1. Introduction
Many studies have shown a complex relationship between psychotic symptoms and immune system disorders, including autoimmune conditions (1). In some patients with first psychotic episodes, the anti-N-methyl-d-aspartic acid receptor (NMDAR) antibody, as well as antibodies against the potassium channel, have been found (1).
Anti-NMDAR autoimmune encephalitis is one of the most challenging disorders with both psychiatric and neurologic presentations. Distinguishing auto-antibodies against neuronal receptors in neuropsychiatric disorders would shed light on some aspects of psychotic disorders like schizophrenia (2).
Approximately three-fourth of patients with anti-NMDA receptor encephalitis (anti-NMDARE) are first referred to psychiatrists (3, 4). The psychiatric symptoms of this disorder include auditory and visual hallucinations, delusions, bizarre and disinhibited behaviors, agitation, and impaired consciousness. There are also other symptoms like motor disturbances (ranging from dyskinesia to catatonia), seizures, and autonomic dysfunction. Mild lymphocytic pleocytosis mildly increased CSF protein concentration, and specific oligoclonal bands have been shown in about 80% of patients (5).
There are two groups of differential diagnosis for psychotic symptoms in children and adolescents, including psychiatric disorders (schizophrenia, mood and anxiety disorders, attention-deficit/hyperactivity disorder, posttraumatic states, autism spectrum disorders, etc.) and other medical conditions or organic brain psychosis. Other medical conditions associated with psychosis are infections (Creutzfeldt-Jakob disease, herpes encephalitis, human immunodeficiency virus infection, etc.), metabolic disturbances (adrenocortical insufficiency, Cushing’s disease, hypercalcemia, hypocalcemia, etc.), neurologic conditions (cerebral neoplasms, cerebrovascular diseases, encephalitis, etc.), certain genetic syndromes (fragile X syndrome, Klinefelter’s syndrome, metachromic leukodystrophy, etc.), and vitamin deficiencies (folate deficiency, niacin deficiency, vitamin B12 deficiency, etc.) (6).
Because of various demonstrations of this serious but treatable disorder, its diagnosis may be difficult. The golden time for diagnosis is the most important point which must be noticed. On the other hand, a total lack of specific guidelines, not only for diagnosis but also for treatment, makes the situation more complicated.
In this case report, we presented a teenage girl with anti-NMDAR encephalitis, who manifested with depression, suicidal ideation, and cognitive impairment leading to poor school performance during the past one year. Because of these early symptoms, she was only treated for depression. Her symptoms followed by behavioral changes, acute psychosis, and eventually neurological symptoms, but again, due to the lack of clinical suspicion, the correct diagnosis was not made. The patient was hospitalized in a psychiatric hospital after normal primary neurological assessments and normal CSF tests. Finally, due to acute psychosis symptoms and the presence of seizures, neurological counseling was performed. This case is invaluable as it reminds us of the importance of having clinical suspicion for the correct diagnosis and timely treatment of this disorder.
2. Case Presentation
A 15-year-old single female adolescent who was a student of the ninth grade, living in Tehran, was admitted to a psychiatric hospital with changes in behaviors, aggressive outbursts, impaired attention, suicidal ideas, depressive mood, lethargy, and anorexia, for the past one whole year. During this time, her performance at school was becoming impaired, and her interpersonal relationships were getting shaky.
She was hopeless, and therefore, she was referred to a psychiatrist. Selective serotonin reuptake inhibitor (SSRI) was prescribed for her depressive symptoms, but not only did the symptoms not improve, but they also exaggerated day by day. No other psychopathology was found, and she had no history of any manic symptoms so far. There were no signs of other medical illnesses or histories of substance and alcohol abuse. Her physical and psychological development was normal, and her family history showed diabetes and Hashimoto’s hypothyroidism.
On 23th March 2017, she suddenly showed disinhibited behaviors like wearing inappropriate clothes or shoplifting, but they lasted a short time, and she was not visited by her medical doctor during this period.
On 8th April 2017, stupor and generalized tonic-colonic (GTC) seizures appeared. Therefore she was hospitalized at the emergency department of a general hospital. The symptoms were controlled by intravenous diazepam, and she was discharged after a couple of hours. She showed no signs of fever or infections and did not report any head trauma. Disinhibited behaviors and irrelevant speaking before and after the seizures were reported by her family, which were assumed as seizures auras. After an argument on the next day at home, GTC seizures occurred two times, and she was immediately transferred to the hospital. Seizures again occurred on two additional occasions, and she showed fluctuations in the consciousness level and disinhibited behaviors (e.g., swearing during medical interview, knocking herself to the window to jump out, and incoherent speech). Except for deep tendon reflexes, which were symmetrically reduced (2+), other neurological examinations, including cranial nerve tests, movement tests, muscles’ tones, and gait and cerebellar functional evaluations were normal. The brain computed tomography (CT) and magnetic resonance imaging (MRI) scans, cerebrospinal fluid (CSF) test, and other primary lab tests (complete blood cell count, liver function tests, electrolytes, urine toxicology analysis for substance abuse, fasting blood sugar, and renal functional tests) were all normal. In electroencephalograms (EEG), many artifacts were reported due to poor cooperation; however, generalized sharp and slow waves were detected prominently on the left side. After stabilization, she was discharged with 200 mg/three times a day of carbamazepine and Ca-D daily. She was recommended to meet a neurologist and a psychiatrist the other day.
After the neurological assessments, on 29th April 2017, she was referred to a psychiatric hospital due to her aggressive and uncontrollable behaviors in addition to sleep disturbance, rapid mood swings, restlessness, stereotypic behaviors, fluctuating attention and concentration, misidentification delusion, and perceptual changes (i.e., the color of everywhere was changed to blue). In the mental state examination, the recent and remote memories, the working memory, four-digit forward and backward tests, general knowledge, concentration, calculation, and time orientation were impaired. She was irritable and cursing suddenly during the interviews.
During the first hospitalization, primary differential diagnoses were bipolar mood disorder with psychotic features and substance-induced psychotic disorder. As there was a history of recent seizures without any report of substance abuse in a young girl with first-episode psychosis, new consultation with a neurologist was suggested to rule out neurological conditions such as encephalitis.
All laboratory tests (complete blood cell count, liver functional tests, electrolytes, urine toxicology for substances, fasting blood sugar, kidney tests, thyroid function tests, viral markers, paraneoplastic antigens, lupus anticoagulants, and rheumatologic tests) were normal, and the urine toxicology test was negative for any substance. Generalized slowing and generalized epileptic form discharges were reported in EEG while agitation and suicidal ideas were prominent in her mental state examination. Brain MRI, with and without contrast, was normal. Chest, abdominal, and pelvic CT scans were normal, and tumor markers were negative.
Then autoimmune panel tests were requested while agitation and confusion were making the patient out of control.
Carbamazepine (400 mg) two times a day, quetiapine (100 mg) two times a day, Na-valproate (500 mg) two times a day, and folic acid and Ca-D supplements daily were prescribed, but she did not show any clinical improvement and gradually became more agitated.
Finally, anti-glutamate receptor antibody was reported in her CSF, and anti-NMDA receptor encephalitis was finally diagnosed.
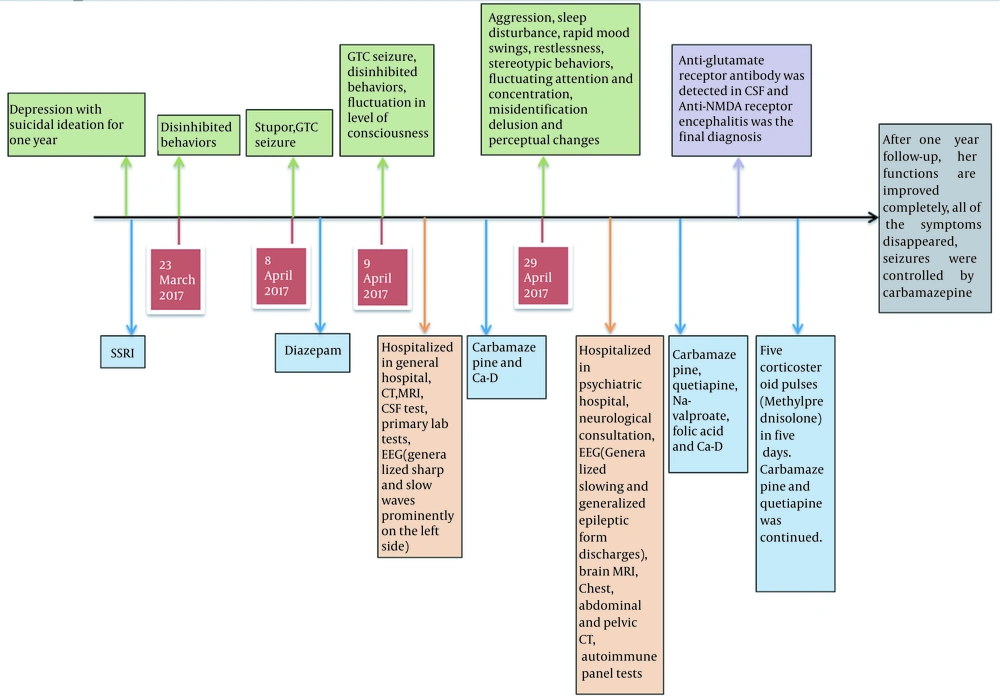
She received five corticosteroid pulses (methylprednisolone 500 mg) in five days. Carbamazepine and quetiapine continued. Her symptoms decreased afterwards, but memory impairments were still notable. After one year of follow-up, her family and the patient reported that her school performance and interpersonal relationships were completely improved, and all the symptoms disappeared. Moreover, seizures were controlled by carbamazepine, and her memory impairment also completely recovered. Nowadays, her quetiapine is discontinued, and carbamazepine dosage is decreased. She does not suffer from any adverse effect for now. Figure 1 shows the complete clinical timeline referring to this case.
3. Discussion
Several studies have shown that anti-NMDA receptor encephalitis is ranked second among antibody-associated encephalitis. Prevalent presentations are personality changes, psychosis, and catatonia (7).
As an inotropic glutamate receptor, NMDA-R is expressed in the presynaptic area and has effects on synaptic transmission, brain plasticity, and maturation (8). In anti-NMDA-R encephalitis, because of autoantibodies against NMDA receptor1 (NR1), the function of NMDA receptor decreases (9). Some studies have found a relationship between the hypo-functionality of NMDA-R and schizophrenia, which may explain psychotic symptoms in anti-NMDA-R encephalitis (10).
Anti- NMDA-R encephalitis symptoms are classified into different stages; a flu-like phase in 70% of patients presenting with fever, headache, nausea, vomiting, diarrhea, or upper respiratory tract symptoms. The next stage includes psychiatric symptoms such as anxiety, insomnia, mania, grandiosity delusions, hyper-religiosity, and paranoia. This stage is followed by autonomic instability, seizures, decreased responsiveness, and in some cases, short-term memory impairments (11). In our case, due to deficits in attention and some depression-like symptoms, the patient’s function was impaired at the school. No flu-like symptoms were reported by the patient and her family. After that, disinhibited behaviors and seizures appeared and followed by psychosis, disorganized behaviors, mood swings, and insomnia. Her recent and remote memories, working memory, concentration, and orientation were also impaired. Since the initial symptoms were merely psychiatric without any physical sign, there was not a high clinical suspicion for association with medical conditions. After the occurrence of seizures, medical examinations were performed more precisely, all of which were normal, which is one of the features of this disorder, rendering it undiagnosed. The strength of our approach was that, despite repeated neurological visits, we simply did not accept that the problem was only psychiatric due to acute symptoms and seizures and asked for more neurological consults.
Nearly 40% of these cases are below 18 years old. Usually, the patients are hospitalized in psychiatric wards because of their psychotic symptoms, and in this phase, primary or secondary psychosis is not easily distinguishable. Unfortunately, some evaluations like brain MRI (60%) and routine CSF analysis, unless antibodies are investigated (10%), are not diagnostic; however, EEG is usually abnormal (12). These atypical early manifestations, the normality of early tests and imaging, and the absence of clinical suspicion are among the most important barriers for the diagnosis of the disorder. Therefore, patients may be treated for a primary psychiatric disorder without fully responding to the treatments and visiting different psychiatrists while the course of the disorder deteriorates. This was the scenario that happened to our patient.
Just as the above explanation, our case's brain MRI scans, and CSF analysis were normal, but EEG had pathologic changes (i.e., generalized slowing and generalized epileptiform discharges).
The first-line treatment of anti-NMDA-R encephalitis is immunotherapy [corticosteroids, intravenous immune globulin (IVIG), and plasma exchange], improving the symptoms in 53% of the cases during one month. The second-line therapy is immunosuppression (rituximab or cyclophosphamide) (5). Differences in initial treatment regimens, based on specialty, include an increased use of plasma exchange by adult neurologists (27%) and rituximab by pediatric rheumatologists (29%). Physicians in the US also utilize the second-line treatment earlier than most of their European peers (13). Antipsychotics can be used for psychiatric symptoms, but their adverse effects like extrapyramidal symptoms before the correct diagnosis may complicate the clinical diagnosis. On the other hand, corticosteroids may induce psychosis (5). In our patient, we obtained an adequate response with the first-line therapy.
Psychiatric symptoms are usually controlled by psychotropic drugs, but there is a higher risk of side-effects like neuroleptic malignant syndrome (NMS) in these patients (14). We used quetiapine in this case, which did not result in any adverse effect.
There is not enough information about how long immunotherapy should last, so we discontinued corticosteroid therapy after the symptoms improved. She recovered completely after one year.
In summary, in patients with first and acute psychotic symptoms, especially in young patients with seizures, the possibility of autoimmune disorders should be kept in mind, and complementary tests must be done for detecting possible autoantibodies in these patients.