1. Background
Patients with schizophrenia spectrum disorders, including schizophrenia, schizoaffective, and delusional disorder may experience some impairments in social functioning, interpersonal relationships, emotion recognition, and problem-solving. Social skills are appropriate social behavior, used in proper time and setting to foster success in everyday life (1). Social skills training (SST) is described as behavioral interventions in which the patient’s social functioning is targeted (2). The effectiveness of SST has been demonstrated in patients with schizophrenia (3-7). Furthermore, the vulnerability-stress model suggests that coping skills, including social skills, can reduce the impact of stress on the severity of psychotic symptoms (4). Introducing SST interventions was based on studies that suggested the patient’s ability to learn through observation and practice (8). Early practices of SST in schizophrenia were based on behavioral changes in hospitalized patients. Later on, interventions were designed to be implemented in individual or group outpatient settings (4).
A recent meta-analysis suggested that SST is an effective intervention in reducing negative symptoms (6, 9, 10). Some studies have suggested that SST in patients with schizophrenia is essential to improve quality of life and social abilities and has been considered as a part of comprehensive treatment. Quality of life is an important outcome of the treatment. A relationship between symptoms of schizophrenia and quality of life has been reported (7). A meta-analysis in 2002 suggested that SST for patients with schizophrenia does not contribute to the improvement of compliance, quality of life, and social function (11). Some other studies have indicated that SST can improve the social capabilities of patients with schizophrenia (3, 12).
In Iran, as a developing country, there are some barriers to provide psychosocial services to the patients. Limited resources, low socioeconomic status, and insurance coverage may affect the structure and quality of services. Most of the existing programs are long-term, and based on limited financial resources in Iran, providing short-term services is more feasible and cost-effective. Recently, a study was performed on patients referring to Razi Psychiatric Hospital using different manuals (13).
2. Objectives
The aim of this study was to evaluate the effects of short-term SST on positive and negative symptoms, quality of life, and global functioning in patients with schizophrenia spectrum disorders in an outpatient clinic in Iran.
3. Methods
This clinical trial with a before-after design was conducted on 29 patients diagnosed with schizophrenia spectrum disorders based on the new version of the diagnostic and statistical manual of mental disorders (DSM-5). They aged 18 - 65 years, with at least elementary education, residing in Tehran or in the surrounding suburbs who were referred to the Day rehabilitation center at Roozbeh Hospital from April 2016 to April 2017 selected by convenience sampling. The patients were not in the acute phase of their illness and were receiving antipsychotic medications.
Patients with a history of head trauma, neurological or disabling medical conditions, substance abuse, and intellectual disability were excluded. Furthermore, patients and their families signed informed consent forms. After obtaining the patient’s medical and case history, demographic data were collected and assessed using global assessment of functioning (GAF), positive and negative syndrome scale (PANSS), world health organization quality of life assessment (WHOQOL-BREF) instrument was performed by a trained psychologist. Then, the patients participated in short-term SST sessions. We used the Persian version of PANSS to assess the positive, negative, and general symptoms of illness (14); and the Persian version of WHOQoL-BREF was applied to assess the patients‘ quality of life in four domains, including psychological, physical, social, and environmental domains (15). We used a revised manual of SST, which was developed by the Department of Occupational Therapy of the University of Rehabilitation and Welfare Sciences. This manual is based on a guideline developed by Bellack, with the same structure and different content (16).
The training was provided in twelve 60 - 90 min group sessions. by two moderators, a trained occupational therapist, and a third-year resident of psychiatry. The main therapeutic techniques used in each session were modeling, role-playing, and feedback. At the end of twelve sessions and three months later, reassessment with GAF, PANSS, HDRS, WHOQOL-BREF, and Client Satisfaction Questionnaire (CSQ) was performed by the same psychologist.
The sample size was calculated based on a study presented at the Social Psychiatry Conference in Tehran (13). According to this study, the mean of GAF in patients in the intervention group was 51 at baseline and 63 in the follow-up. Based on the comparison of the two means before and after, the alpha of 0.05, test power of 80, and the mean values of 51 and 63 at baseline and follow-up, respectively, and considering the standard deviation of 9, the sample size was considered at least 9 cases. Considering the attrition of 50% (in the outpatient setting) (17), it was necessary to examine at least 18 patients.
The study was accepted by the Ethics Committee of Tehran University of Medical Sciences (Ethics Code: IR.TUMS.VCR.REC.1395-395), and it was also registered at the Iranian Registry of Clinical Trials (IRCT2016043027691N1). Table 1 presents the skills areas considered in this study.
| Sessions | Skills Areas |
|---|---|
| Session 1 | Listening |
| Session 2 | Making a request |
| Session 3 | Expression of pleasant emotions |
| Session 4 | Expression of unpleasant emotions |
| Session 5 | Criticizing |
| Session 6 | Initiating a conversation |
| Session 7 | Maintaining a conversation |
| Session 8 | Ending a conversation |
| Session 9 | Making a conversation with the unfamiliar person |
| Session 10 | Principles in conversation |
| Session 11 | Finding common topics |
| Session 12 | Problem-solving |
Repeated measure analysis of variance (ANOVA) and Mauchly's Test of Sphericity were used for data analysis at the significance level of 0.05.
4. Results
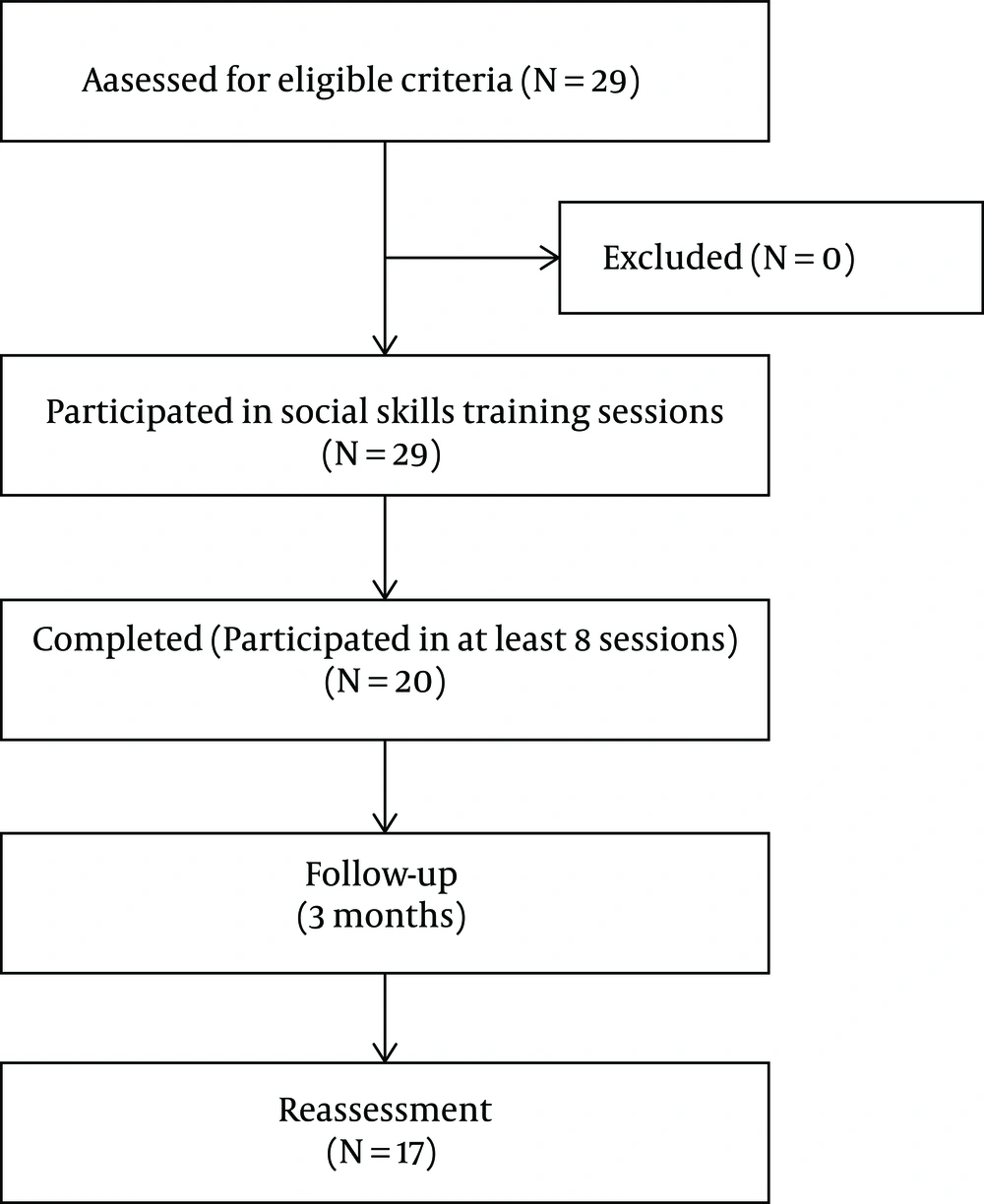
Flowchart of the study participant selection is shown in Figure 1 and demographic characteristics of the patients are presented in Table 2.
| Variable | No. (%) of Patients |
|---|---|
| Age | |
| 20 - 30 | 8 (27.6) |
| 31 - 40 | 15 (51.7) |
| 41 - 50 | 4 (13.8) |
| 51 - 60 | 2 (6.9) |
| Gender | |
| Male | 23 (79.3) |
| Female | 6 (20.7) |
| Educational Status | |
| Elementary | 3 (10.3) |
| Middle high school | 15 (51.7) |
| High school diploma | 8 (27.6) |
| University degree | 3 (10.3) |
| Job status | |
| Unemployed | 19 (65.5) |
| Employee | 6 (20.7) |
| Homemaker | 4 (13.8) |
| Marital Status | |
| Single | 23 (79.3) |
| Married | 2 (6.9) |
| Divorced | 4 (13.8) |
4.1. Social Skills Training and Positive and Negative symptoms
The mean score of positive and negative symptoms improved at the end of the intervention and three months later (F = 8.17, P = 0.004 and F = 5.96, P = 0.012, respectively). A pairwise comparison of the baseline and at the end of the three-month follow-up suggested statistical significance for positive and negative domains (P = 0.003 and P = 0.008, respectively) (Table 3).
| Variable | First Assessment, Mean | Second Assessment, Mean | Third Assessment, Mean | F | Multivariate Tests, P-value | Partial eta squared |
|---|---|---|---|---|---|---|
| PANSS (positive symptoms) | 13.529 | 11.824 | 10.941 | 8.177 | 0.004 | 0.522 |
| PANSS (negative symptoms) | 18.765 | 17.294 | 16.118 | 5.965 | 0.012 | 0.443 |
| GAF | 1.8824 | 2.2941 | 2.2941 | 3.878 | 0.045 | 0.339 |
Abbreviations: PANSS, positive and negative symptom scale; GAF, global assessment of functioning.
aThe significance was set at P < 0.05
4.2. Social Skills Training and Quality of Life
The mean score of the psychological domain of quality of life improved at the end of the intervention and three months later. Repeated measures ANOVA showed a statistically significant difference within the group (baseline, after the termination of 12 sessions and after three months follow-up) (P = 0.042, F = 3.954). There was no statistically significant difference between the baseline and the third assessment (P = 0.053).
4.3. Social Skills Training and Global Assessment of Functioning
The mean score of GAF improved in all three assessments. A pairwise comparison between the baseline and the end of the intervention, and also between the baseline and after three months of follow-up, suggested a statistically significant difference (P = 0.014, P = 0.014, F = 3.84). The role of different variables in the improvement of GAF was assessed using tests of between-subjects effects (Table 4).
| Variables | df | Mean Square | F | P-value |
|---|---|---|---|---|
| Age | 33 | 0.737 | 2.479 | 0.107 |
| Gender | 1 | 0.002 | 0.004 | 0.952 |
| Educational Status | 3 | 0.193 | 0.456 | 0.718 |
| Job Status | 2 | 0.373 | 0.978 | 0.400 |
| Marital Status | 2 | 0.167 | 0.408 | 0.673 |
| Illness Duration | 12 | 0.432 | 1.946 | 0.273 |
| Hospitalization | 6 | 0.310 | 0.824 | 0.579 |
aThe significance was set at P < 0.05.
The equivalent doses of antipsychotics did not show a statistically significant difference in all three assessments.
4.4. Dropout
As mentioned before, patients who were participated in at least eight out of twelve SST sessions were considered completers. According to this consensus, 20 patients (69%) completed the course. Only 17 patients (58.6%) accepted the invitation to participate in the reassessment session at the end of three months. The reason for non-acceptance was not explored.
5. Discussion
Schizophrenia spectrum disorders can influence different social aspects of life. Despite pharmacotherapy, poor performance was observed in most patients. Although antipsychotics are highly effective in the treatment of positive symptoms, the role of these medications in the improvement of negative symptoms and cognitive deficits is not prominent. The combination of pharmacotherapy and psychosocial interventions are considered as the standard care for patients with schizophrenia spectrum disorders. Furthermore, people with severe psychiatric illnesses, such as schizophrenia spectrum disorders need to use social support and skills training after discharge (12). Most of the experts believe that SST should be considered as a part of a comprehensive treatment plan in rehabilitation services (4, 5, 7, 18). Recently in Iran, psychosocial interventions have been developed and provided for patients with severe mental illnesses (19). Unfortunately, these services are not available for all patients.
As mentioned before, in this study, the mean score of positive and negative symptoms improved at the end of the intervention and also after three months of follow-up. There was a statistically significant difference between the baseline and the third assessments. This finding suggests that SST can cause improvement in positive and negative symptoms (3, 9, 10).
Evidence regarding the role of SST in positive symptoms improvement is controversial. This may be as a result of methodological differences, such as different duration of follow-up. The role of SST in the improvement of negative symptoms has been reported (6, 9, 18), while other studies have shown that SST in these patients did not reduce the positive symptoms compared with the control group in both hospital and outpatient groups. In a randomized clinical trial in Iran, SST in hospitalized patients could reduce negative symptoms after the intervention sessions. In this study, there was no follow-up assessment (13). In the current study, we observed improvement in both positive and negative symptoms after the sessions and three months of follow-up.
Our study suggests that SST can reduce positive and negative symptoms. Improvement in positive symptoms is a new finding in our study. In hypothesis, patients may engage in more meaningful social activities. This could distract them from positive symptoms. Although positive symptoms exist in patients, the patient reports them less often.
Our results suggest that the mean score of the psychological domain of quality of life improved in all three assessments. Based on repeated measures ANOVA results, there was no statistically significant difference within the group. Although there was no statistically significant difference between the baseline and the third assessments, the result is only a little short of significance.
Various instruments have been used in different studies to investigate the role of SST in quality of life. In this study, the WHOQOL-BREF was used to assess the quality of life. Improvement in the psychological domain of quality of life may reflect the role of interpersonal relationships in the patient's life. We did not observe any improvement in other domains. Perhaps, the duration of our intervention was not enough to promote the patients‘ quality of life. Studies have shown that there is a relationship between the negative symptoms and the performance of patients with schizophrenia and their quality of life (20).
The mean score of GAF improved in all three assessments. A pairwise comparison between baseline and the second assessments and between baseline and the third assessments suggested a statistically significant difference. On the other hand, after the 12 training sessions, the patients’ functioning improved. This improvement was still apparent after the three months of follow-up and was not influenced by the patient’s demographic characteristics. In different studies, other instruments have been used to investigate the level of patient functioning. A meta-analysis suggests that SST moderately affect indicators of life skills based on overall performance and social performance. Some authors showed that the mean of patients’ social functioning score after three months was significantly higher than the pre-test score (21). However, in most studies, there was no follow-up assessment.
As mentioned before, patients who participated in at least eight out of twelve SST sessions were considered as completers. The dropout percentage was 31%. There was no statically significant difference between these groups in demographic variables. The reason for non-acceptance was not investigated. Lack of assessment of the baseline cognitive capacities, poor insight into illness, and the long commute to the hospital may be the causes of the patient’s disinterest.
As a pilot study, these results were encouraging. SST should be used as an intervention in comprehensive rehabilitation programs. It should be noted that social skills are culture-dependent, and some skills are not properly suitable for Iranian patients (22). Thus, the training package should be revised, completed, and re-evaluated after overcoming the barriers.
5.1. Limitations
This study was a clinical trial with a before-after design without a control group, which is a methodological limitation. Furthermore, the sample size was small, and this was an important limitation in our study. Although there was no statistically significant difference in some variables, they demonstrated an improvement in three assessments.
This study did not investigate the reasons for patients dropping out of the final assessment. However, it is plausible because Tehran is a large metropolitan city with congested traffic, and transportation is the main challenge, which can influence the continuity of care.
The short period of the follow-up was another limitation. Generalization of the acquired skills is another field of concern, which is mentioned in some studies (4). In this study, we did not assess the generalization of the acquired skills. Furthermore, we did not assess the basic level of social skills before the intervention.
5.2. Conclusion
SST may reduce positive and negative symptoms and promote performance among patients with schizophrenia spectrum disorders in a rehabilitation center in Iran. These results were achieved after a three-month follow-up. This effective intervention should be considered in aftercare services.
5.3. Future Direction
Studies with a larger sample size, using the randomized clinical trials, evaluating the generalization of the acquired skills, assessing the cognitive capacities before engagement in skills training, and using a native educational package are recommended.