1. Context
Suicide is a major public health concern worldwide, which causes severe health consequences and adversities for survivors. Annually nearly 800000 people die due to suicide worldwide. Most cases of suicide are associated with psychiatric disorders so that over 90% of cases of suicide commitment are attributed to mental health disorders. Also, 51% of them have a history of major depressive disorder (1-3). Self-immolation is defined as ending life by suicide, particularly through burning. Furthermore, in some countries, it has political reasons. Survivors of self-immolation experience significant scars and a prolonged and painful recovery, both physically and psychologically. Moreover, it imposes considerable costs to both families and the healthcare system (4, 5). As injuries and burns caused by self-immolation are deeper and more extensive than those occurring in accidents, it carries high morbidity and mortality. Therefore, self-immolation should be distinguished, in its clinical and psychosocial aspects, from other types of self-harm.
Various factors contribute to self-immolation, depending on the cultural and socio-demographic characteristics, psychiatric disorders, and experienced adverse life events (6, 7). In most of the low- to middle-income countries, young women and teenage girls are at increased risk of self-immolation, while in high-income countries, it’s more common among older men (5, 8, 9). In Iran, self-immolation is a common method of suicide among women, with significant differences among various regions of the country (mostly in the north and west of the country). Most cases of self-immolation among Iranian women are attributed to psychosocial problems.
The current study aimed to review the literature and summarize the evidence on suicide by self-immolation to assess the socio-cultural and epidemiological covariates of self-immolation. We have tried to answer the following epidemiological and clinical questions in the Iran context: Areas with the highest prevalence of this behavior; those who are at increased risk of self-immolation; cultural factors that contribute to self-immolation; injuries that cause by self-immolation; and, last but not least, what is known about the risk factors, causes, and associated social problems? the findings of this study could contribute to understanding the factors associated with self-immolation to identify the potential target groups and developing preventive strategies to reduce the incidence of self-immolation.
2. Evidence Acquisition
2.1. Search Strategy
This is a narrative review of available literature, both in English and Persian, on self-immolation in Iran. First, a list of keywords and terms related to self-immolation, suicide, self-burn, and deliberate self-harm was developed. We systematically searched the US National Library of Medicine (PubMed), the online abstracts and citations database of Elsevier’s SciVerse (Scopus), Psychinfo, and ISI Web of Science to identify relevant studies from the time of inception of these databases to June 17th, 2017. Also, Iranian databases of Iran Medex, scientific information database (SID), and the national magazines’ database (Magiran) were searched to find Persian studies using the Persian equivalents of the above-mentioned keywords. According to each database specifications, a sensitive search of the literature was performed using combinations of different terms and subject headings related to the population (Iran), indices (prevalence, epidemiology, incidence), and outcomes (self-immolation, self-burn, deliberate self-burning, women).
2.2. Summarizing, Extracting, and Reporting the Data
All cross-sectional, longitudinal, cohort, case-control, descriptive, and review studies, either in English or Persian, were included. Two reviewers independently reviewed the titles and abstracts of potentially relevant studies for eligibility criteria. Afterward, the same two reviewers independently applied the inclusion/exclusion criteria for articles that were selected for full-text review. Then data were extracted by the two reviewers working alone and then cross-checked.
Data extraction sheets contained data on the first author, study date (year), publication date (year), place (province, etc.), the field of study (rural/urban), sample size, and methodology. The sheets were independently completed by the reviewers for each eligible study.
3. Results
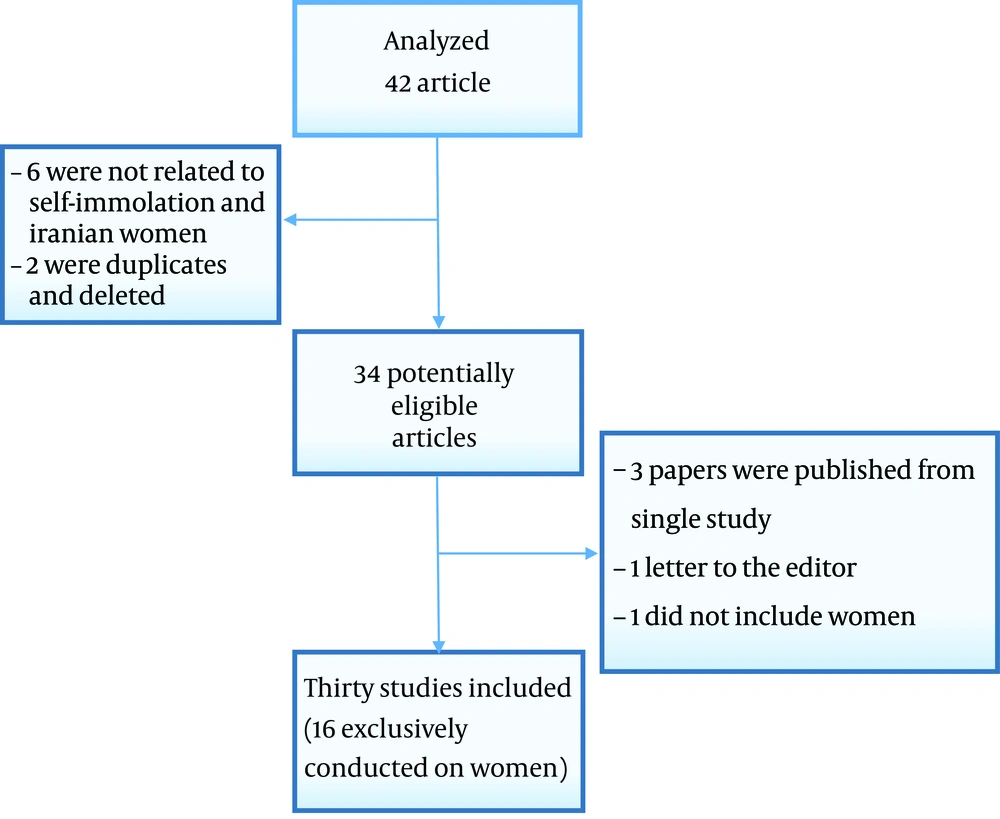
Thirty studies were included in this review (Tables 1 and 2). The study selection process is depicted in Figure 1.
| Authors | Study Date, y | Study Type | Sample Size | Gender Female/Male | Data Source | Province | Setting/Participants | |
|---|---|---|---|---|---|---|---|---|
| 1 | Zarghami and Khalilian (10) | 1991 - 1993 | Prospective descriptive | 318 | 264/54 | Medical record | Mazandaran/Iran | The burn unit of Mazandaran University of Medical Sciences |
| 2 | Aliverdinia and Pridemore (11) | 1995 - 2000 | Review | N/A | N/A | Registered data | Iran | Management and planning organization of Iran |
| 3 | Dastgiri et al. (12) | 1998 - 2003 | Retrospective descriptive | 98 | 23/75 | Medical record | North West of Iran | N/A |
| 4 | Amirmoradi et sl. (13) | 2001 - 2002 | Descriptive | 35 | 35/0 | Interview | Tehran/Iran | Burn referral center |
| 5 | Ahmadi et al. (14) | 2003 - 2004 | Review | 1157 | 340/817 | Registered data | Iran | National research center of medical science |
| 6 | Shakeri et al. (15) | 2003 - 2004 | Cross - sectional | 126 | 98/28 | Interview | Kermanshah/Iran | A tertiary referral hospital |
| 7 | Mohammadi et al. (16) | 2003 - 2006 | Prospective | 283 | 193/90 | Medical records | Fars, Iran | Burn referral center |
| 8 | Heydari (17) | 2003 - 2014 | Cross - sectional | 3105 | 1196/1909 | Registered data | Kermanshah/Iran | Death registry of Iranian legal medicine organization |
| 9 | Ahmadi (18) | 2004 - 2005 | Retrospective cross - sectional | 37 | 7/30 | Medical record | Kermanshah/Iran | Emergency department of 20 hospitals & A burn center of KUMS |
| 10 | Alaghehbandan et al. (19) | 2005 - 2006 | Prospective cohort descriptive | 51 | 36/15 | Interview | Ilam, Iran | Burn referral center |
| 11 | Alaghehbandan et al. (20) | 2006 | prospective descriptive | 181 | 130/51 | Interview | Ilam, Khorasan/Iran | Referral burn centers in Ilam and Khorasan |
| 12 | Shojaei et al. (21) | 2006 - 2010 | Retrospective descriptive | 15755 | 11091/4664 | Registered data | Ilam, Iran | Forensic medical center |
| 13 | Ahmadi et al. (22) | 2007 - 2008 | Case control | 60 | 52/8 | Interview | Kermashah/Iran | A tertiary referral hospital |
| 14 | Rezaie et al. (8) | 2008 | Prospective descriptive | 63 | 60/3 | Interview | Kermanshah/Iran | A tertiary referral hospital, trauma center of KUMS |
| 15 | Mohammadi et al. (23) | 2009 - 2012 | Prospective descriptive | 388 | 122/266 | Interview | Fars/Iran | Burn referral center |
| 16 | Malakouti et al. (9) | 2010 - 2011 | Field trial | 17 | 7/10 | Medical records | Nahavand and Savajbolagh/Iran | Primary health care |
| 17 | Dahmardehei et al. (24) | 2010 - 2012 | Retrospective cross - sectional | 315 | 104/211 | Medical record | Zahedan/Iran | A tertiary hospital |
| 18 | Zamani et al. (25) | 2011 - 2012 | Case control | 30 | 18/12 | Questionnaire | Hormozagan/Iran | A tertiary referral hospital |
| 19 | Hosseini et al. (26) | 2011 - 2014 | Retrospective descriptive | 74 | 52/22 | Medical records | Mazandaran, Iran | Referral hospital of psychiatric diseases and burn |
| 20 | Hosseini et al. (27) | 2012 | Case control | 157 | 82/75 | Medical record | Yasuj, Iran | General hospital |
| 21 | Khankeh et al. (28) | 2012 - 2013 | Grounded theory | 14 | 0/14 | Interview | Kermanshah/Iran | A tertiary hospital, burn center Of KUMS |
| 22 | Rostami et al. (29) | 2012 - 2013 | Descriptive | 265 | 91/174 | Registered data | Kermanshah/Iran | Forensic medical center |
| 23 | Karim et al. (30) | 2013 | Case control | 60 | 52/8 | Interview | Kermanshah/Iran | A tertiary referral hospital |
| 24 | Ahmadi et al. (31) | 2013 | Case control | N/A | N/A | Interview | Kermanshah | A tertiary hospital, burn center of KUMS |
| 25 | Malakouti et al. (32) | Up to 2013 | Review | N/A | N/A | Online data bases | N/A | N/A |
| 26 | Boostani et al. (33) | N/A | Grounded theory | 11 | 11/0 | Interview | Lorestan, Iran | Consult center |
| 27 | Ahmadi et al. (7) | N/A | Case control | N/A | N/A | Interview | Kermanshah/Iran | A tertiary referral hospital |
| 28 | Suhrabi et al. (5) | N/A | Review | N/A | N/A | Online data bases | N/A | N/A |
| 29 | Mami et al. (34) | N/A | Review | N/A | N/A | Online database | Iran | N/A |
| 30 | Heidari Zadi et al. (35) | N/A | Cross sectional | 251 | 95/156 | Medical record | Kermanshah/Iran | Medical documents of 251 patients admitted at medical centers of KUMS |
Characteristics of the Included Studies
| First Author | Study Date | Age (Mean ± SD) | Field of Study (Urban Vs. Rural) | Low Level of Literacy | Married, % | Low Socio-Economic Status | Psychiatric Diagnosis, % | Outcome (Death %) | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Zarghami and Khalilian (10) | 2002 | 26.9 | 48% R | 57% | 70.5 | N/A | 95 | 79% |
| 2 | Aliverdinia and Pridemore (11) | 2009 | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 3 | Dastgiri et al. (12) | 2005 | 27 | 32.7% R | N/A | 51.1 | N/A | 15 | 75.5% |
| 4 | Amirmoradi et al. (13) | 2005 | 24.57 ± 3.94 | N/A | 77% | 100 | 68.8% | N/A | 100% |
| 5 | Ahmadi et al. (14) | 2008 | 29 | 65.6% R | N/A | N/A | 23% | N/A | N/A |
| 6 | Shakeri et al. (15) | 2016 | N/A | N/A | N/A | 57.2 | N/A | 51.6 | 67.5% |
| 7 | Mohammadi et al. (16) | 2008 | 20 ± 6 | 74.9% R | 85.4% | 51.9 | N/A | 21.3 | 60.4% |
| 8 | Heydari (17) | 2017 | 30 - 33 | N/A | N/A | N/A | N/A | N/A | N/A |
| 9 | Ahmadi (18) | 2007 | 24.9 | 53% R | 84% | 51 | N/A | N/A | N/A |
| 10 | Alaghehbandan et al. (19) | 2011 | 26 | 54.9% R | 26.8% | 56.8 | N/A | 23.5 | 33.3% |
| 11 | Alaghehbandan et al. (20) | 2015 | 27.9 ± 14.3 | 63% R | 58% | 68.5 | 4.6% | 33 | 52.3% |
| 12 | Shojaei et al. (21) | 2014 | 30.5 | N/A | 77% | N/A | N/A | N/A | 100% |
| 13 | Ahmadi et al. (22) | 2009 | 27 | 80% R | N/A | 57 | 40% | 25 | N/A |
| 14 | Rezaie et al. (8) | 2011 | 28.9 ± 9.9 | N/A | 95.2% | 63.5 | N/A | 28.6 | N/A |
| 15 | Mohammadi et al. (23) | 2016 | 29.3 | 57.7% | Up to 70% | 67.4 | N/A | 12.2 | N/A |
| 16 | Malakouti et al. (9) | 2013 | N/A | 64.7% R | N/A | 52.2 | N/A | 47 | N/A |
| 17 | Dahmardehei et al. (24) | 2014 | 25.3 | 61.05% | 63.55% | 74.2 | 72.3% | 20 | 90% |
| 18 | Zamani, Bagheri (25) | 2013 | N/A | N/A | 73.3% | 33.3 | N/A | N/A | N/A |
| 19 | Hosseini et al. (26) | 2015 | 32.32 ± 12.8 | 47.2% R | 0 | 59.5 | N/A | 33.8 | 0 |
| 20 | Hosseini et al. (27) | 2013 | N/A | N/A | N/A | 46 | 39% | 38 | N/A |
| 21 | Khankeh et al. (28) | 2015 | 29.76 ± 10.74 | 50% R | 85.7% | 79 | N/A | 7.4 | 0% |
| 22 | Rostami et al. (29) | 2016 | 31.3 | 26.4% R | 85.7% | 47.2 | N/A | N/A | 100% |
| 23 | Karim et al. (30) | 2015 | 27.5 | N/A | N/A | 57 | N/A | N/A | N/A |
| 24 | Ahmadi et al. (31) | 2015 | 27 | N/A | 60% | 57 | 33% | 10 | N/A |
| 25 | Malakouti et al. (32) | 2014 | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 26 | Boostani et al. (33) | 2012 | N/A | 100%R | N/A | 100 | 100% | N/A | 0% |
| 27 | Ahmadi et al. (7) | 2012 | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| 28 | Suhrabi et al. (5) | 2012 | N/A | N/A | N/A | N/A | N/A | 60 - 91 | N/A |
| 29 | Mami et al. (34) | 2015 | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
Demographic and Clinical Characteristics
3.1. Prevalence and Demographic Characteristics
Studies performed on the incidence and/or prevalence of self-immolation in Iran have reported various rates for these variables in different parts of the country (10, 14, 18, 21, 23, 28). Our review showed that 1500 to 2000 people die due to self-immolation each year in Iran (34). Self-immolation accounts for 1.4% to 9.5% of suicide attempts and 25.0% - 71% of completed suicides (5, 14). According to the reports of the Forensic Organization of Iran on deaths by suicide, of total suicides recorded from 2006 to 2010, hanging was the most common method (52.5%), followed by self-immolation (16.4%) and self-poisoning (11.2%) (21, 28). Similar patterns have been reported by other studies, as well (5, 10, 27).
A study conducted in Iran reported that the incidence of self-immolation has increased from 1.48 per 100,000 population in 1998 to 7.7 in 2003 in the northwest provinces (12). However, more recent studies conducted in the southwest of the country reported a decrease in the incidence of self-immolation during 2009 - 2012 (23). Furthermore, another study has demonstrated a dramatic shift in women’s suicide during 2003 - 2014, from self-immolation among villagers and those with lower education levels to hanging in urban areas and those with higher education (12). The youngest and oldest victims of self-immolation were 18 and 30 years, respectively (Table 2) (10, 18, 36, 37). A study has reported a direct association between risk of self-immolation (compared to poisoning) and age (P < 0.007) (8).
3.2. Geographical Distribution
Self-immolation rates vary across regions of the country, with the highest rates occurring in border provinces, particularly among the Kurdish population (6, 8, 38). Ahmadi et al. (14) and Boostani et al. (33) reported that the rate of self-immolation is higher in rural areas in the western parts of Iran. While, in a study performed in the Mazandaran province (north of Iran), Zarghami et al. (10) reported higher rates of self-immolation in urban areas. Another study concluded that the incidence of self-immolation is higher in most deprived cities than in more affluent areas (12). A population-based survey on the causes of death (39) in the provinces of Iran showed that the three provinces located at the Iran-Iraq border, the most affected provinces during the Iran-Iraq war, had significantly higher rates of self-immolation (3 - 9 per 100,000 persons/year) (P < 0.05). However, this figure was 8.2 per 100,000 general population in the northern border of Iran (10). The authors categorized these provinces as those with “high” and “very high” rates of self-immolation. Provinces located at the center of Iran (e.g. Esfahan and Semnan) had low rates of self-immolation. This study has categorized the provinces of Iran based on the incidence of self-immolation into “low” (0.1 - 1 per 100,000 population), “medium” (1 - 3 per 100,000 population), “high” (3 - 7 per 100,000 population), and “very high” (≥ 7 per 100,000 population) (12). Concerning the ethnicity, self-immolation is reported to be more prevalent among Kurds (who primarily reside in Kurdistan, Kermanshah, Ilam, and some parts of the West Azerbaijan provinces), Lors, and the Torkamans (who reside in the Golestan Province). On the other hand, Turk and Baluch populations (living in the East Azerbaijan and Zanjan, and Sistan-and-Baluchestan provinces, respectively) are reported as those with the lowest risk of self-immolation (14, 17, 40).
3.3. Gender Distribution of Victims
Similar to the global pattern, self-immolation is significantly higher among females, particularly young women (8, 10, 20, 34, 36). Chronic marital conflict is reported as an important risk factor for self-immolation. Therefore, couples are at an increased risk of suicide attempts by self-immolation (P < 0.001) (18).
Since self-immolation is associated with high morbidity and mortality, it imposes a significant burden, particularly years of life lost (YLL) (10, 14, 18, 28). There are considerable differences concerning the suicide attempts and suicidal behaviors among males and females.
Self-immolation was the method of choice among women in some parts of the country. For example, in the Kurdistan Province, self-immolation is reported to be 23 times more prevalent among females than males, or 83% of the self-burning cases were women (10). In the “medium,” “high,” and “very high” provinces, self-immolation was more common among females (14). However, in the “low” provinces, most of the self-immolation cases were male (53 versus 29%, P < 0.001) (14, 21). Several studies have reported no association between suicidal attempts and not having a job (zero income) (7, 17, 22).
3.4. Level of Education
In Iran, most of the self-immolation cases were educated up to primary only. Besides, women committing self-immolation were either illiterate or had low levels of education (P < 0.001) (5, 14, 18, 22, 24, 30, 37, 41). However, in the north of Iran, most (57.3%) of the self-burning cases were educated up to high school (10). Besides, those with lower levels of education tend to use more violent methods for suicide (8). Hanging and self-immolation were more frequent among those with lower levels of education; whereas, poisoning was more frequent among those with higher educations (P < 0.0001) (21). This association is reported by almost all included studies, and more than half of these studies mentioned low education as a risk factor (Table 2).
3.5. Self-Immolation and Psychiatric Disorders
The majority of self-immolation victims had a history of psychiatric disorders (60% to 91%) (42). Various studies have mentioned psychiatric disorders, such as substance abuse, as important factors that lead to self-immolation. The most frequently reported psychiatric disorder is affective disorders (21%), followed by schizophrenia (12%) and personality disorders (7%) (10, 12, 34, 43). Some studies have placed more emphasis on adjustment disorder, particularly due to marital conflicts, and mentioned it as the most prevalent psychiatric disorder (10, 34).
3.6. Self-Immolation Outcome
Regarding the outcomes, most of the studies focused on deaths caused by self-immolation. A study that followed a particular population for 8 - 10 years has reported no case of self-immolation death. But, a suicide case, which resulted in death, by self-hanging after a self-immolation attempt is reported (37). No other outcome is reported by the included studies. The mortality rates reported for self-immolation range from 70% to 90%. Therefore, it can be considered as the most fatal method of suicide (10, 12, 26, 37). Some studies mentioned self-immolation as the third leading cause of death among Iranian women, which is more common among young married women living in rural areas (8, 21, 30). In almost all of the included articles, reported mortality rates were higher than 50% (Table 1).
4. Discussion
This study showed that, generally, women are more likely to commit suicide via self-immolation. Several factors are reported as risk factors for self-immolation, the most important of which are domestic violence and stressful events such as family conflicts. Most of the self-immolation victims had a history of psychiatric disorders, were less educated, and were married. Studies performed in various regions of Iran have reported different rates for self-immolation. These studies reported higher rates in the western and northern parts of Iran and border provinces. Self-immolation is a significant social and medical problem all around the world. Suicide by self-immolation is more frequent in developing (40.3% of all suicides) than the developed countries (0.06% - 1% of all suicides). It comprises 0.37% to 40% of total burn center admissions worldwide, and, in Iran, it ranges from 4.1% to 36.6% (5, 18).
Self-immolation is the fourth leading cause of death and the sixth leading cause of disability among people aged 15 to 44 years (1, 5).
The mean age of self-immolation victims in Iran is relatively low compared to the western countries (12). Studies have shown that the mean age of self-immolators in the world is one decade older than the corresponding age in Iran (44, 45). Several factors contribute to this issue, including arranged marriage and children’s wedding (8, 10, 18, 41, 46-49). A review study performed in Iran has reported that in border provinces, which have higher rates of self-immolation than other regions of the country, family size (5.2 versus 4.1; P < 0.05) and age at first marriage are significantly different than the national averages (P < 0.05) (14).
The results of studies on suicidal patterns about gender differences are controversial. In the present study, self-immolation was more common among females. In contrast to Iran, studies conducted in Australia and North America have shown that men committed self-immolation more than women (50, 51). This difference might be due to the fact that self-immolation is considered as a method of crying for help by women in some regions of Iran (21).
Previous studies conducted in Iran and other developing countries have reported an inverse association between self-immolation and level of education (18). Also, those with lower levels of education tend to use more violent methods for suicide, which can be attributed to poor problem-solving skills (8). Moreover, a low level of education is usually associated with lower socio-economic status (11).
There are studies that mentioned socio-economic status as an important factor that contributes to self-immolation in less developed countries, which is in line with findings of the present study, that most of the female self-immolators were from low socio-economic classes. Deprivation, poverty, and humiliation in Uzbekistan, problems related to marriage and trousseau in India, and arranged marriage in Afghanistan have been reported as the main causes of attempting self-immolation by young women (52-54).
In Iran, self-immolation is more a cultural issue rather than a religious (8). Similar to other studies, Iranian studies have also reported that there are cultural factors that increase the risk of self-immolation, including imitative acts by women who imitate self-immolation threats from their peers and sisters (8, 18). Both socio-cultural and psychiatric factors have been found to be associated with self-immolation (10). Easy access to inflammable materials may have an important role in committing suicide by self-immolation; Kerosene is the most commonly used tool (85%) for self-immolation (12).
Domestic violence is reported to be associated with self-immolation. Family conflicts, intimate relationship break-ups, divorce, and financial issues might also have a similar role (14, 34). Arranged marriage, unwanted pregnancy, being financially dependent on the husband, unfair divorce laws, unemployment, and limited job opportunities for women may bring social hopelessness in women. In this context, suicidal behaviors may be an automatic reflection, particularly in the first years of married life for women (5, 9, 24). Similar cultural factors might contribute to self-immolation in different provinces of Iran. The results of studies conducted in East Azerbaijan (41), Mazandaran (10), Kohgiluyeh-and-Boyer-Ahmad (48), Kurdistan (36), Ilam (6, 19), Kermanshah (18), Tehran (55, 56), Khuzestan (57), Lorestan (33), and Sistan-and-Baluchestan (24) suggest that tension with husband and his family has a crucial role in women’s deciding to commit self-immolation. Economic opportunities are often lower in border provinces of Iran, and, therefore, their unemployment rate is higher than the national average. Moreover, people of these provinces are usually more illiterate, suffer from higher rates of psychological distress, and have limited access to health facilities. Furthermore, in these regions, divorce is associated with a high stigma, and women feel uncertain about their future. Overall, studies have shown that almost all border areas of Iran suffer from a high prevalence of self-immolation, compared to central regions of the country. Future studies are needed to elaborate on this phenomenon and understand its underlying mechanism. Self-immolation in Iran particularly affects young married women living in rural areas (8, 41, 47, 48, 58), and 73% of self-immolation cases occur in families with physical or verbal aggression (24).
The findings of the present revealed that although mental disorders may contribute to deciding to commit suicide, but social and cultural issues seem to better predict self-immolation. This finding is somehow inconsistent with studies conducted in western countries, in which major depressive disorder, psychosis, alcoholism, and drug use disorders were strongly associated with suicide (59-63).
In many countries, self-immolation is a type of radical political protest. For example, during the “Arab Spring” in recent years (64). Our review revealed no association between a particular political challenge and self-immolation in Iran. The present study had limitations. First of all, due to the limitation of data, we couldn’t perform a meta-analysis. Also, there were differences between the included studies concerning the sampling method, data collection instruments, and methods applied to assess the outcomes. We limited the data collection process to studies performed on women in Iran.
5. Conclusions
This study demonstrated that the prevalence of self-immolation is relatively high among Iranian women, compared to other countries. Although studies have reported different rates for self-immolation in various regions of the country, it can be argued that this harsh method of suicide roots in similar cultural and socio-economic factors. While the current study highlighted the specific and contextual factors associated with self-immolation, future studies benefiting from high-quality methodology are necessary to increase understanding of this phenomenon and perhaps to develop prevention measures.