1. Background
One of the most significant aspects of old people’s health is their mental health, deserving further attention (1). Of psychiatric diseases, whose outbreak increases with age, are cognitive, mood, and mental disorders, such as dementia, delirium, and depression disorders (2). The prevalence of age-related psychiatric disorders varies. In Iran, according to the 2013 census, the prevalence of various elderly period psychiatric disorders was reported as 23.6% (3). The elderly with psychiatric disorder were in need of daily activities being constantly supported and monitored by the caregivers (4). Family caregivers are considered as a part of the informal support system mainly in charge of the patient without receiving any financial reward (5-8). Family caregivers are a vulnerable population and like the elderly, they require special attention (9). Besides biological and physiological damage, stress and long-term caring impacts on the caregivers can result in fatigue (10, 11), and probably reduced job and social activities and disconnected relationships with family and friends (12, 13). A study found that an old person's physical ailment causes an increased financial burden, stress, and anxiety in the caregivers' personal lives (14). Another study revealed that caring of psychiatric elderly patients leads to nuisances, such as personal life stress, losing one’s job, additional financial burden and feeling guilty for the caregivers, resulting in the caregiving burden (15). Caregiving burden is covert in nature, meaning that the patient and the caregivers are both in pain and suffering and strongly need to be socially understood and supported (16). The mental disorder type, its duration and severity, the caregiving period, the incidence of problematic behaviors on the patient's side, lowered social protection and negative feelings can bring about further burden and lower quality of life (17, 18). Under the best state and conditions, the caregivers are affected by burden (19). Hence, family caregivers are considered the most significant protective system, and it seems that the perceived burden in the caregivers can play a decisive role in caregiving. The idea behind mental health concentrating on directing the activities on vulnerable populations is to prevent mental illnesses. For this purpose, it is required to preliminarily assess caregiving burden in family caregivers.
2. Objectives
The present study pursues to determine caregiving burden in the psychiatric elderly caregivers and its related factors.
3. Materials and Methods
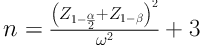
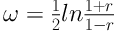
The study was a descriptive cross-sectional study. Two hundred caregivers of psychiatric elderly that had referred to Zare hospital clinic of Sari, Mazandaran province, were selected via convenient sampling. This paper was part of a thesis titled “association between attitude toward long-term care provision and caregiving burden in Sari based zare hospital psychiatric elderly family caregivers”, approved by Iran University of Medical Sciences and Health Services. The sample sizes in the original study were calculated by the following formula:
The inclusion criteria were as follows: being the caregiver of psychiatric elderly relative (spouse, sibling, child, and daughter-in-law), providing the highest caregiving during the day, providing mental, emotional, and social supports and the medical plan of the elderly in diverse forms (in person or in absentia), and caregiving duration of more than 6 months. The caregivers were 18 years old or older. The study samples were collected within 5 consecutive months from June to mid-November 2015, and the questionnaires were filled by the caregivers. In the proposal plan, when the caregivers were illiterate, the researcher read the questionnaires for them. There was no illiterate caregiver in this study.
3.1. Ethical Considerations
The ethical committee of Iran University of Medical Sciences of Tehran approved the study. The caregivers were informed verbally about the purpose of the study and signed a written informed consent. In this study, the caregivers had the right to decide on participating in the study or leave at any time. The data were confidential.
3.2. Data Collection Tool
The demographics form of the elderly included gender, marital status, education, the psychiatric disorder type, the disorder duration, job status and insurance, and that of the caregivers covered age, gender, marital status, relation, education, economic status, employment status, the number of psychiatric patient members in the family, and care giving hours per week.
3.3. Zarit Burden Interview
Burden Inventory of Zarit et al., is the most established tool that measures the perceived burden of family caregivers (20). The inventory consists of 22 questions in a 5-point Likert scale. Each question has 5 choices given scores as “never (0), almost (1), sometimes (2), often (3), and always (4)”. Total scores indicate the care giving burden. After analyzing and determining the cut-off point, scores of less than 30 were defined as mild burden, 31 to 60 as average burden, and 61 to 88 as severe burden. The ZBI explores negative physical, mental, social, and economic impacts of care giving on the life of the caregiver. Navidian et al. have culturally adjusted this scale and its Congruent validity was confirmed with high and positive correlation with the Hamilton anxiety scale (r = 0.89) and beck depression inventory (r = 0.67). The internal reliability of the inventory was 0.94 (21). The questionnaires were filled out by the caregiver. The SPSS 21 software was used to analyze the date with descriptive and inferential statistics such as analysis of variance (ANOVA), independent t-test, and Scheffe Post hoc test.
4. Results
Fifty-two percent of the caregivers were male, 94% married, and 57.4% of them were in the age group of 40 to 59 years old. The majority of the caregivers were the children of the patients (48.5%) followed by spouses (29.5%). About half (49%) of the caregivers were post diploma holders. More than half (67.8%) of them had an average economic status. Around 86.4% of them only had cared for one psychiatric elderly and 13.6% took care of another psychiatric patient at home in addition to the psychiatric elderly. The highest care-giving hours per week was 35 to 44 hours (Table 1).
| Demographic Data | Frequency | Percent |
|---|---|---|
| Gender | ||
| Male | 104 | 52.00 |
| Female | 0.96 | 48 |
| Age, y | ||
| > 40 | 33 | 16.7 |
| 40 - 59 | 113 | 57.4 |
| 60 - 70 | 0.0051 | 25.9 |
| Mean ± S.D = 51.24 ± 12.96, Min = 22, Max = 70 | ||
| Education | ||
| Under diploma | 0.0012 | 6.00 |
| Diploma | 0.0090 | 45 |
| College education | 0.0098 | 49 |
| Marital status | ||
| Single | 0.0013 | 6.00 |
| Married | 0.0187 | 94 |
| Economic status | ||
| Poor | 0.00.06 | 030.00 |
| Average | 0.00135 | 97.5 |
| Well-off | 0.0058 | 29.2 |
| Employment | ||
| Housewife | 0.0040 | 20.00 |
| Farmer | 0.0032 | 16.00 |
| Self-employed | 0.0033 | 16.5 |
| Jobholder | 0.0066 | 33.00 |
| Retired | 0.0029 | 14.5 |
| Another psychiatric person in family | ||
| No | 0.00173 | 86.4 |
| Yes | 0.0027 | 13.6 |
| Weekly patient care hours | ||
| < 24 hours | 0.0028 | 14.00 |
| 24 - 34 hours | 0.0071 | 35.5 |
| 35 - 44 hours | 0.0080 | 40.00 |
| > 44 hours | 0.0021 | 10.5 |
| Mean ± S.D = 34.24 ± 24.09, Min = 14, Max = 56 | ||
| Relation | ||
| Spouse | 0.0059 | 29.5 |
| Child | 0.0097 | 48.5 |
| Daughter/son-in-law | 0.0022 | 11.00 |
| Other relatives | 0.0022 | 11.00 |
The Psychiatric Elderly Patient Caregivers’ Demographic Data
In addition, the results showed the mean age of patients was 71.96 ± 2.27 years, ranging from 60 to 92 years; 51% were male, 54.5% married, and 46.2% of them were jobless with no income; about 42.7% had a psychiatric disorder for 10 to 19 years. In this study, depression and anxiety had a higher and lower frequency, respectively (Table 2).
| Demographic Data | Frequency | Percent |
|---|---|---|
| Gender | ||
| Male | 102 | 51 |
| Female | 98 | 49 |
| Age | ||
| 60 – 69 | 92 | 46 |
| 70 – 79 | 83 | 41.5 |
| < 80 | 25 | 12.5 |
| Mean ± S.D = 71.96 ± 7.27, Min = 60, Max = 92 | ||
| Education | ||
| Illiterate | 72 | 36 |
| Under diploma | 61 | 30.5 |
| Diploma | 44 | 22 |
| Post diploma | 32 | 11.5 |
| Marital status | ||
| Single | 10 | 5 |
| Married | 109 | 54.5 |
| Widow | 81 | 40.5 |
| Employment | ||
| Jobless | 92 | 46.2 |
| Farmer | 49 | 6 |
| Self-employed | 5 | 2.6 |
| Retired | 53 | 26.6 |
| Disease duration | ||
| 10 < | 35 | 17.6 |
| 10 – 19 | 85 | 42.7 |
| 20 – 29 | 52 | 26.1 |
| > 30 | 27 | 13.6 |
| Mean ± S.D = 18.05 ± 9.65, Min = 3, Max = 42 | ||
| Psychiatric disorder type | ||
| Schizophrenia | 59 | 29.5 |
| Anxiety | 14 | 7 |
| Mania | 43 | 21.5 |
| Depression | 63 | 31.5 |
| More than one disorder | 21 | 10.5 |
The Psychiatric Elderly Patient’s Demographic Characteristics
It was found that 32%, 56%, and 12% of caregivers had mild, average, and severe burden, respectively. The mean scores of personal, emotional, social, and economic caregivers’ burden were 15.67 ± 5.6, 13, 57 ± 1.05, 4.75 ± 33.3, and 4.81 ± 1.55, respectively. The results showed that caregivers’ burden had a meaningful association with type of psychiatric disorder in elder patients (F = 4.330, df = 4.174, and P = 0.002). Post Hoc test showed caregivers’ burden was higher in caring for schizophrenic patients and then obsessive-compulsive, mania, depression, and anxiety disorders, respectively. The results denoted that care giving hours per week (t = 2.97, df = 31.54, and P < 0.001) and additional psychiatric patients number in the family (t = 2.97, df = 31.54, and P = 0.006) had an association with care giving burden. Post Hoc test showed that greater care giving hours/week was associated with higher care giving burden (Table 3).
| Demographic Data | Mean | SD | Test Result |
|---|---|---|---|
| Gender | t = 1.34, df = 198, P value = 0.181 | ||
| Male | 40.11 | 14.43 | |
| Female | 37.46 | 13.45 | |
| Age, y | F = 0.788, P value = 0.456 | ||
| < 30 | 38.24 | 13.81 | |
| 30 – 39 | 39.74 | 14.66 | |
| 40 – 49 | 36.33 | 11.95 | |
| 50 – 59 | 41.25 | 13.42 | |
| 60 – 69 | 37.99 | 13.52 | |
| 70 – 79 | 43.45 | 15.96 | |
| Education | F = 1.63, P value = 0.184 | ||
| Under diploma | 37.33 | 13.52 | |
| Diploma | 36.6 | 12.1 | |
| College education | 39.98 | 14.53 | |
| Marital status | t = -0.713, df = 117, P value = 0.477 | ||
| Single | 38.54 | 14.10 | |
| Married | 40.39 | 14.51 | |
| Economic status | F = 2.854, P value = 0.061 | ||
| Poor | 34.04 | 10.66 | |
| Average | 37.32 | 13.75 | |
| Well-off | 48.33 | 15.23 | |
| Employment | F = 0.202, P value = 0.937 | ||
| Housewife | 39.61 | 13.64 | |
| Farmer | 35.96 | 14.32 | |
| Self-employed | 40.57 | 14 | |
| Jobholder | 38.69 | 14.89 | |
| Retired | 38.33 | 13.29 | |
| Another psychiatric person in family | t = -2.97, df = 31.54, P value = 0.006 | ||
| No | 38.32 | 14.33 | |
| Yes | 38.17 | 13.63 | |
| Weekly patient care hours | t = -2.97, df = 31.54, P value = 0.006 | ||
| < 24 hours | 37.51 | 13.18 | |
| 24 - 34 hours | 47.3 | 16.33 | |
| 35 - 44 hours | 34.78 | 14.45 | |
| > 44 hours | 35.49 | 13.17 | |
| Relation | F = 1.363, P value = 0.255 | ||
| Spouse | 40.00 | 14.27 | |
| Child | 50.86 | 10.99 | |
| Daughter/son-in-law | 38.54 | 14.10 | |
| Other relatives | 40.39 | 14.51 | |
| Psychiatric disorder type | F = 4.330, P value = 0.002 | ||
| Schizophrenia | 44.59 | 15.82 | |
| Anxiety | 27.60 | 5.54 | |
| Mania | 37.81 | 12.18 | |
| Depression | 35.71 | 12.92 | |
| Obsessive-compulsion | 39.33 | 12.60 |
Caregivers’ Burden Numerical Indicators in Terms of Demographic Data
5. Discussion
The study findings imply high burden in caregivers. The achieved results indicated that 32% of the caregivers had mild burden and 68% had average to severe burden. This finding was compatible with previous studies on caregivers of elderly in Iran (4, 22-24). Another study was not consistent with our result (15). Based on the findings, out of the care giving burden dimensions, only 2, including personal and emotional aspects, were associated with disease duration in the psychiatric elderly. A study from Italy on caregiver's burden and quality of life of elderly patients with physical and mental illness also revealed emotional, personal, and economic burden associated with disease duration in the caregivers (9). The present study revealed that the main caregivers were children of the patients followed by spouses. Although the care giving burden of the children was higher than that of other caregivers (spouse, daughter-in-law, daughter, and son-in-law), this difference was not significant (Table 3). This study revealed that almost half of the caregivers were male, the gender of the caregivers was divulged no meaningful association with care giving burden while burden scores of males were higher than that of females (Table 3). Similar to this study, earlier studies (22-26) found that the mean caregiving burden scores among males were higher than that of females. However, the existing difference somewhat depends on the cultural context of the study setting, such as significant role of males as a breadwinner and supplier of financial requirements in Iranian families and ability of males in physically handling the patients. The majority of the participating caregivers in this study were married, which may indicate economic security and sense of responsibility compared to single individuals; marital status showed no significant relationship with caregiving burden. Married caregivers had higher mean burden scores than single caregivers (Table 3). In addition, the mean burden scores of the caregivers aged 45 to 65 was reported more than that of other age categories. However, this age difference was not significant. The mean caregiving burden scores according to the perceived economic condition based on Post Hoc test indicated higher caregiving burden in low-income caregivers. The above findings are in line with some previous studies (4, 9, 15). This finding asserted the significant role of economic status in caregiving of patients. The present study also revealed that the elderly caregiving hour/week and having additional family psychiatric members and type of psychiatric disorders of the elderly had a meaningful association with caregiving burden. The present study findings are in accordance with that of such studies (9, 22, 27). Additionally, the presence of another psychiatric patient in the family along with the elder psychiatric patient raised the burden for the caregivers. Other studies (28, 29) denoted that long term care of elder Alzheimer patients led to reduced burden in the caregivers. The existing difference in these studies can somehow be justified according to adaptability, individual characteristics, cultural and traditional beliefs of the caregivers; it seems, the caregivers with higher adaptation abilities and responsibility for the existing circumstances experience less burden, while those with lower adaptability reported higher burden (30). The findings showed that caregiver burden had a significant difference according to type of psychiatric disorders among elder patients. Schizophrenic patients’ caregivers experienced a higher burden. This result was congruent with other of studies (31, 32). Results showed that elder male patients imposed a greater burden on their caregiver in comparison with women patients. However, this difference was not statistically significant. The results are similar to some other studies (23, 25, 33). This can attributed to worse psychiatric disorder prognosis in males than in females and greater resistance to treatment in male patients (34).
In summary, the findings imply high burden in the caregivers in this Iranian samples, thus, it is necessary to promote the families' knowledge and awareness to reduce long-term care giving burden. In addition, evidence showed elderly psychiatric patient caregivers’ burden is related to care recipient factors. Counseling services, cooperation between public and private organizations, training programs by the national media and application of respite care (35) are suggested to alleviate the burden among psychiatric elder patient caregivers
Findings of this study should be interpreted with caution. The use of convenient sampling method limited the generalization of the findings. As well as analysis, data from self-report measures should be interpreted with caution. The adequate sample size also supports the findings to conclude a true relationship between common characteristics of patients and caregivers with the burden. In addition, the use of an instrument with accepted psychometric properties confirms that the variables were measured correctly. Based on the findings, many research questions emerge such as: What are predicators or moderators of the elderly psychiatric patient caregivers' burden? Do psycho-educational interventions alleviate caregiver burden? Can positive psychological characteristics in elder patients or caregivers moderate the caregiver burden? What are specific factors related to burden according to type of psychiatric disorders? How does cultural differences effect caregiver burden?