1. Background
Aggressive behavior of psychiatric inpatients is a prevalent and significant problem for the medical staff and patients (1, 2). Aggressive behavior may be the reason for hospitalization or might be the result of the patient's reaction to admission and could lead to prolonged hospitalization (3). In addition, disrupting the patient's treatment process, aggressive behavior may lead to further aggressive behaviors, adverse effects, physical and psychological harm, and reduced functioning for the patient and other patients admitted to the ward (4).
Research on aggressive behavior of psychiatric inpatients has been focused on analyzing the common factors affecting its prevalence and incidence. Studies have shown that the prevalence of aggressive behavior is age-related and occurs in 3 - 30% of adults, 23 - 50% of adolescents, and 58 - 76% of children (5). In general, the incidence of aggressive behavior in psychiatric patients results from the interaction of various variables, including patient-related variables (such as gender, age, and underlying psychiatric illness), environmental variables (space-related characteristics, such as ward's crowdedness and size), interactive variables (such as stimulation and arousal), and medical staff-associated variables (such as the level of professional knowledge and how they deal with the patient) (6). Despite the abundance of research on the frequency of aggressive behavior, not enough attention has been paid to its severity (3). However, both severity and frequency can influence aggression in the psychiatric ward (7). Thus, it is essential to evaluate the related factors affecting the severity of aggressive behaviors.
Another aspect that still remains unclear in the studies on the aggression of psychiatric patients is the management method concerning aggressive behaviors. The four common methods employed for the immediate management of the aggressive inpatients are the verbal method (no medication and no physical restraint), drug-assisted patient control, physical method (isolation/fixation), and drug-assisted patient control plus physical restraint (3). It should be noted that the selected method for immediate management of aggressive behavior can indeed affect the frequency and the severity of the aggressive behaviors. Without understanding the features of aggressive behavior, the above-mentioned management methods may be inappropriately selected, contributing to more frequent aggressive behaviors (8).
The arguments mentioned above highlight the need for early recognition of patients with potential severe aggressive behavior. The early recognition of these patients would prevent aggressive behaviors and significantly reduce the costs to morale and functioning of the psychiatric wards. In Iran, the majority of studies on the aggressive behavior of psychiatric patients have focused on the experience of mental health providers and the way they perceive aggressiveness (9-11). Therefore, this study intended to emphasize the factors related to psychiatric patients, which can affect the frequency and severity of aggressive behaviors. Furthermore, the restraint methods employed to manage these aggressive behaviors were investigated.
2. Objectives
This study aimed to compare the relationship between demographic information, diagnosis of psychiatric problem, medical illness, and hospitalization characteristics with features of aggressive behavior in patients experiencing different types of restraint during hospitalization.
3. Methods
The present descriptive study was conducted in the psychiatric wards of two hospitals in Tehran, Iran. The minimum sample size (n) was estimated using Cochran’s sample size formula (Equation 1). The prevalence was considered 20% based on a previous study by Baeza et al. (5). Additionally, considering α = 5% and the precision level (d) of 0.07, the minimum sample size was estimated to be 125.
In this study, we included a total of 132 patients (males: 87 vs. females 45) admitted to the psychiatry wards of Taleghani and Imam Hossein hospitals in Tehran, Iran, in 2018. All patients had been restricted during hospitalization. The mean age of the patients was 36.7 years (SD: 12.7), and the age range was 18 - 71 years. The patients were divided into four groups, including verbally-controlled patients (no medication assistance and no physical restraint), patients controlled only by drugs, patients controlled by physical restraint (isolation/fixation), and patients controlled by medication plus physical restraint. Demographic characteristics, including age, gender, educational status, employment status, marital status, admission type, final diagnosis, history of hospitalization, history of drug use, history of aggressive behavior, medical illness, and ward type, were collected based on the patients’ medical information. The patients had been admitted to the women-only, men-only, and emergency wards.
Given the broad definitions of aggressive behavior and different theories about its origin, a standardized method is required to understand and quantify the aggression and its severity. Various unique aggression observation scales have been introduced to standardize the quantification of the aggression severity and provide a single definition for the observed behavior. Among these scales, the Modified Overt Aggression Scale (MOAS) is an aggression observation tool with good inter-rater reliability, which separates aggressive behavior into four subcategories of verbal aggression, aggression against property, auto-aggression, and physical aggression (12). In this study, we used the Persian version of MOAS to assess the severity of aggressive behavior. The questionnaire was completed by nursing staff after the aggressive behavior was observed for each patient within 24 hours. The English version of the questionnaire was first translated into Persian by two independent translators. Afterward, the two translations were compared by an individual fluent in both languages, and a single copy of the Persian translation was prepared. Subsequently, the reverse translation from Persian to English was performed by a bilingual translator who had not seen the original version of the questionnaire. The English translation was then compared to the original version of the questionnaire. To determine the face validity of the questionnaire, the Persian version was primarily provided to the evaluators, and their opinions on understanding words and phrases, appropriateness and relationship of the items, the possibility of ambiguity in terms or the existence of inadequacies in the meanings of the words were received and applied. Finally, the revised Persian version was approved by five faculty members of the Psychiatry Department of Shahid Beheshti University of Medical Sciences.
Moreover, in order to evaluate the reliability of the questionnaire, the inter-rater agreement level was assessed based on the method described by Oliver et al. (13). Thus, for a group of constant patients, the scale was measured independently by two different raters. According to the study by Oliver et al., 60 observations or 30 measurement pairs (for each aggression occurrence, one measurement with the primary rater and one measurement with the second rater) were needed. The data was then used to calculate the kappa score [with 95% confidence interval (CI)] and intraclass correlation coefficient (with 95% CI). All the raters recorded their ratings independently and were blinded to the results by the other raters. The total number of evaluators was six, the number of patients was 18, the duration of the reliability assessment was four months, and the value of the MOAS for the recorded events ranged from 1 to 21. Table 1 represents the results of the reliability evaluation. As can be observed, the levels of agreement between the raters for the total scale and physical aggression (to others) were significantly high, followed by verbal aggression, auto-aggression, and aggression against property. Based on the intraclass correlation coefficient, the agreement between the raters could be considered clinically significant for the questionnaire. Generally, the agreement level (ICC) above 0.75 was acceptable. It should be noted that both methods of the kappa coefficient and intra-cluster correlation index can be used; however, the use of ICC for MOAS has been recommended due to its ordinal nature (13).
| Aggressive Behavior Scale | Kappa (CI = 95%) | ICC (CI = 95%) |
|---|---|---|
| Verbal aggression | 0.77 (0.57 - 0.98) | 0.89 (0.78 - 0.95) |
| Aggression against property | 0.72 (0.50 - 0.94) | 0.82 (0.67 - 0.91) |
| Auto-aggression | 0.83 (0.63 - 1.00) | 0.88 (0.77 - 0.94) |
| Physical aggression | 0.93 (0.78 - 1.00) | 0.98 (0.95 - 0.99) |
| Total Scale | 0.69 (0.52 - 0.86) | 0.93 (0.87 - 0.97) |
After determining the reliability and validity of the MOAS questionnaire, a pilot study was conducted for two months in the psychiatric wards in order to remove any potential concerns. In addition to holding training sessions on the importance of the research design, the staff who were more willing to cooperate in the study were selected as data collectors at the end of each shift.
For the descriptive analysis, statistical parameters were utilized to describe the data depending on the variable. Mann-Whitney and Kruskal-Wallis nonparametric tests (P-value = 0.05) were applied to determine the relationship between the variables depending on their type. We also used the Spearman correlation coefficient (α = 0.01) to determine the relationship between MOAS and the number of days spent in the hospital. IBM SPSS 24 was used for statistical analysis.
4. Results
Out of a total of 1,642 patients admitted to adult psychiatry departments, 132 cases had been recorded to have aggressive behaviors. The total number of incidence of aggressive behaviors registered by nurses (raters) was 192 events. Based on these results, the prevalence of aggressive behaviors was found to be 11.7%. The results also revealed that some patients had several recorded events (aggressive behavior). Table 2 depicts the demographic and clinical characteristics of the recorded aggressive behaviors.
| Variables | No. (%) |
|---|---|
| Gender | |
| Male | 118 (61.5) |
| Female | 74 (38.5) |
| Marital status | |
| Single | 76 (39.6) |
| Married | 82 (42.7) |
| Divorced or widowed | 34 (17.7) |
| Education level | |
| Uneducated | 29 (15.1) |
| Precollege education | 139 (72.4) |
| College degree | 24 (12.5) |
| Employment status | |
| Unemployed | 150 (78.2) |
| Employed | 31 (16.1) |
| Retired | 11 (5.7) |
| Admission type | |
| Involuntary | 136 (70.8) |
| Voluntary | 56 (29.2) |
| History of hospitalization | |
| None | 54 (28.1) |
| Once | 38 (19.8) |
| More than once | 100 (52.1) |
| Non-mental medical condition | |
| Yes | 52 (27.1) |
| No | 140 (72.9) |
| Diagnosis | |
| Psychotic disorders | 57 (29.7) |
| Mood disorders | 92 (47.9) |
| Comorbidity | 18 (9.4) |
| Other | 25 (13) |
| History of substance abuse | |
| Yes | 63 (32.8) |
| No | 129 (67.2) |
According to the results in Table 2, this behavior was more frequently observed in males. Furthermore, being married, having a pre-university degree, and unemployment accounted for a higher proportion of the patients showing aggressive behavior. The majority of the cases showing aggressive behavior were admitted involuntarily and also had more than one experience of hospitalization. Additionally, the proportion of the patients with mood disorders was higher compared to that in other groups. Substance abuse was present in only 32.8% of cases.
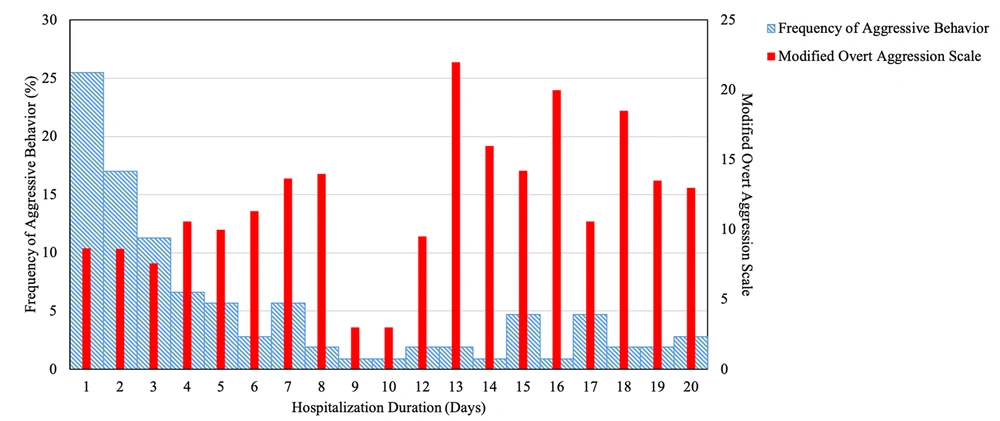
After confirming the validity and reliability of the MOAS (ICC = 0.93), it was used to evaluate the severity of the aggressive behaviors. The range of scale ranged from 1 to 30, with a median of 9 (mean = 10.3, SD = 6.7). Based on the Shapiro-Wilk test, the distribution of the scale was not normal (P-value = 0.00). The severity of aggressive behavior was not significantly correlated with age, yet it had a weak positive correlation with hospitalization duration (Spearman’s ρ = 0.262, P-value = 0.00). Hospitalization duration ranged from 1 to 20 days with a median of 3 (mean = 5.9, SD = 5.9). Figure 1 demonstrates the relationship between the frequency of aggressive behavior with the hospitalization duration. As can be seen, as the duration of hospitalization increases, the frequency of aggressive behavior decreases, whereas its severity intensifies. The relationship between the aggression severity with gender, admission type, non-mental medical condition, and history of substance abuse was assessed using the Mann-Whitney U test (Table 3). The severity of aggressive behavior was significantly associated with gender (P-value = 0.003), admission type (P-value = 0.00), non-mental medical condition (P-value = 0.026), and history of substance abuse (P-value = 0.025). Table 3 shows the results of the relationship between the severity of aggressive behavior and the history of aggressive behavior. The results indicated that the severity of aggressive behavior had a significant relationship with a history of aggressive behavior prior to hospitalization (P-value = 0.001), yet it had no significant relationships with a history of aggressive behavior during hospitalization (P-value = 0.06). The relationship between MOAS with marital status, education level, employment status, number of previous hospitalizations, and diagnosis of psychiatric illness was evaluated by Kruskal-Wallis statistical test. Among these variables, education was the only variable that had a significant relationship (χ2 = 5.82, DoF = 2, P-value = 0.05) with the severity of aggressive behavior.
| Variables | Median of MOAS (Range) | Mann-Whitney U Test | Z | Significance |
|---|---|---|---|---|
| Gender | 880.5 | -2.939 | 0.003 | |
| Male | 11 (1 - 30) | |||
| Female | 7 (1 - 20) | |||
| Admission type | 635 | -3.673 | 0.000 | |
| Involuntary | 11 (1 - 30) | |||
| Voluntary | 6 (1 - 6) | |||
| Non-mental medical illness | 803 | -2.227 | 0.026 | |
| Yes | 7 (1 - 25) | |||
| No | 10 (1 - 30) | |||
| History of substance abuse | 988.5 | -2.237 | 0.025 | |
| Yes | 12 (1 - 30) | |||
| No | 8 (1 - 29) | |||
| History of aggressive behavior before hospitalization | 729 | -3.454 | 0.001 | |
| Yes | 11 (1 - 30) | |||
| No | 7 (1 - 25) | |||
| History of aggressive behavior during hospitalization | 929 | -1.884 | 0.06 | |
| Yes | 11 (1 - 30) | |||
| No | 8 (1 - 25) |
a Mann-Whitney U test, P-value = 0.05.
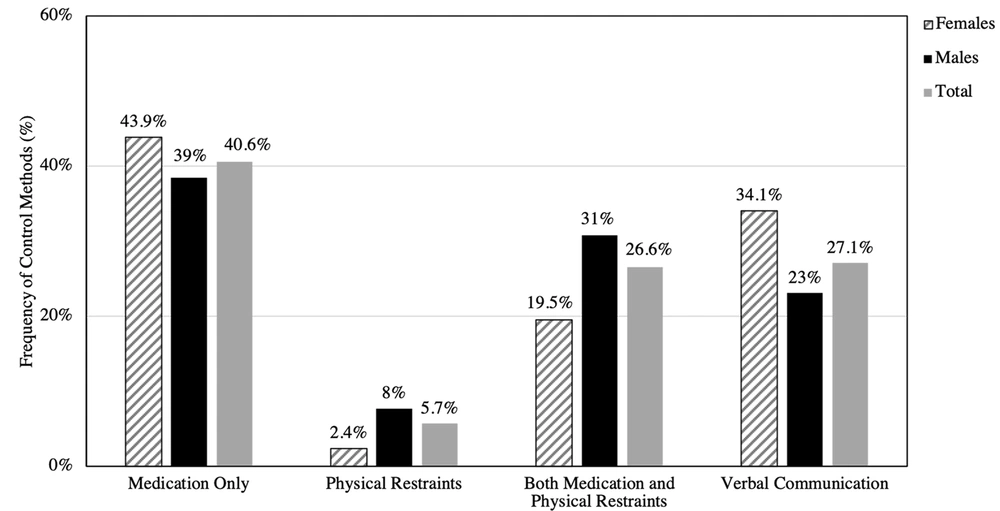
Figure 2 illustrates the results of aggression management methods. The majority of aggressive behaviors were controlled by drugs, and physical methods were less likely to be used. Also, the frequency of female patients controlled by less aggressive methods (verbal method and drug-assisted control) was higher. This trend was reversed for male patients since a higher proportion of male patients was controlled by physical methods.
5. Discussion
This study aimed to evaluate the frequency of aggressive behavior in the patients admitted to adult psychiatry wards of Imam Hossein and Taleghani hospitals in Tehran, Iran, and to assess the relationship between the severity of aggressive behaviors and demographic variables.
According to our results, the prevalence of aggressive behaviors in patients (11.7%) was consistent with that in previous studies (3 - 30%) (5). As expected, the effects of most demographic factors were consistent with those reported in previous studies. Generally, in most studies, the male gender had a significant and direct relationship with the frequency of aggressive behavior (14), which was similar to our results. In terms of marital status, the majority of aggressive behaviors were observed among single, widowed, or divorced patients. This trend was also observed in some previous studies (14). The prevalence of aggressive behavior in uneducated patients and those with a college degree was approximately similar, which was consistent with the results of some other researchers (15, 16). Even though there has been limited research on the relationship between job status and aggressive behavior, a study by Newton et al. implied that unemployment is significantly associated with the frequency of aggressive behavior in psychiatric wards (17). Similarly, the majority of the recorded incidents belonged to the patients who were either unemployed or retired.
However, in this study, certain clinical factors showed contrasting results with some previous studies. In the present study, aggressive behavior was observed more frequently in patients with mood disorders. Some studies have suggested the highest prevalence of aggressive behaviors among patients with schizophrenia (14). Nonetheless, Volavka reported that the prevalence of violent behavior in bipolar disorder is at least as high as that in schizophrenia (18). The reason for this contradiction is that research efforts in bipolar disorder lagged behind analogous work in schizophrenia (19). Another reason for different results in this study was substance abuse. The presence of substance abuse was correlated with the frequency of aggressive behaviors in previous studies; however, those results have shown a great degree of heterogeneity. Some studies have reported that including alcohol use might affect the results (14). Another reason for this difference might be that this information was based on self-reporting of the patients regarding their substance abuse, and respondents may misreport or deny their usage (20). Consistent with previous studies (14), both involuntary admission and previous hospitalization admissions were correlated with an increased number of aggressive behaviors.
In this study, we also investigated the relationship between demographic and clinical variables with the severity of aggressive behavior. Among the demographic variables, gender, education level, and history of aggressive behavior before admission were significantly correlated with MOAS. It is noteworthy that higher severity in aggressive behavior was observed in male patients and those with a lower education level. Among the clinical variables, the severity of aggressive behavior had a weak positive correlation with a more extended hospitalization period. Moreover, admission type, concomitant medical illness, and substance abuse were significantly correlated with the MOAS. The patients with involuntary hospitalization and the absence of non-mental medical conditions were more aggressive, and a history of substance abuse was associated with an increase in the severity of aggressive behavior. Although the number of studies on aggression severity is considerably lower compared to that on aggression frequency, some of the observed results are comparable to the literature, such as a significant relationship between aggression behavior intensity and substance abuse (21). In terms of aggression management, the majority of incidents were controlled by drugs, and physical methods were rarely applied. However, there was a contrast in the management method for female and male patients. Less aggressive methods were used to control female patients.
In general, the results of this study suggested that the male gender, being single and unemployed, and having mood disorder diagnosis were correlated with a higher frequency of aggressive behavior. However, the severity of these behaviors correlates with gender, education level, duration of the hospitalization, admission type, concomitant medical illness, and history of substance abuse. This information could be used for early identification of patients with the potential of aggressive behavior. This practice would assist the caregivers in considering an effective management strategy to control these patients, and an appropriate approach might be used to prevent potential adverse consequences. Understanding a proper management strategy requires further research in this regard.
The most important limitation of this study was that some of the aggressive behaviors could be missed by the nursing staff, which may lead to underestimation of the incidence of aggressive behavior. Moreover, demographic characteristics were based on the information recorded in the patients’ medical history file. Hence, the accuracy of this information depends on the accuracy of the registrants. It is suggested that the patients’ view on aggressive behavior be considered in future studies. Time constraints and the elimination of adolescent patients from the samples were also among the limitations of the current study.