1. Background
Although there is no general agreement on the definition of fear of childbirth, this fear is characterized by worries about childbirth assessed by several specific scales (1). Fear of childbirth has a global prevalence of 20% - 25% and 14% for its severe type (2). Based on another study, this fear is between 8% and 30% around the world, and this heterogeneity depends on its different definitions and the tools used to measure (3). The prevalence rate of anxiety during pregnancy is 35% greater compared with women of the same reproductive age (19.8%) (4). A pregnant woman’s emotional and physical experience makes unique and context-specific anxiety, which can evoke an effective reaction (5).
However, negative emotions and maternal fear of childbirth have usually been ignored, since it can lead to tension in communication, reduced thinking power, and lack of ability and perception of the mother during pregnancy (6). Mother’s uncertainty about her ability for vaginal delivery and fear of perineal tearing (7) or the fear of the unknown (8) lead to choosing elective cesarean (9). Women staying longer in the hospital pay more that is estimated to be 38% more than treatment costs and imposes huge costs on health systems in countries (10). The need for epidural anesthesia and postpartum trauma has increased, whereas the rate of mother breastfeeding has reduced (11). Also, there is a strong correlation between postpartum depression and fear of childbirth (12). Moreover, women’s satisfaction is dependent on health care staff through labor, which can be used in hospital policies as feedback to improve maternity-related systems (13). Labor and childbirth experiences are complex and multidimensional (14). Women’s birth satisfaction may have an impact on their health and children as an experience that can be achieved sooner or later. For example, postpartum depression, post-traumatic stress disorder, lack of ability to resume sexual activity, increased number of cesarean cases, negative attitude towards the baby, and lack of compatibility with the maternal role are the factors affecting childbirth dissatisfaction (15). According to the aforementioned reports, childbirth fear and anxiety are undeniable facts, and there is a need for interventions for reducing these discomforts (16). Snoezelen room with multiple sensory stimulations has been considered worldwide as a complementary therapy (17). There is a lack of comprehensive research in this field, but a qualitative study showed that women experienced subjective relaxation, comfort, and a sense of control in labor using a Snoezelen delivery room (18). The results of a systematic review showed that environmental interventions had a lower effect on women’s ability to cope with pain and their personal relationships (19). The results of another systematic review revealed the evidence on how birthing environments affect outcomes of labor and birth is incomplete (20). The term “Snoezelen room” was used by Hulsegge and Verheule in 1975 with the combination of two Dutch words describing a process of controlling all sensory systems in a safe environment, i.e., Dozelen and Snoezel that means seeking out and relaxing with creating satisfaction in people (21, 22). Snoezelen room is a multidimensional stimulus environment useful for relaxation and distracting mind through an increase in the secretion of endorphins from the brain and an increase in the capacity of individuals to adapt pain (23). Aromatherapy (24) is one of the ways, which is used in the Snoezelen room, as the olfactory system has a direct and immediate effect on the nervous system (25). Music therapy during childbirth can reduce anxiety, pain, and postpartum depression and increase satisfaction, which it is also another component of a Snoezelen room (26) and improves physical symptoms, hormones, and stabilizes vital signs via stimulating the brain, increasing endorphins, inhibiting sensory-environmental receptors. Light music can make a slow breathing rate, reduce heart rate, and relax the body (27, 28). It seems that the use of complementary medicine in most Iranian pregnant women is acceptable, and like many other countries, such as Germany, over 50.7% of women use it during pregnancy (29). Also, massage therapy and yoga are some of the most common methods for pregnant women in Australia and the United States (30). For example, Hatha yoga training in pregnancy reduced the fear of childbirth (31).
There are other non-pharmacological methods for improving the emotional and psychological aspects of pain, leading to appropriate decisions and feelings of strength and self-control in the progress of the delivery. Using interventions as non-pharmacological methods (32), like acupuncture, which has no impact on maternal or fetal outcomes (33), hypnosis that had been effective in soothing fear and pain and the increasing sense of control during labor (34), water childbirth (35), which has not approved in a systematic review because of bias (36), yoga (37, 38), and physical and emotional support compatible with pain (39) have been effective accordingly. However, studies on the effect of the Snoezelen room on childbirth are scarce, and whether a Snoezelen room can make women comfortable during labor and birth should be assessed. Consequently, it can be considered as a complementary method to reduce pain, the anxiety of birth, and making the childbirth process a pleasant and enjoyable event. As a complementary method, it can reduce severe anxiety and fear and decrease the tendency for selective cesarean (40). Therefore, non‐drug interventions should be selected for pain relief and better satisfaction with childbirth (41), especially in nulliparous women who had not previous negative birth experience.
2. Objectives
The aim of the present study was the efficacy of the Snoezelen room on fear, anxiety, and satisfaction of childbirth.
3. Methods
3.1. Design
This randomized controlled trial was conducted on 130 nulliparous women in the Akbar Abadi Hospital affiliated to Iran University of Medical Sciences from February 2016 to March 2017.
3.2. Sample
The sample size was 65 individuals in each group, considering a 95% confidence level, a test power of 80%, and based on the Namazi study (d = 0.79) with the attrition probability of 10%.
In this study, inclusion criteria were the absence of known medical conditions, such as migraine, epilepsy, asthma, and allergies, mothers’ age of from 18 to 35 years, gestational age of 37 to 42 weeks, estimated embryo weights of 2500 to 3500 g per examination or according to the sonography results, head and pelvic fitness based on vaginal examination, cephalic examination according to the vaginal examination, no stressed events in the previous 6 months, dilatation of 3 - 4 cm at the beginning of the study, low-risk pregnancy, and normal pattern of fetal heart rate. The exclusion criterion included the need for an emergency cesarean for medical reasons, according to a doctor and midwife suggestions during the study.
3.3. Data and Measures
Data gathering was performed by a demographic characteristics form, and three questionnaires, including the Harman’s Childbirth Attitude questionnaire (CAQ), reviewed by Lowe (42) and translated and validated in Iran (43), the Mackey Childbirth Satisfaction Rating scale (MCSRS), and Visual Analogue scale (VAS). CAQ has 14 items scoring on a four-point scale Likert (not at all, very low, moderate, and high). Score 14 shows the minimum, and 56 shows maximum fear, and it has no cutoff point. VAS was used to measure childbirth anxiety, and women’s satisfaction was measured with the MCSRS that has 34 items (32) and has been translated and validated in Iran, and by eliminating two items for cultural reasons, finally, it includes 32 items (44). In this questionnaire, nine items are related to the mother, nine items are about a midwife, eight items concern the doctor, three items regard the baby, and three items are related to the satisfaction of the childbirth, which ultimately will show the total satisfaction. It is scored on a five-point scale from totally disagree (score one) to totally agree (score five).
3.4. Procedures
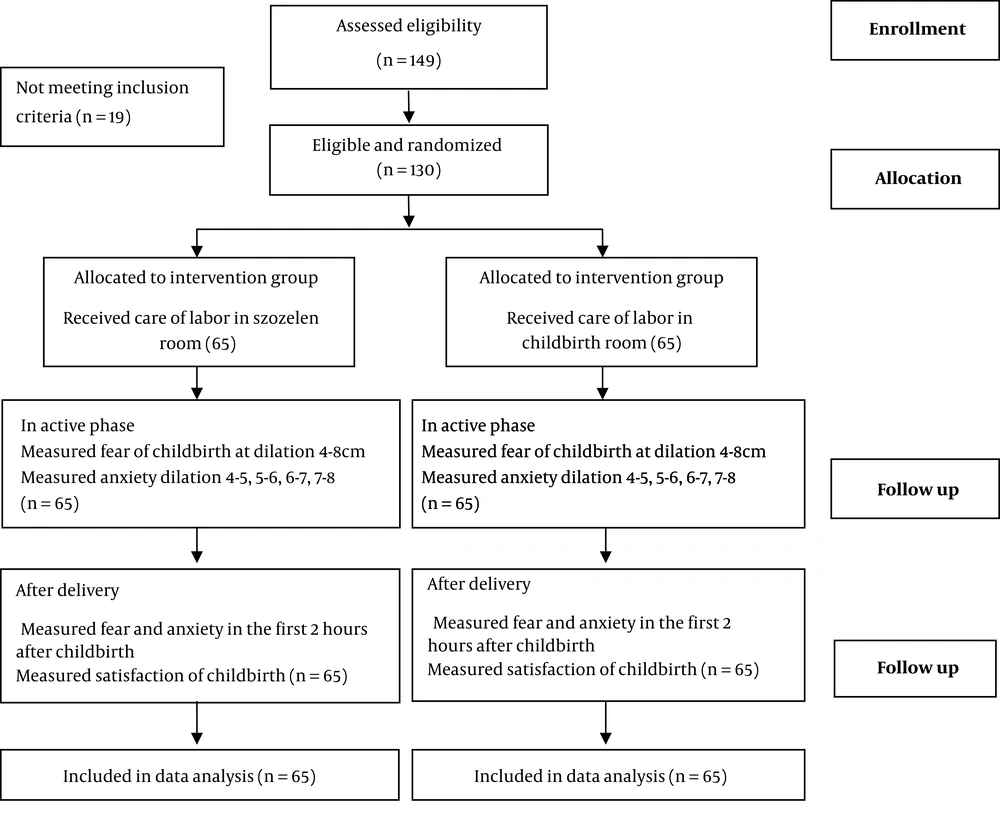
After being approved by the Ethics Committee of Iran University of Medical Sciences, registering a proposal at the Iranian Center for Clinical Trials, and obtaining a permit from the vice-chancellor for research and offering to hospital authorities, a Snoezelen room was designed using an aquarium, a projector, which played optical shapes, playing light music, and essential aroma. The research objective was explained to the eligible women, and then their written informed consent was obtained. The sampling method was using a convenience sample. One hundred thirty women by random allocation assigned to the two groups. They were randomly assigned to the groups using four blocks of six units in the opaque envelopes in the hospital admission by the statistical consultant for maintaining confidentiality. This study was not blinded. Before entering the eligible women to the childbirth rooms their fear of childbirth was evaluated by CAQ and their anxiety by the VAS. Then, the questionnaire assessing fear was refilled at 4 to 8 cm dilatation, and anxiety was also measured by the VAS per hour at 4 to 5 cm, 5 to 6 cm, 6 to 7 cm, and 7 to 8 cm dilatation. Next, after confirming the mother’s vital signs during the first 2 h after childbirth, the CAQ and VAS were completed, followed by filling out the MCSRS when the mother was discharged from the hospital (Figure 1). The collected data were analyzed using independent t-test, repeated measures analysis of variance (rANOVA), and Chi-square and Bonferroni tests by SPSS version 16.
4. Results
The mean age of women in the intervention group was 26.69 ± 5.11, and in the control group was 28.25 ± 4.24 years. The average number of years of education was 12 ± 2.70 and 12 ± 3.20 in the intervention and control groups, respectively. Other demographic variables are shown in Table 1.
| Variable | Interventional Group | Control Group | Results |
|---|---|---|---|
| Employment | χ2 = 0.652; df = 0.2; P = 0.72 | ||
| Housewife | 50 (76.9) | 46 (70.8) | |
| Employed | 15 (23.1) | 19 (29.2) | |
| Previous hospitalization for labor | χ2 = 0.4; df = 0.2; P = 0.53 | ||
| Yes | 26 (40) | 18 (27.7) | |
| No | 39 (60) | 47 (72.3) | |
| Age at pregnancy | 38.4 ± 0.92 | 38.1 ± 0.82 | t = 1.94; df = 128; P = 0.62 |
| Neonate’s weight | 2948.35 ± 180 | 2890.20 ± 220/ | t = 1.54; df = 128; P = 0.126 |
aValues are expressed as No. (%) or mean ± SD.
The results revealed the mean score of fear at baseline was 43.38 ± 3.56 in the intervention group and 41.33 ± 2.89 in the control group. The mean of fear during the active phase and after childbirth decreased than the baseline in the intervention group, which was statistically different between the intervention and control groups (-6.4 ± 28.91 and 2.09 ± 6.24, respectively). The mean score of fear in the postpartum was also significantly lower in the interventional group than baseline (37.11 ± 3.47), whereas, in the control group, the postpartum fear score was higher than before entering to the childbirth room (44.33 ± 2.99) (Table 2).
| Time | Group | ||||||
|---|---|---|---|---|---|---|---|
| Interventional Group (N = 65) | Control Group (N = 65) | Results | Comparison | Interventional Group (N = 65) | Control Group (N = 65) | Results | |
| At baseline | 43.38 ± 3.56 | 41.33 ± 2.89 | t = 2.71; df = 128; P = 0.07 | In active phase-at baseline | -2.37 ± 5.50 | 2.46 ± 7.74 | t = 4.106; df = 128; P < 0.001 |
| In active phase | 41.01 ± 2.01 | 43.79 ± 2.51 | t = 3.39; df = 128; P < 0.001 | At postpartum-in active phase | -3.90 ± 4.50 | 0.54 ± 1.66 | t = 3.93; df = 128; P < 0.001 |
| After delivery | 37.11 ± 3.47 | 44.33 ± 2.99 | t = 10.57; df = 128; P < 0.001 | At postpartum-at baseline | -6.28 ± 4.91 | 2.09 ± 6.24 | t = 8.50; df = 128; P < 0.001 |
aValues are expressed as mean ± SD.
bUsing repeated measures analysis of variance and Bonferroni test.
The mean score of anxiety was measured before, during, and after childbirth by t-test. The results showed that the mean score of anxiety decreased in the intervention group in the active phase than the baseline and also than the control group. Besides, the mean score of mothers’ anxiety in the intervention group decreased after delivery, whereas in the control group, it was higher than before entering the room (4.62 ± 3.1 and 8.87 ± 5.1, respectively) (Table 3).
| Cervix Dilation | Interventional Group (N = 65) | Control Group (N = 65) | Results |
|---|---|---|---|
| At baseline | 8.06 ± 1.34 | 7.49 ± 1.61 | t = 2.18; df = 128; P = 0.031 |
| In active phase | 7.87 ± 0.74 | 8.04 ± 1.18 | t = 1.98; df = 128; P = 0.09 |
| After delivery | 4.62 ± 3.1 | 8.87 ± 5.1 | t = 8.31; df = 128; P < 0.001 |
aValues are expressed as mean ± SD.
Also, the mean score of anxiety in different dilations of the cervix was assessed by the rANOVA and Bonferroni test. The mean score of anxiety at 4 - 5 cm was similar to 5 - 6 cm of dilation, but there was a significant difference at 6 - 7 and 7 - 8 cm of dilation between the two groups (Table 4).
| Anxiety at Different Cervix Dilations, cm | Interventional Group (N = 65) | Control Group (N = 65) | Results |
|---|---|---|---|
| 4 - 5 | 8.4 ± 1.43 | 7.95 ± 1.77 | t = 1.578; df = 128; P = 0.117 |
| 5 - 6 | 7.95 ± 0.94 | 8 ± 1.73 | t = 0.189; df = 128; P = 0.85 |
| 6 - 7 | 5.49 ± 1.03 | 7.92 ± 1.41 | t = 1.99; df = 128; P = 0.04 |
| 7 - 8 | 6.64 ± 1.20 | 8.29 ± 1.4 | t = 2.82; df = 128; P = 0.006 |
aValues are expressed as mean ± SD.
The total mean score of birth satisfaction was 163.19 ± 10.15 in the intervention group and 74.71 ± 6.04 in the control group. Also, 58.5% of mothers in the Snoezelen room reported satisfaction and were very pleased with the experience of childbirth, whereas 67.7% of mothers were dissatisfied with the childbirth in the control group. The mean score of satisfaction with childbirth was higher after delivery (23.82 ± 1.03) in the intervention group than the control group (11.32 ± 0.73). Mothers’ satisfaction with their neonate was 49/79 ± 10.42 in the intervention and 63.72 ± 17.58 in the control group. More than half of women (52.3%) were very satisfied with their postpartum in the interventional group than the control group (16.9%) (Table 5).
| Mother’s Satisfaction | Groups | Values | Results |
|---|---|---|---|
| The mother with herself | Interventional group | 41.82 ± 2.73 | t = 15.41; df = 128; P < 0.001 |
| Control group | 20.18 ± 5.26 | ||
| With the baby | Interventional group | 22.12 ± 1.42 | t = 6.23; df = 128; P < 0.001 |
| Control group | 10.2 ± 1.04 | ||
| With the midwife | Interventional group | 42.61 ± 3.37 | t = 4.32; df = 128; P < 0.001 |
| Control group | 15.26 ± 1.57 | ||
| With the physician | Interventional group | 32.82 ± 6.47 | t = 7.46; df = 128; P < 0.001 |
| Control group | 17.82 ± 3.73 | ||
| Childbirth satisfaction | Interventional group | 23.82 ± 1.03 | t = 11.52; df = 128; P < 0.001 |
| Control group | 11.32 ± 0.73 | ||
| Overall satisfaction | Interventional group | 163.19 ± 10.15 | t = 7.83; df = 128; P < 0.001 |
| Control group | 74.71 ± 6.04 |
aValues are expressed as mean ± SD.
5. Discussion
In the intervention group, the mean score of fear was different during and after the intervention than baseline (P < 0.001). Also, the mean score during the active phase was less than before entering the room and after the childbirth in the intervention group. Moreover, the mean score of fear of childbirth during the active phase was statistically significant in both groups (P < 0.001). The mean score of fear in postpartum showed a significant difference between the two groups (P < 0.001). This study did not categorize the severity of fear of nulliparous women as mild, moderate, or severe, but in one study, it was reported that in the general population of pregnant women, 6% suffered from severe fear and about 2.4% had a phobia of childbirth that led to choosing a cesarean section (45). Fear of childbirth is one of the main reasons to request a cesarean section (46-48). The study (2017) suggested that prenatal mindfulness training reduced fear and pain of childbirth and prevented from postpartum depression symptoms; mindfulness was assumed as the primary mechanism for coping with the fear of labor (49). The effectiveness of hypnotherapy on the fear of childbirth has been shown to increase maternal confidence in her abilities and improve mother mental health resulting in pain relief (50).
The mean score of anxiety was lower at ≥ 6 cm of dilation in the intervention than the control group (P < 0.001). Consistent with this study, it has shown that the mean score of anxiety through inhaling Geranium during childbirth in the intervention group was lower than the control group (51). Using lavender in aromatherapy had reduced the anxiety of childbirth by affecting pain perception at intrapartum (52). Also, an intervention showed that mindfulness-based stress reduction reduced anxiety in pregnancy (53). Several physical interventions have been used during pregnancy to prevent mother’s anxiety, including autogenic training, biofeedback, hypnosis, prayer, yoga, meditation, and auto-suggestion, which act via psychological techniques and self-hypnosis (54).
The total mean score of birth satisfaction was significantly different between the two groups (P < 0.001). The results of another study showed that music did not significantly affect the anxiety between the two groups, but there was a significant difference in mothers’ satisfaction between the two groups following listening to music (30 min) 5 days before childbirth and 2 days after birth, and it could create a good childbirth experience (55). In our study, integrating the ways to distract the mind effectively reduced anxiety. Childbirth satisfaction in cases who had vaginal delivery was higher than women with cesarean section, and women who had decided to deliver at home or at the birth center had higher satisfaction than those who were at the hospital (56). In our study, women in the Snoezelen room could walk and select their positions, perhaps they had the feeling of being at home, and they were nulliparous. It was similar to the birth room in the hospital described by other women in their families or friends as the control group had experienced. There was a significant difference between the two groups in the score of satisfaction with the newborn (P < 0.001). The satisfaction score of the labor agents, the midwife, and the physician was also significantly different between the two groups (P < 0.001). The result of another study showed that the Belgian women’s satisfaction with birth was higher than Dutch women, however, home birth was prevalent among Dutch women and Belgian women who had home birth experience reported a higher level satisfaction than those experiencing hospital childbirth (57).
In line with the present study, a study revealed that women who used the Snoezelen room for breastfeeding in the early hours of birth showed an increase in their self-confidence and comfortable sleep in their babies, and despite the pain in their breasts, they started easier breastfeeding (18).
In the current study, women’s satisfaction with a midwife was significantly different between the two groups (P < 0.001). It seems that women had a good experience with the midwives and doctors. It has shown that the scores of satisfaction with care by nurses in women who gave birth at home were higher than in hospitals (58). In this regard, a study concluded using the effect of face-to-face counseling and Internet based on cognitive-behavioral therapy on birth satisfaction, showed a decrease of from 34% to 12% in cesarean rate than using the Internet (24% to 20%), but there was not a significant difference in birth satisfaction level in the groups (59). In the present study, it seems that the presence of a midwife in the Snoezelen room to support women through the labor and birth process as a face-to-face form led to a decrease in fear of birth and cesarean.
It has revealed that providing a good level of care had a meaningful relationship with the positive comments of women via keeping the mother at a private place, answering mother’s questions, receiving information, and mental support by the personnel (60). In our study, midwives and physicians were able to provide women’s satisfaction through the mental support of the mothers and by appropriate responses to them.
5.1. Conclusions
Our results showed that fear of childbirth in the intervention group was lower than the control group during labor and after childbirth.
Also, the mother’s anxiety in the active phase at 6 to 7 cm and 7 to 8 cm of dilatations were lower and showed significant differences in two groups. The mean score of postpartum anxiety also had a significant difference between the two groups, as the mean score of anxiety in the control group after delivery was higher than the intervention group.
The mean score of overall satisfaction with postpartum care was different in the intervention than the control group and was higher in the intervention group. Mothers’ satisfaction scores with their babies, themselves, and birth agents, namely the midwife and the physician, were higher in the Snoezelen room.
The limitation of this study was including previous information regarding childbirth by our nulliparous women who participated in a birth preparation class.