1. Background
As a natural and enjoyable life experience (1, 2), pregnancy may be accompanied by many physiological and psychological changes (1). These changes make women susceptible to mental disorders (3). Anxiety disorders are among the most common disorders, with a prevalence of 4.4 to 39% (4, 5). In Iran, the prevalence of anxiety disorders has been reported to be 15% (6). Anxiety, as a syndrome relatively distinct from other mental illnesses, reflects concerns about the child’s health and well-being, childbirth and its consequences, and accepting a parental role (7). Anxiety is an unpleasant mental state associated with physical discomfort such as headache, stomachache, shortness of breath, palpitation, restlessness, excitement, stress, and panic (8). However, anxiety is a condition that any person might experience due to pressures or environmental stress (9). Anxiety is considered as one of the most dangerous psychological disorders due to its harmful effects on the mother’s and fetus’s health (10). Anxiety increases in the first and third trimester due to increased estrogen levels and approaching delivery time, respectively, but decreases in the second trimester due to adaptation to physiological changes in pregnancy (11). Female perceptions of pregnancy, delivery pain, fear of delivery, marital satisfaction, physical violence of husband as well as low economic status and education are factors influencing pregnancy anxiety (2).
Maternal anxiety can lead to preterm labor, fetal death (12), intra uterine growth retardation (13), sleep problems (14), attention deficit hyperactivity disorder (15), fetal weight loss (16), crying, restlessness, and low mental development of the infant (17). Hormones such as catecholamines cause placental artery contraction, which restricts fetal oxygen supply and nutrition, and by passing the placenta, catecholamines affect fetal brain development (18), causing developmental and psycho-cognitive disorders in infants (19). Also, high levels of anxiety during pregnancy make the child susceptible to future schizophrenia and affective disorders (20). On the other hand, affecting the adrenal, pituitary-hypothalamic, and sympathetic nervous systems, stress, and anxiety lead to neuronal and endocrine changes, increasing in plasma levels of cortisol through secreting cortisol and adrenocorticotropin hormones (21). Since cortisol is high in anxious pregnant women and there is a high correlation between maternal and fetal cortisol concentrations, it rapidly affects the fetus, impairs fetal development, and decreases fetal heart rate variability (22, 23).
There are various therapies for pregnancy anxiety including behavioral therapy (24), music therapy (25), mindfulness (26), relaxation techniques (27), counseling (1), spiritual counseling (28), education (29), and distraction techniques (30), each performed in the form of individual therapy (31) or group therapy (32). Non-pharmacological methods such as writing therapy are among the ways to deal with anxiety (33, 34). Writing therapy is the art of disclosing emotions through writing (35). In this counseling approach, ambiguous and unsubstantiated feelings turn into meaningful words, raising one’s awareness of fears in one’s life (36). Writing leads to the cohesion of emotions and also to their evaluation and management, according to one’s experiences. It also changes one’s attitude toward stressful events, resulting in positive effects on physical and mental health as well as on overall physiological performance (37). Previous therapists used this approach for post-traumatic stress disorder control, schizophrenia treatment, memory enhancement, pain reduction, creativity enhancement, and acute and chronic anxiety treatment (38).
2. Objectives
Because of sensitive emotions during pregnancy associated with the fear of pharmacotherapy and the importance of mental health and also due to the cost-effectiveness of writing therapy, the researchers investigated the effect of this method on the reduction of pregnancy anxiety and its implications for improving quality of life and physical health.
3. Methods
3.1. Participants and Study Design
The present randomized controlled trial was conducted on pregnant women visiting health centers in Tabriz, Iran, from September to December 2018.
Inclusion criteria included pregnant women with a gestational age between 28 - 31 weeks, first or second pregnancy, moderate anxiety based on the Beck anxiety inventory (BAI), and education of at least high school. Exclusion criteria included mental illness, any psychotropic drug use, alcohol addiction, and cigarette smoking that all were assessed by self-reported questions; high-risk pregnancies suffering from high levels of stress and anxiety, such as pregnancies affected by diabetes, cancer, hypertension, kidney disease, and epilepsy; multiple pregnancy; personal or family history of congenital anomalies and a history of preterm labor; mothers with no plan to take care of their infants for any reason after childbirth, such as divorced or surrogate mothers; and mothers with a previous child suffering from a known physical or mental health problem.
This study was a part of a large ongoing trial, entitled “the effect of writing therapy of anxious pregnant women on the quality of their neonates’ sleep”, in which pregnancy anxiety was assessed as a secondary outcome. A total of 33 pregnant women were determined using the G-Power software based on the results of Mirjam et al.’s study on anxiety (39), with m1 = 48.5 (the pre-intervention anxiety score), a default 10% intervention-induced reduction in the mean anxiety score (m2 = 43.6), SD1 = SD2 = 4.8, two-sided α = 0.05, and power = 95% with a 20% attrition. In this study, 35 participants were evaluated in each group.
3.2. Sampling
Tabriz has 80 health centers, and sampling was conducted in 12 crowded health centers for people of various socio-economic levels. The family health department of the East Azerbaijan Province introduced the crowded centers based on the number of pregnant women covered in the health centers. The health centers were selected based on their locations in low-, middle- and high-income areas (four centers from each area) to represent different socio-economic conditions. After obtaining permission from the Ethics Committee of the Tabriz University of Medical Sciences (code: IR.TBZMED.REC.1397.408), submitting the study in the Iranian Registry of Clinical Trials (code: IRCT20120718010324N45), and coordinating and obtaining permission from the health centers in Tabriz, sampling was conducted from 1st September to 15th December 2018. During this time, the authors attended these centers, selected pregnant women with a gestational age between 28 - 31 weeks from the records of pregnant mothers at each center, and made telephone calls after reviewing the inclusion and exclusion criteria. Then, a brief description of the research objectives was provided, and individuals who were eligible and interested in participating in the study were invited to visit the intended health centers.
The interested participants visited the centers to complete the BAI. Women with severe and mild anxiety were excluded from the study, and only those with a score of 16 to 25 (moderate anxiety) were included. Afterward, written informed consents were obtained from the participants, who then completed the socio-demographic characteristics questionnaire. Women with severe anxiety were referred to a psychiatrist.
3.3. Randomization
The participants were assigned to an intervention group and a control group using block randomization with a block size of four and six and a 1:1 allocation ratio. Random allocation to the groups was conducted by an individual not involved in the study using similar opaque envelopes. The envelopes were opened by the researcher and the assistant researcher in the presence of the participants to allocate them to the intended group.
3.4. Intervention
Three protocol-based writing therapy sessions in the groups, each including 3 - 6 individuals, were held at weeks 28 - 31, 32 - 35 (two to four weeks after the first session), and 34 - 37 of gestation (two weeks after the second session).
The first session was held at week 28 - 31 of gestation. It was run to communicate with all the participants, build intimate relationships with them, and gain their trust. The concept of anxiety and factors affecting it, as well as disadvantages of anxiety and its impact on mothers, were discussed at the meeting. For the next meeting (four weeks later), the clients were then asked to list anxiety-inducing factors and their worries on a piece of paper, and write their solutions in front of each factor. The first telephone consultation (for about 15 minutes) was held two weeks after the first session (at 30 - 33 weeks). In this follow-up call, the author examined the assignments and encouraged and motivated the participants to accomplish their tasks. The second session was performed between 32 - 35 weeks of gestation. In this session, first, the assignments were reviewed. Then, the anxiety-inducing factors reported by the women were discussed in a group setting, and their strategies were analyzed. Next, each participant was asked to write a story about their problem for the next session, recount causes of their anxiety and the origin of their problem, and apply strategies based on what they learned in previous sessions. The participants were asked to seek guidance from the researcher if they had any problems. The second telephone session was a week after this meeting. In the second telephone call, the author answered the women’s questions and assessed their ability to manage their anxiety relative to the baseline. The third session was held at weeks 34 - 37 of gestation. Similar to the previous session, first, the assignments were evaluated, and then, a group discussion was conducted about them. Afterward, the participants were asked to choose the best solution getting from their groupmates brainstorming. and discuss their reasons. At the end of the third session, the mothers completed BAI. It was attempted to adhere to all the principles of counseling as much as possible during all the sessions. The control group only received routine pregnancy care.
3.5. Data Collection Tools
Data collection tools used in the present study were the socio-demographic characteristics questionnaire and BAI that were completed by the participants.
The socio-demographic characteristics questionnaire included questions about age, education, spouse’s age, and education, occupation of wife and husband, income, number of pregnancies, and type of pregnancy (intended or unintended).
BAI specifically measures the severity of clinical anxiety symptoms in people. BAI is an inventory designed to measure the severity of anxiety in adolescents and adults. It is a 21-item scale, in which the participant chooses one out of four options, indicating the severity of their anxiety. The four options for each question are scored on a Likert scale from 0 to 3. Each of the items describes one of the most common symptoms of anxiety (mental, physical, and phobic symptoms). Therefore, the total score of this questionnaire is between 0 and 63. A score of 0-7, 8 - 15, 16 - 25, and 26 - 63 indicates no to minimum anxiety, mild anxiety, moderate anxiety, and severe anxiety, respectively. This questionnaire is highly valid. Types of validity, including the face, content, and construct validity, were assessed for this test, all of which indicate the high performance of this tool in measuring the severity of anxiety. An alpha coefficient of 0.92, a reliability coefficient of 0.75 with a one-week test-retest, and a correlation rate between 0.30 and 0.76 for the items were reported (40). Kaviani et al. (41) assessed the psychometric properties of the Persian version of BAI. The results showed that the inventory had good test-retest reliability (r = 0.72) and internal consistency (Alpha= 0.92).
3.6. Data analysis
The data were analyzed using SPSS 24. The Kolmogorov-Smirnov test confirmed the normality of the quantitative data. Chi-square, chi-square for trend, independent t-test, and Fisher’s exact test were used to assess the consistency of the two groups in terms of socio-demographic characteristics. Moreover, an independent t-test was used to compare the mean score of anxiety in the study groups before the intervention, and ANCOVA was used after the intervention with adjustment of baseline values as a possible confounding variable.
4. Results
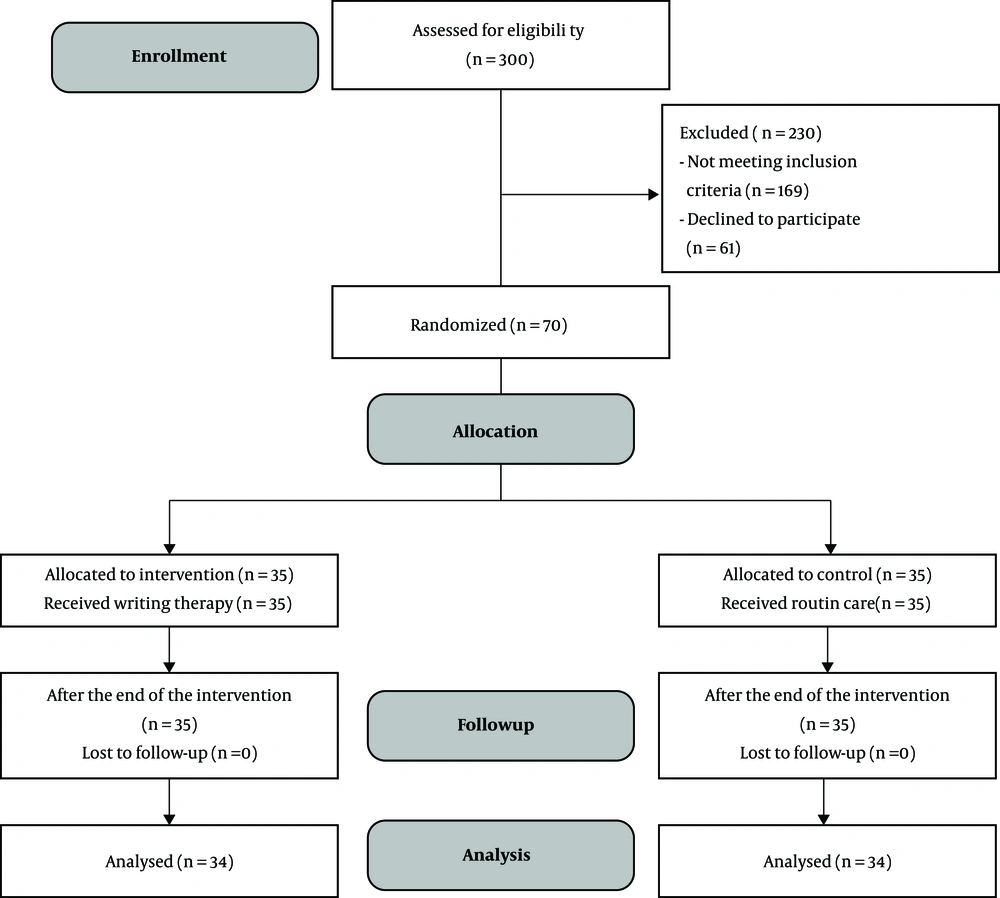
Of the 300 pregnant women evaluated, 70 met the inclusion criteria and accepted to participate in the study. They were thus allocated randomly to the study groups. The others (n = 230) were excluded from the study because of unwillingness, high-risk pregnancies, third and more pregnancies, and lack of education or inability to write. There was only one loss in each group due to lack of access, and the data of 34 participants in each group were statistically analyzed (Figure 1).
According to the socio-demographic characteristics of the participants, there was no significant difference between the two groups. The mean age (SD = standard deviation) of the women and their spouses was 27.5 (5.9) and 33.3 (5.5) in the intervention group and 27.7 (5.8) and 33.2 (5.4) in the control group, respectively. About half of the participants in the intervention (45.7%) and control (42.9%) groups had a diploma. The majority of women in both groups were homemakers. More than two thirds (68.6%) of mothers in both groups reported that their spouses were self-employed. More than half of the mothers (68.6% in the intervention group and 57.1% in the control group) stated that their family income was, to some extent, adequate for living expenses. The majority of women in both groups (94.3% in the intervention group and 97.1% in the control group) had a normal pregnancy. About half of the participants in the intervention (51.4%) and control (57.1%) groups were experiencing first pregnancy. The majority of women in both groups (76.5% in the intervention group and 86.7% in the control group) reported the type of their previous delivery as vaginal. About one-third of women in both groups (37.1% in the intervention group and 34.3% in the control group) were satisfied with life. The mean (SD) number of family members was 2.8 (1.0) in the intervention group and 2.5 (0.7) in the control group (Table 1).
| Variable | Intervention Group (N = 35) | Control Group (N = 35) | P Value |
|---|---|---|---|
| Woman’s age, y | 27.5 ± 5.9 | 27.7 ± 5.8 | 0.888b |
| Spouse’s age, y | 33.3 ± 5.5 | 33.2 ± 5.4 | 0.948b |
| Woman’s education | 0.847c | ||
| High school | 9 (25.7) | 11 (31.4) | |
| Diploma | 16 (45.7) | 15 (42.9) | |
| Academic education | 10 (28.6) | 9 (25.7) | |
| Spouse’s education | 0.354c | ||
| Under high school diploma | 11 (31.4) | 16 (45.7) | |
| High school diploma | 16 (45.7) | 9 (25.7) | |
| Academic education | 8 (22.9) | 10 (28.6) | |
| Woman’s job | 1.000d | ||
| Homemaker | 32 (91.4) | 33 (94.3) | |
| Working at home other than homemaking | 1 (2.9) | 1 (2.9) | |
| Working outside the home | 2 (5.7) | 1 (2.9) | |
| Spouse’s job | 0.542d | ||
| Unemployed | 1 (2.9) | 0 (0) | |
| Worker | 4 (11.4) | 2 (5.7) | |
| Employee | 6 (17.1) | 9 (25.7) | |
| Self-employed | 24 (68.6) | 24 (68.6) | |
| Income | 0.241c | ||
| Not enough | 6 (17.1) | 5 (14.3) | |
| Somewhat enough | 24 (68.6) | 20 (57.1) | |
| Enough | 5 (14.3) | 10 (28.6) | |
| Type of pregnancy | 1.000d | ||
| Natural | 33 (94.3) | 34 (97.1) | |
| Assisted reproductive techniques | 2 (5.7) | 1 (2.9) | |
| Number of pregnancy | 0.745d | ||
| One | 18 (51.4) | 20 (57.1) | |
| Two | 17 (48.6) | 15 (42.9) | |
| Type of previous delivery | 0.659d | ||
| NVD | 13 (76.5) | 13 (86.7) | |
| C/S | 4 (23.5) | 2 (13.3) | |
| Pregnancy desire | 0.218d | ||
| Yes | 26 (74.3) | 31 (88.6) | |
| No | 9 (25.7) | 4 (11.4) | |
| Life satisfaction | 0.917c | ||
| Absolutely satisfied | 13 (37.1) | 12 (34.3) | |
| Somewhat satisfied | 12 (34.3) | 14 (40) | |
| Neutral | 6 (17.1) | 4 (11.4) | |
| Somewhat dissatisfied | 2 (5.7) | 3 (8.6) | |
| Absolutely dissatisfied | 2 (5.7) | 2 (5.7) | |
| Family member number | 2.8 ± 1.0 | 2.5 ± 0.7 | 0.215b |
aValues are expressed as No. (%) or mean ± SD.
bIndependent t-test.
cChi-square for the trend test.
dFisher’s exact test.
The results of the independent t-test showed no significant difference in the mean (SD) score of pre-intervention anxiety in the intervention 19.3 (3.3) and control 18.5 (2.8) groups (P = 0.287). The mean (SD) score of anxiety was 13.2 (5.2) and 19.4 (5.2) in the intervention and control groups, respectively, six weeks after the intervention. According to ANCOVA with baseline score adjustment, the score of anxiety had a significant reduction in the intervention group compared to the control group (adjusted mean difference: -6.8; 95% confidence interval: -9.1 to -4.5; P < 0.001) (Table 2).
| Variable | Intervention Group (N = 35) | Control Group (N = 35) | MD (95% CI) | P Value |
|---|---|---|---|---|
| Total anxiety (Score: 0 - 63) | ||||
| Before the intervention | 19.3 ± 3.3 | 18.5 ± 2.8 | 0.8 (-0.6 - 2.2) | 0.287 |
| Six weeks after the intervention | 13.2 ± 5.2 | 19.4 ± 5.2 | -6.8 (9.1 - 4.5) | < 0.001 |
Abbreviation: MD (95% CI), mean difference (95% confidence interval).
aValuess are expressed as mean ± SD.
bFor comparison of the groups before the intervention, an independent t-test was used, while for comparison of the groups after the intervention, ANCOVA was used by adjusting the baseline score.
5. Discussion
This study was conducted to investigate the effect of writing therapy on anxiety scores of pregnant women visiting health centers in Tabriz, Iran. The results showed that writing therapy had a significant positive impact on reducing anxiety scores during six weeks of intervention compared to the control group.
Crawley et al. (42) conducted a study to investigate the feasibility and acceptance of writing therapy in postpartum women. In this study, 865 postpartum women (6 - 12 weeks postpartum) were divided into three groups of controlled writing therapy based on the researcher’s instructions, i.e., writing and disclosure of personal emotions, and control. Subjects in both intervention groups were required to complete their writing assignments within three consecutive days for 15 minutes. The results showed that the writing and disclosure of personal emotions groups had the least anxiety one and six months after the intervention (42). The results of a randomized controlled trial by Hasanzadeh et al. (43) on 80 patients with multiple sclerosis (MS) showed that writing emotional expression was effective on anxiety and stress scores in patients with MS one month after the intervention. In the study by Horsch et al. (44) in Lausanne, Switzerland, 120 postpartum women were allocated to control and intervention groups with writing therapy. The intervention group wrote their emotions within three consecutive days for 15 minutes. The intervention was performed on mothers whose children were still alive three months after the birth of a preterm infant. The author measured mothers’ anxiety four and six months postpartum.
The results showed that the level of depression and post-traumatic stress decreased significantly in the intervention group compared to the control group at the end of the intervention and 6 six months postpartum (44). Moradmand et al. (45) showed in their study that written emotional disclosure reduced anxiety scores of students undergoing writing therapy compared to the control group. The results of the above studies are in line with the results of the present research. Writing about traumatic events leads to reduced anxiety and depression by reducing negative emotions. Moreover, writing about negative emotions enables one to make sense of one’s vague feelings in the mind. Being aware of these emotions empowers one to overcome them, resulting in reduced anxiety (43).
In a study by Panagopoulou et al. (46), 148 women undergoing infertility treatment at the Aristotle University of Thessaloniki in Greece were allocated to emotional disclosure writing, reality writing, and control groups. The aim was to investigate the effect of disclosing emotions on these women using writing therapy. The results showed that the anxiety score was not significantly different between the three groups, and, more interestingly, the infertility treatment was more successful in the control group than in the other groups (46), which is not consistent with the present study. Perhaps the reason for the discrepancy is the difference in the number of counseling sessions and type of emotions disclosed, as in the present study, counseling was performed in three in-person and two telephone sessions. The participants in our study were asked to disclose their emotions soon after becoming upset. However, participants in the above study were asked to write about the problems they experienced with infertility. Writing in the short period revives negative memories and affects the mood, but in the long period, it reinforces positive emotions (47). Further, in a pilot study, Anderson et al. (48) examined the effect of emotional disclosure on rape victims. To this purpose, 670 American students with a history of rape were examined. The results showed that the post-traumatic stress score was not significantly different between the two groups one month after the intervention. However, there was a significant difference between the two groups by continuing the treatment and in the third month after the intervention in favor of the intervention group (48), which is not consistent with the present study. Perhaps the reason for this disagreement is the severity of psychological trauma caused by rape, which takes longer to be healed. However, in the present study, women with moderate anxiety were assessed.
Writing transforms meaningless words and emotions into meaningful and comprehensible words. What is unseen and invisible is more frightening and scary, which reduces awareness of the event criticality (38, 49, 50). Moreover, since people are not exposed to face to face encounters, expressing their emotions, fears, and shames not being confirmed by others, this approach could be even more effective than in-person counseling. Further, writing is easy, inexpensive, and accessible and thus, could be a good technique to disclose emotions and prevent or treat anxiety-inducing factors in life (37, 39).
The significant effect of other techniques such as counseling (1), training (51), and lifestyle-based education (29) has been reported on reducing anxiety disorders in pregnant women. It is suggested to assess and compare the effect size of various techniques in a systematic review and meta-analysis.
One of the strengths of this study was to observe all the principles of clinical trial design, including random assignment and allocation concealment to prevent selection bias. Efforts were made to ensure equal communication with all the participants and give them full confidence in doing their assignments. The entire staff of the health centers helped the researchers access the mothers’ records. Using the standard questionnaire to measure anxiety was the other strength of this study. However, one of the limitations of this study was the lack of a similar consultation space at all the centers such that the consultation room used for the counseling sessions was a more suitable place for holding the counseling sessions at some centers, but more cramped and compact at some others, which might influence the intervention result. In addition, to prevent the participants’ lack of cooperation, the counseling sessions were arranged according to the health care schedule at each center. Therefore, the interval between the sessions was not fully observed for some of the participants. Due to the nature of the intervention, it was not possible to blind the participants and the data collector. It is recommended to study the effect of writing therapy on stress levels during pregnancy or grieving a pregnancy loss in case of miscarriage or infant death.
5.1. Conclusions
According to the results of this study, writing therapy has a positive effect on reducing maternal anxiety. Writing therapy is a secure and self-directed method in reducing maternal anxiety and ultimately reducing maternal and neonatal complications without the need for clinical and pharmaceutical services.