations and take proper advantage of health investments and resources (51, 52).
5.1. Conclusion
According to the present study results, socioeconomic factors (education, occupation, and income) and social support directly or indirectly (or both) are effected on maternal mental health. Material deprivations and socioeconomic inequities such as malnutrition, poverty and poor housing status and income have major effects on the incidence of chronic diseases and mental health by way of psychosocial factors, lifestyle habits and physiopathological changes. Counseling interventions aimed at improving maternal mental health through alleviating socioeconomic damages and increasing family support are recommended. Consideration the pregnancy per se causes emotional instability in women, knowledge of factors affecting or exacerbating these disorders is highly important.
5.2. Limitations
Limitation of the study is due to financial constraints and limitation of time, this study was conducted by Cross-sectional design and the majority of study samples were home makers. Therefore, further studies on working women and the effect of employment on mental status during pregnancy are recommended.