1. Context
Infertility is defined as the inability of a non-contracepting, sexually active couple to achieve pregnancy in one year (1). Of all infertility cases, approximately “50% is due to female factors alone, 20% - 30% due to male factors alone, and the remaining (20% - 30%) is due to a combination of male and female factors” (2). It is also estimated that approximately 72.4 million couples are infertile worldwide (3). Infertility is a common problem among couples worldwide and is estimated to affect 10% to 15% of couples (4). In Iran, the prevalence of infertility is approximately 17.3% (5).
As a serious crisis, infertility can affect different aspects of infertile couples’ life (6) and cause a broad range of social, psychological, physical, and financial problems (7, 8). Mental problems are frequently observed in infertile couples, which can be affected by many factors, such as culture, gender, duration of infertility, cause of infertility, and therapeutic methods (8, 9). The World Health Organization (WHO) defined infertility as a global problem in fertility health, which affects the mental health of infertile couples through frustration, stress, anger, depression, isolation, anxiety, feelings of guilt, sexual and marital problems, lack of self-confidence, etc. (10).
Also, psychological problems caused by infertility can be an aggravating factor for infertility (11). Infertility diagnosis examinations and relevant therapeutic processes are among risk factors for anxiety and depression in 20% - 40% of infertile women. Psychological consequences of infertility remain in 20% of infertile women even after successful treatment (12, 13).
Guz et al. investigated mental symptoms in infertile women and showed that the rates of depression and anxiety were higher in infertile women than the fertile couples; in addition, they also found that the rates of depression, anxiety, and low self-confidence increased with aging and prolonged infertility (14). Another study reported a high prevalence of mental problems, specifically generalized anxiety disorder (GAD), among infertile couples, particularly women, which considerably affected their quality of life. Such consequences affect infertile couples’ lives (15). According to the study by Hasanpour et al. (2014), the mean total mental health and anxiety scores of infertile women were 29.70 ± 11.50 and 6.29 ± 4.17, respectively, whereas the subscale of depression scored 3.58 ± 4.11 indicating the adverse mental health status of Iranian infertile women (16). Infertility is associated with psychological pressures and negative behaviors as risk factors for in vitro fertilization with intracytoplasmic sperm injection (IVF/ICSI) outcomes (17). Anxiety can worsen infertility conditions by increasing the secretion of cortisol and prolactin (18). Many mechanisms have been suggested for the effects of psychological pressures on fertility, including inhibition of gonadotropin secretion, local effect of catecholamine on the uterus and function of uterine tubes, and disruption of immunological processes involved in the preservation of fertility and implantation (19). As an unwanted and unplanned stressor, diagnosis with infertility challenges infertile couples’ expectations of life as many couples have no adequate knowledge and skill regarding the proper management of infertility (20, 21).
Cognitive behavioral therapy (CBT), highly effective intervention with short-term effects, reduces anxiety and depression in infertile couples and enables them to achieve general mental health through identifying and challenging their illogical behaviors and thoughts (22). CBT counseling helps clients to develop skills required for behavior change, development of relationships, problem-solving, harmful belief and attitude change, and cognitive reconstruction (23). The effectiveness of CBT has shown in improving anxiety in some cases. For example, CBT was reported effective in women undergoing intrauterine insemination (24) and also cases with anxiety and depression. It was also reported effective in raising hope in women with breast cancer by identifying negative schemes and using downward arrow techniques (25).
A study showed that CBT, as an experimental treatment method, is very effective in improving anxiety disorder and reducing anxiety levels (26).
Another study showed that the continuous application of CBT techniques on infertile women, who did not have a medical or physical problem, reduced anxiety, depression and psychological symptoms and even led to pregnancy in some cases (27).
This study was conducted to determine the effect of CBT on anxiety and depression of Iranian infertile women for the following reasons:
i. There is a high prevalence of mental disorders among infertile couples (15).
ii. Although different reviews (28-31) in other countries have investigated the effect of CBT as a psychological intervention on anxiety and depression of infertile couples, no Iranian investigation has addressed the effect of variables, such as culture on Iranian women in reacting to their infertility.
2. Objectives
This study aimed at determining the effect of CBT on anxiety and depression in Iranian infertile women focusing on preventing mental problems.
3. Data Sources
To find relevant studies published until February 20, 2019, national and international databases, such as Magiran, Iranmedex, SID, Medline (via PubMed), Scopus, Google Scholar, Embase, Cochrane Library, and Web of Sciences were independently searched by two researchers without any time limit. Finally, references of selected articles were used to find other relevant studies. As some of the Iranian databases showed no sensitivity to search operators (AND, OR, NOT), the search was done only through Persian keywords, including cognitive-behavioral therapy, infertility, infertile couples, anxiety, depression, and systematic review. To search English databases, keywords containing, Iranian Infertile Couples, Anxiety, Depression, Cognitive Behavior Therapy, Systematic Reviews together with their equivalents in Mesh and combining words with AND and OR functions were searched using search operators.
4. Study Selection
The present study reviewed all Iranian controlled randomized clinical trials on the effect of CBT on anxiety and depression. The population intervention comparison and outcomes (PICO) tool was used to identify components of clinical evidence. In the selected studies, participants were Iranian infertile women. The used intervention was the application of CBT, the control group had received only routine care, and the outcomes were anxiety and depression.
5. Data Extraction
Two authors separately investigated the acceptability and quality of articles and any disagreement was solved through consensus and a third opinion. Data regarding time, place, methodology, number of randomized participants, attrition rates during follow-up, outcomes, and results were extracted and then recorded on a checklist designed by the research team.
5.1. Assessment of the Risk of Bias
Two researchers separately evaluated the risk of bias based on the Cochrane Handbook in terms of allocation sequence concealment, blinding of participants, personnel, and outcome assessors, incomplete outcome data, and selective reporting bias.
6. Data Analysis
Review Manager (RevMan) 5.3 was used for meta-analysis and plotting the risk of bias diagrams and because different instruments were used to measure desired variables, the standardized mean difference was reported instead of the mean difference. Moreover, due to a high level of heterogeneity of the included studies, the “random effect” was used instead of the “fixed effect.”
7. Results
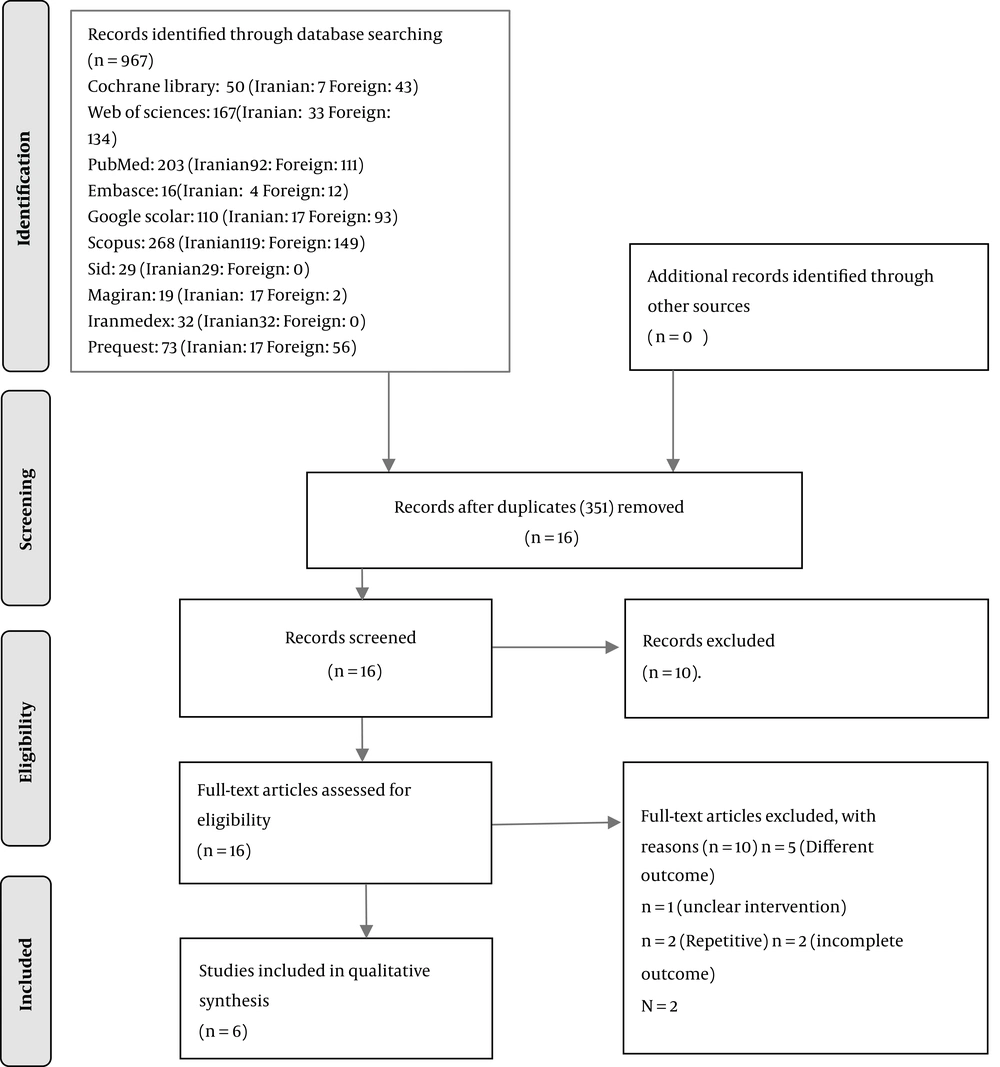
Iranian studies included 367 out of 973 articles. However, 351 Iranian articles were excluded because of irrelevancy, non-interventional methodology, and duplication. Out of the remaining 16 articles, five articles were excluded because they did not assess the desired outcome, and one article was excluded because the employed psychological intervention was not mentioned. Moreover, since two studies conducted by Mosalanejad et al. had the same registration codes at the Iranian Registry of Clinical Trials with similar outcomes, the study with a greater sample size was selected for the meta-analysis. Since two studies conducted by Faramarzi et al. had similar outcomes and sample size, only one study was included. Although studies conducted by Javdani et al. (32) and Khalatbari et al. (33) were analyzed for bias, they were not included in the final analysis as the mean values had not been reported and the authors did not respond to our email, as well. Finally, six clinical trials were included for a meta-analysis (Table 1 and Figure 1).
| Authors, Years | Country | Study Design | Study Period | Sample Size | Study Population | Intervention/Treatment | Comparator | Outcomes | Result |
|---|---|---|---|---|---|---|---|---|---|
| Mosalanejad et al. 2012 (34) | Iran | RCT | 3 months | 65 | All women with primary infertility | CBT (group meeting) | Routine care | Depression and anxiety | CBT significantly decreased depression and anxiety |
| Hamzeh Pour 2014 (35) | Iran | Experimental research with pretest posttest design and control group | CBT was conducted through eight 90-min sessions | 30 | All women who had referred to the Mehr Proffetionl Clinic during 4 months in Rasht” | CBT | Routine care | Anxiety | Anxiety in the experimental group was less than the control group |
| Heidari et al. 2002 (24) | Iran | RCT | From May to August 2001 | 110 | All women who had referred for IUI treatment | CBT | Routine care | Anxiety | CBT was effective |
| Nilforooshan et al. 2006 (36) | Iran | “Quasi-experimental research with pre-test post-test design and experimental group” | The intervention was performed for six sessions (once a week) | 30 | All women who had referred to a Fertility and Infertility Center in Isfahan | Cognitive-behavioral counseling meeting based on Interacting Cognitive Subsystems (ICS) | Routine care | Depression | CBT was effective |
| Talaie et al. 2014 (37) | Iran | RCT | CBT was performed in 10 sessions (weekly) in 2011 | 30 | Infertile women who referred to the Monteserie Fertility Treatment Hospital in Mashhad for a month (from mid-September to mid-March 2011) | CBT | Routine care | Depression | CBT significantly decreased depression |
| Faramarzi et al. 2008 (38) | Iran | RCT | September 2006 to June 2007 | 82 | Women who had been trying to conceive for more than 2 years | CBT | Routine care | Depression and anxiety | CBT significantly decreased depression and anxiety |
| Khalatbari et al. 2011 (33) | From the late July 2010for 3 consecutive months (90 minutes per week) | 30 | Infertile women referring to the Mehr Infertility Clinic in Rasht city for 4 months in 2010-2011 | CBT | Routine care | Depression and anxiety | CBT significantly decreased depression and anxiety | ||
| Javedani et al. 2017 (32) | Iran | RCT | Quasi-experimental research with pre-test post-test design and control group | 30 | All infertile women who had referred to the Healthcare and Medical Centers of Mashhad in 2015 | Mindfulness-based cognitive therapy (MBCT) | Routine care | Depression and anxiety | In the intervention group, depression and anxiety significantly decreased |
Characteristics of the Included Studies
Two studies had been conducted in Mashhad (24, 37), one study in Jahrom (34), one study in Rasht (35), one study in Babol (38), and one study in Isfahan (36).
The sample size varied from 30 (35-37) to 110 participants (24). Different instruments had been used for the assessment of depression and anxiety. Depression had been assessed using the Beck Depression Inventory (BDI) in two studies (36, 37), through the Depression, Anxiety, and Stress Scale (DAS) in one study (34), and General Health Questionnaire (GHQ) in one study (38).
Anxiety had been assessed using Kettle’s Anxiety Questionnaire in one study (35), Spielberger Questionnaire in one study (24), Depression, Anxiety and Stress Scale in one study (34), and General Health Questionnaire (GHQ) in one study (38).
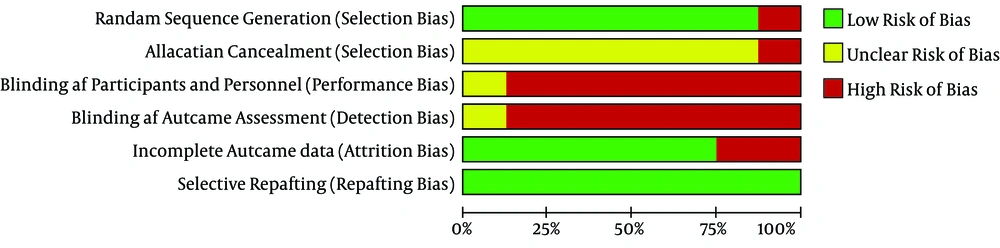
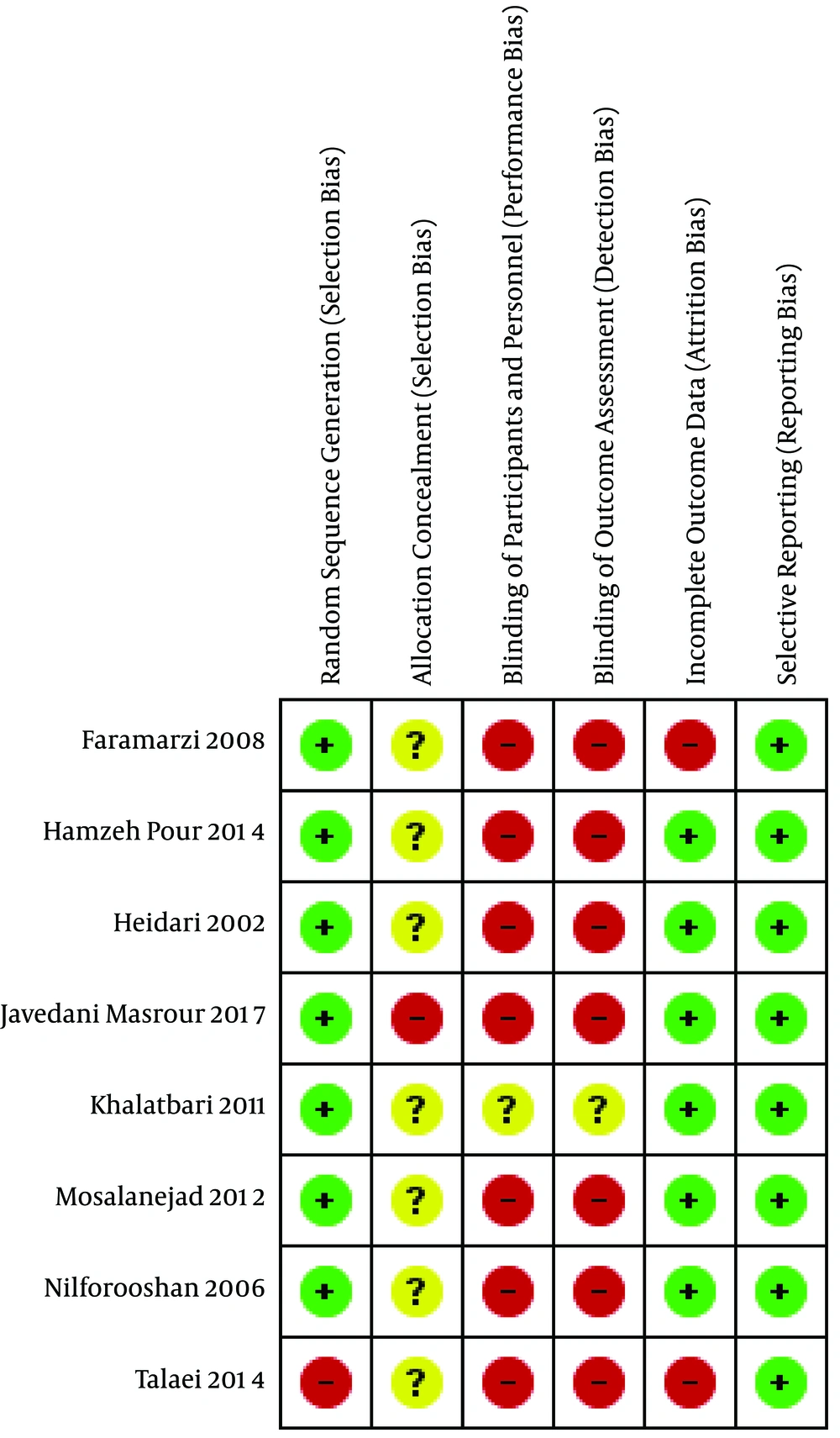
The risk of sequence bias was high in two studies (32, 37) and low in six studies (24, 33-36, 38). The blinding status of study participants and personnel and also the risk of bias from blinding of outcome assessment were high in all eight studies (24, 32-38). The risk of incomplete outcome bias was high in two studies (37, 38), unknown in one study (33), and low in five studies (24, 32, 34-36). The risk of selective reporting bias was low in all studies (24, 32-38) (Figures 2 and 3).
7.1. Meta-Analysis Results
7.1.1. Depression
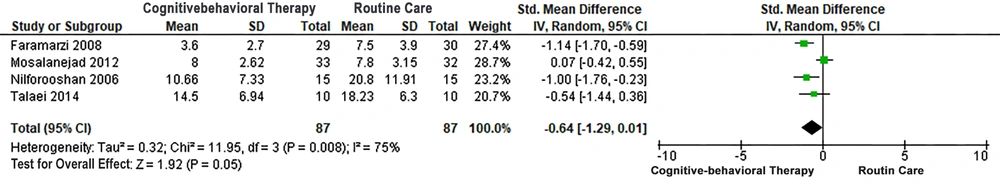
According to the meta-analysis results, the mean score of depression in the CBT group was lower than the control, whereas the heterogeneity was higher (I2 = 75%; Tau2 = 032; Chi2 = 11.85, P = 0.008); however, this between-group difference was not significant (SMD = -0.64; 95% CI: -1.28 to 0.01 P = 0.05) (Figure 4).
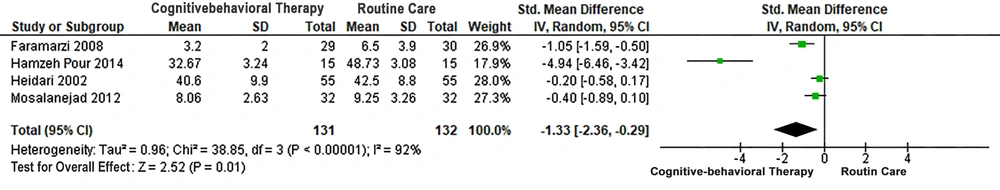
7.1.2. Anxiety
The mean anxiety score in the CBT group was significantly lower than the control, whereas the heterogeneity was higher (I2 = 90%; Tau2 = 0.96; Chi2 = 33.85, P < 0.00001) and this between-group difference was significant (SMD = -1.33; 95% CI: -2.36 to -0.29 P = 0.01) (Figure 5).
Khalatbari et al. (33), showed that CBT significantly reduced depression (P = 0.0005) and anxiety (P < 0.0005). In Javedani et al. (32) study, the rates of anxiety and depression were lower in the CBT group than the controls.
8. Discussion
The present study is the first systematic review and meta-analysis on the effect of CBT on anxiety and depression in Iranian infertile women. The meta-analysis results showed that anxiety in infertile women undergoing CBT was significantly lower than the control group; however, it was not significant for depression, which can be due to the confounding factors, such as the lack of screening for those with depression. This is because the treatment of depression by CBT plus medication seems to produce better results than CBT alone (39, 40).
In a review, Cuijpers et al. (41) showed that psychotherapy was more effective in European countries than in other countries. Therefore, the insignificant between-group difference in this study can be due to the cultural differences between Iran and European countries.
Moreover, two studies (34, 36) had been conducted only on individuals with initial infertility with a very high level of depression (42). As a result, it can be regarded as a confounding factor. In other studies, the type of infertility had not been mentioned.
In a review, LoGiudice and Massaro (2018) had shown that CBT was effective in reducing anxiety, depression, and stress, and increasing infertility quality (29). The results of our meta-analysis are partially consistent with studies on women undergoing IVF; however, CBT showed no significant effect on depression in the present study.
Frederiksen et al. (2015) in a review and meta-analysis showed that the psychological interventions, especially CBT, are effective in improving infertility and also in reducing psychological depression and improving clinical pregnancy (30). The results of a meta-analysis by Hammerli et al. did not indicate the effectiveness of psychological interventions in improving mental health (depression and anxiety) of infertile men and women; however, the advantages of psychological interventions on infertility have been reported (28). House (2011), reported that continuous CBT reduced the anxiety, depression and psychological symptoms in infertile women with no certain medical and physical cause, and resulted in pregnancy in some of the cases after a while (27). Their results are consistent with ours in terms of anxiety and inconsistent in terms of depression.
Some studies have shown promising results regarding the effectiveness of pharmaceutical and non-pharmaceutical interventions on infertility treatment. In this regard, Noorbala et al. showed that psychological interventions improved mental health and increased the chance of fertility (43). Due to the high level of depression and anxiety in infertile women (44, 45), special attention should be paid and appropriate treatments should be provided. CBT effectiveness in reducing anxiety and depression (46, 47) has made this technique as an appropriate approach to improve mental health in infertile people and also alleviate their infertility problems.
In fact, CBT can reduce the level of anxiety, depression, and other psychological problems by focusing on attitude, identifying and correcting cognitive distortions, modifying thinking skills, and assessing negative judgments and thoughts (35).
Future studies are recommended to hold follow-up sessions to ensure the long-term effects of this intervention (37) for the following limitations of this study:
Small sample size due to attrition because of no use of some CBT techniques, lack of corporation of some participants in completing the post-test forms, examination of the samples from the beginning of the treatment to the end of intrauterine insemination (IUI) operation, lack of follow-ups for positive pregnancy test result (24, 35), and time limit (37).
It is also recommended to conduct some studies on the effects of CBT on the success of assisted reproductive techniques and its effects on anxiety and depression of people undergoing infertility treatment until observing fertility test result.
8.1. Strengths and Weaknesses of the Study
Thestrength of this study was its methodology for a thorough search using many keywords along with the manual search. Among the weaknesses of the study was using convenience sampling and a small sample size in assessed studies, which affected its generalizability. The blinding of participants and personnel, as well as blinding of outcome assessment bias were at high levels in all eight studies.
9. Conclusion
Our results indicated the effectiveness of CBT intervention in reducing anxiety and depression in infertile women. However, the between-group difference was not significant in terms of depression. It is also recommended to conduct clinical trials with larger sample size and accurate methodology to obtain more generalizable results.