1. Introduction
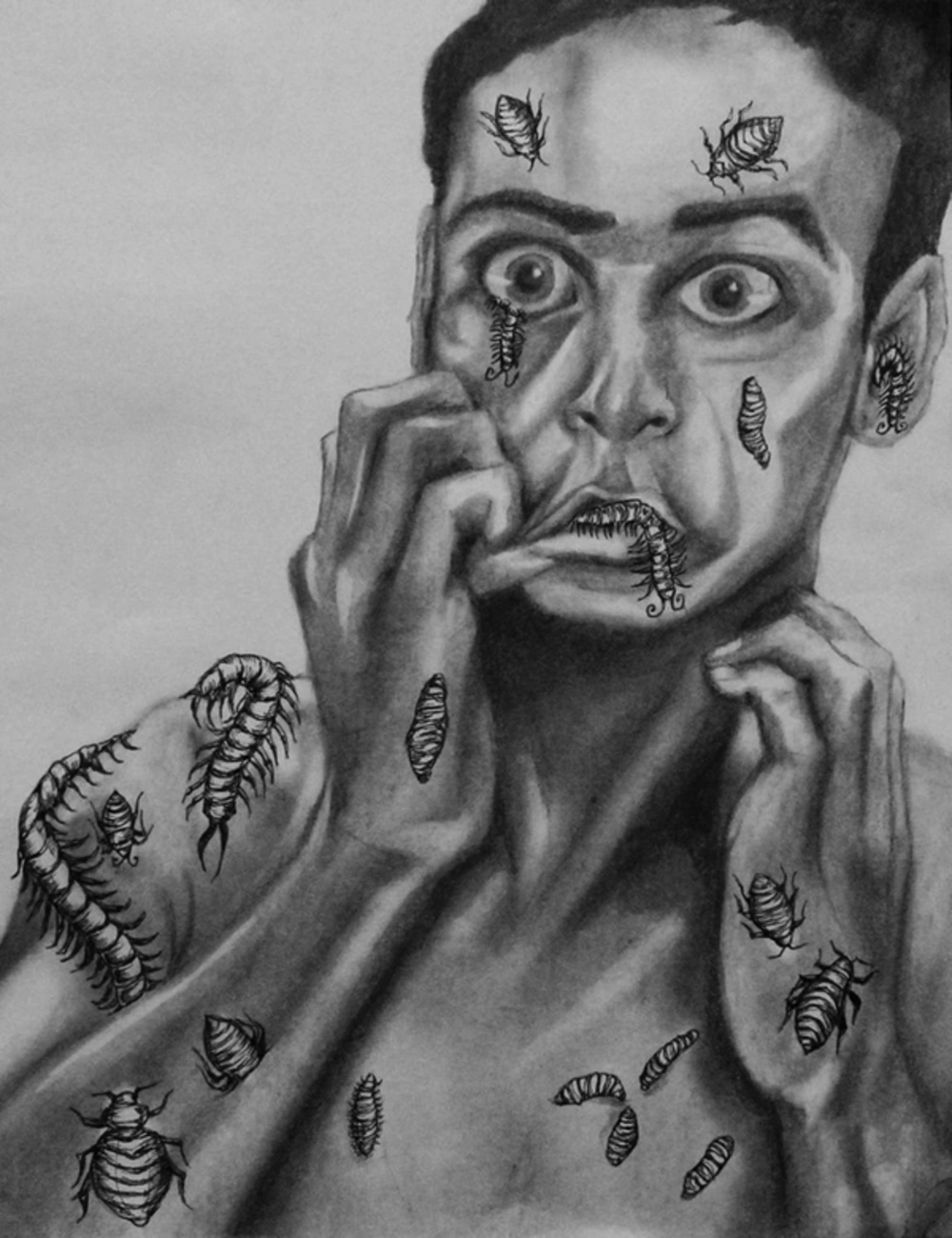
Patients with Delusional Parasitosis (DP), also known as Ekbom syndrome, have an unsurpassed conviction that organisms are living within and/or underneath their skin (Figure 1) (1). In young patients, DP can be the earliest sign of a major psychosis. Karl Ekbom described the principal manifestations of this disease in the early 20th century (2, 3). A similar nonsynonymous condition is called Morgellons disease, which falls within the same delusional complex. Thomas Browne first described it in the late 17th century, naming it “Morgellons disease”, in which delusional skin infestation by inanimate objects is described (4, 5). Somatic delusions are proven to be the most difficult to treat, while classical treatment of this condition should be a combination of both psychotropic medications and psychotherapy, atypical (2nd generation) antipsychotic represent the treatment of 1st choice (6, 7).
Ekbom Syndrome, Concept Art. (1)
Psycho-cutaneous disorders are more common in females. However, this delusional complex affects both males and females equally below 50 years of age. In addition, it is slightly more prevalent in females above the age of 50 years. It is considered a rare disease of a very low prevalence. Ekbom himself pointed out that it is common for psychotic patient to have delusions of creatures in and/or on the body. Delusional parasitosis affects 2.37 - 17 per million per year (2). The age of onset ranges from the 6th to 7th decades of life. However, primary (idiopathic) variant may occur in adolescents, and those in the age group of 20 - 40 years must be dealt with caution, as the disease itself can be a manifestation of a recreational substance abuse, including psychostimulants, cognitive enhancers, and Amphetamine-type stimulants (ATS). Many ES-sufferers are intelligent, medical professionals, and even research scientists (5, 7, 8).
The exact etiology is multifactorial and of a neurochemical basis in relation to the central Dopaminergic pathways of the brain. This is confirmed by triggering psychoactive agents (cocaine, amphetamine, ATS, etc.), its association with neuro-hormonal disorders, and senility (2, 4). It was proposed that decreased striatal dopamine transportation is incriminated in its pathogenesis. An MRI study in 2008 revealed the relevance of structural lesions in the corpus striatum, mainly the putamen nucleus, in secondary subtype of this disease. Further, the role of postsynaptic-D2 receptors in mediating the anti-psychotics’ effect gave the first neurochemical evidence, which is pertinent to the pathogenesis of the disease (9-12).
The dilemma in Morgellons disease, especially the primary (idiopathic) type, is convincing the patient of the true (psychiatric) nature of the condition, in order to avoid a “physician odyssey”, in which the desperate patient will seek help from one physician to the next, depleting all resources for patient and the physician, including financial ones. Accordingly, a solid doctor-patient rapport is a cornerstone for an efficient subsequent management (2, 4, 5). If the patient is diagnosed late or left untreated, his/her condition will become recalcitrant and fortified against management. Further, delusions do not resolve spontaneously, however, there is a high chance of remission if an antipsychotic drug is administered as early as possible, which happened in this case scenario. A multi-disciplinary team approach is essential for success. The physician must struggle until the patient is convinced and motivated to accept therapy, which is usually a combination of psychiatric and psychosomatic therapy. It is also vital to never refute an underlying cause or a functional explanation for secondary subtypes of the disease (2, 13, 14).
2. Case Presentation
The patient, Mrs L. D., is a 52 years old female patient from Hertfordshire-United Kingdom. She is a highly educated academic and a professorial researcher in the field of biomedical engineering. She has a certified intellectual quotient (IQ) of 146 on the Stanford-Binet IQ scale, a genius-level of intellect. The patient is married to a fellow researcher and has no children as consequence of female infertility. The patient is non-diabetic and non-hypertensive. She had no previous physiologic or psychiatric history, or any pertinent form of chronic illnesses. Her lifestyle is active and productive in the academia, dedicated to teaching post-graduate students and the field of research. The patient’s drug history was irrelevant, with an exception to what the patient described as “sporadic intake” of Amphetamine-type stimulant (ATS) during her undergraduate studies. It is worthy to emphasize that psychostimulants, including ATS, are correlated with neuropsychiatric disorders, including those of central dopaminergic pathways pathologies of the brain (15, 16). Furthermore, it has been proposed that such manifestations may vary in accordance with the patients’ handedness and cerebral dominance (17, 18).
In the past half-year or less, the patient presented with relapsing-remitting episodes of itching, affecting her left hand and the distal segment of the forearm, mainly the dorsal aspect, these lesions were not confined to a specific dermatomal pattern. The frequent scratching episodes, induced linear excoriated lesions. Within a few weeks, these lesions became crusted with micro-fissures and oriented longitudinally in relation to the longitudinal axis of the distal portion of the upper limb (Figure 2). The patient consulted a dermatologist he diagnosed her condition as a variant of seasonal dyshidrotic eczema affecting the skin during cold dry winters. She was prescribed some skin moisturizers as well as a sedative (1st generation) oral anti-histamine. The patient was compliant with treatment. However, the itchy lesions worsened and her sleep patterns became inconsistent, which lead to refractory insomnia due to severe itching sensation.
The patient re-consulted the dermatologist, who insisted on his diagnosis and added a moderate topical steroid, Clobetasone (Eumovate) ointment to be applied to the dry skin twice daily. He further added an antidepressant, tricyclic Amitriptyline 25 mg oral tablet to be taken once daily at night, her antihistamine was discontinued. Over the next 1 - 2 months, the patient sleep has improved, and she resumed her daily routine. However, the itching sensation became more severe during the day, which made the patient very desperate. Further, the patient started to describe an itchy “crawling” sensation underneath her skin. Later, she was convinced that she had caught some “foreign material” from the research laboratory, nanoparticles to be specific, from her latest research project in relation to nanotechnology. This research project was completed and her cutaneous manifestations appeared soon afterwards.
Consequently, her husband urged her to consult a psychiatrist, the psychiatrist opined to do a full neuropsychological evaluation in collaboration with a neurologist, in order to exclude any functional and/or organic brain pathology that may explain her condition. Concomitantly, the psychiatrist collaborated with a consultant dermatologist to exclude any functional dermatosis and/or a chronic eczematous skin condition that may behave in an analogous fashion. Patch test and skin prick test, Wood’s lamp, mycology test, and other dermatological investigations were done, which all resulted either negative or inconclusive. Accordingly, the dermatologist and the psychiatrist mutually agreed that the condition is of a neuropsychological basis. Furthermore, an MRI imaging of the brain, cervical the spine, and axillary region were done, all being completely normally. Routine PCV, CBC, LFT, RFT, serum electrolytes were within normal limits.
The patient psychiatric evaluation was normal, apart from depressive episodes in relation to her infertility. The depressions were associated with some disputation with the husband’s family, his sisters to be specific. Finally, the patient was diagnosed with a particular category of primary (idiopathic) delusional infestation, this condition is also known as Morgellons disease. The patient was prescribed a 2nd generation (atypical) antipsychotic, Olanzapine 2 mg/day oral tablet once daily at night, which was later incremented to 5 mg/day. All other medications were discontinued. Within 3 weeks, the patient improved significantly, and the crawling itchy sensation was non-existent, her hand and forearm appeared healing.
The level-of-evidence of this paper is Level-5, in accordance with the classification system by the Oxford centre for evidence-based medicine (CEBM) (19).
3. Discussion
This rare case report is both confounding and unique from an epidemiological perspective. The patient is highly intellectual, a research scientist. Her life was severely impaired by irritating episodes of itching and crawling sensations underneath the skin. A multidisciplinary approach with a neurologist and a Dermatologist proved to be a cornerstone, to avoid the classic “physician odyssey”. The patient history and investigations instigated a neuropsychological basis of the disease manifestation. However, the radiological tests further confirmed the absence of any pathologies that may explain such manifestations. The patient was finally diagnosed with Morgellons disease. An atypical antipsychotic was successful in inducing full remission of signs and symptoms. In parallel, the patient was referred for marital counseling to cope with her infertility problem and other marital-related quarrels.