1. Context
Pregnancy is an important period in women’s lives, which is often associated with emotional and mood changes (1, 2). Depression is the most common mental disorder that reduces the ability of people and hinders the growth and development of the individuals. According to the world health organization (WHO), depression is the most important cause of disability in women worldwide (3). This disorder in individuals is characterized by feelings and symptoms such as impaired memory, weight loss, anorexia, feeling bad about themselves, feeling of guilt, hopelessness, thoughts of self-harm, discomfort, low self-esteem, depressed mood, and sadness (4).
Depression during pregnancy is a common problem in pregnant women. Its causes are associated with genetics, history of a mental disorder, physiological and social changes, hormonal changes, physical problems such as nausea and recurrent vomiting, fatigue, sudden pains during pregnancy, and concerns about the health of the fetus and even delivery (5, 6). Untreated depression may have short-term and long-term effects on the mother, including high-risk behaviors, preeclampsia, increased risk of postpartum depression, and pregnancy outcomes such as low birth weight, premature birth, small head circumference, increased distress after delivery, and disrupted sleep (7-9). In addition, depression in pregnancy is related to a range of adverse pregnancy outcomes such as social isolation (10), marital discord (11), child’s delay in motor and intellectual development (12), fetal growth restriction, and high-stress response in infants (13, 14).
2. Evidence Acquisition
Studies report various prevalence rates for depression in pregnant women in Iran (15% to 88.7%) and there is no exact estimate of it (15-48). Systematic reviews and meta-analyses can provide a complete view of a problem in the community by examining all relevant documentation and provide a clear picture (49-51). Given the importance of depression during pregnancy, this study aimed to investigate the prevalence of depression among pregnant women in Iran using the meta-analysis method.
2.1. Data Sources
The present study is a systematic review and meta-analysis of all the current research literature on the prevalence of depression in pregnant women in Iran. This study was conducted based on the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines (51). To avoid bias, search, selection of studies, quality assessment, and data extraction were conducted by two researchers independently in each step. In case of disagreement, the results were evaluated by a third researcher.
2.2. Search Strategy
The national and international databases, including Magiran, Barakat knowledge network system, SID (Scientific Information Database), Regional Information Center for Science and Technology (RICST), Iranian National Library, IranDoc, PubMed, Elsevier (Science Direct, Embase, and Scopus), Web of Science (ISI), and Google Scholar search engine were searched without time limit until 2017. Resources were found by two researchers independently, who were experts in searching databases.
The search mechanism was mainly based on systematic searches using Persian and English (MeSH) keywords, including “prevalence”, “depression”, “mental disorders”, “mental health”, “pregnancy”, “pregnant woman”, “prenatal care”, “pregnancy complications”, “epidemiology”, " prevalence " and “Iran” as well as their combination using “AND” and “OR” operators. In order to find more studies, references of all relevant articles were reviewed. The combined search in the PubMed database is shown in supplementary file Appendix 1.
2.3. Inclusion and Exclusion Criteria
The main inclusion criteria in this study included studies on the topic of depression prevalence in Iran. The exclusion criteria included: (1) non-randomized sample size; (2) non-pregnant subjects; (3) irrelevance; (4) insufficient data for non-reported prevalence of depression; (5) sample size with a history of mental illness or depression medication users; and (6) Reviews, case reports, and editorial letters.
2.4. Qualitative Evaluation
Papers selected by the researchers were reviewed using the modified Newcastle Ottawa Scale (NOS) for cross-sectional studies (52). The checklist contains 8 sections in 4 categories. The method for scoring; 0 - 1 points were awarded to each item; therefore, the maximum attainable point was 8. The studies were separated into three categories: 1- Low quality: < 5, 2- Moderate quality: 5 to 6 scores and 3- High quality: 7 to 8 scores. Finally, studies with a minimum of [5] score were selected for the meta-analysis.
2.5. Data Extraction
The researchers used a checklist containing the required information such as researcher(s) name, title, year of study, place of study, study design, sample size, age (mean ± standard division), gestational age, used questionnaire, the prevalence of depression, the intensity of depression (mild, moderate, and severe), and the pregnancy trimester.
2.6. Statistical Analysis
The binomial distribution was used to calculate the variance of each study. To assess the heterogeneity of the studies, Cochran’s Q test and I2 statistic were used. Due to the heterogeneity of the studies, a random effects model was used to combine studies (53, 54). Sensitivity analysis was conducted to show the effect of omitting one study on the overall estimate at a time (55). To find the source of heterogeneity, the subgroup analysis was performed based on the geographic region, questionnaires and pregnancy trimester. In addition, the meta-regression model was used based on the year of study. Publication bias was assessed by Egger and Begg’s test. Data were analyzed using comparative meta-analysis (CMA) software ver. 2. A P value lower than 0.05 was considered significant.
3. Results
3.1. Literature Search Results
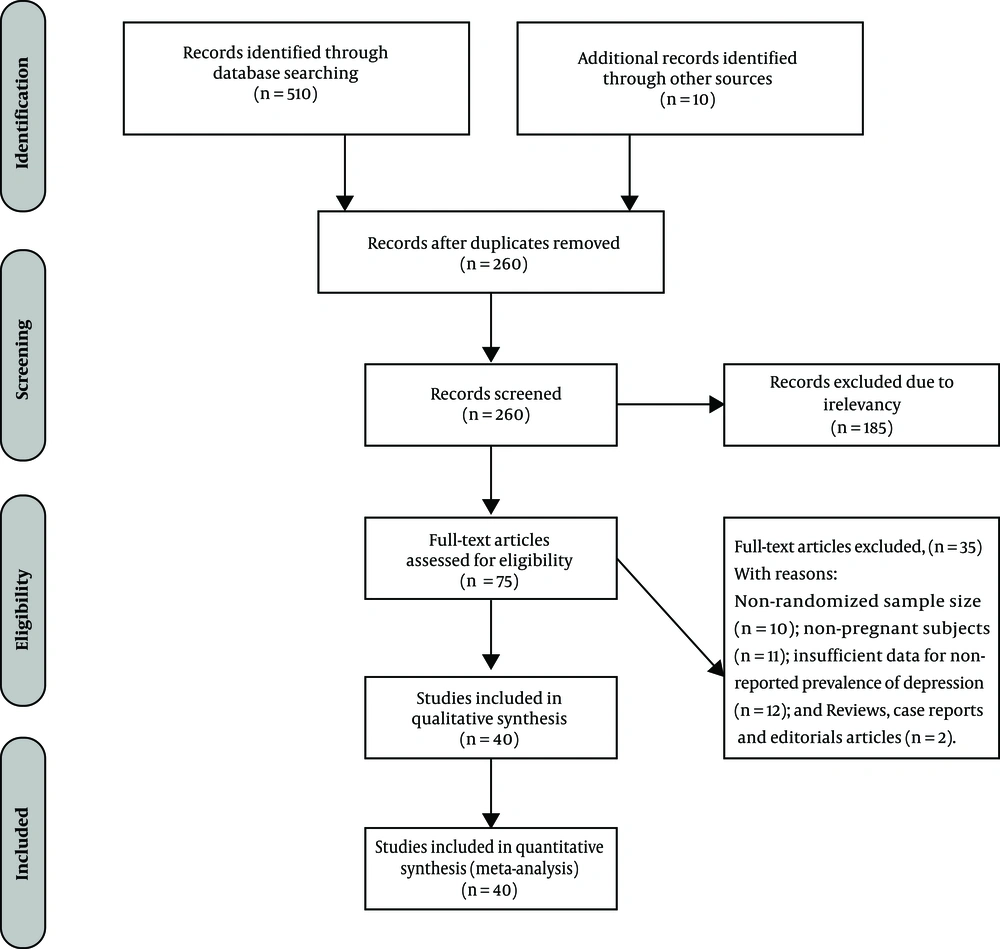
In the systematic review, 520 studies were identified after the review. 260 studies were excluded because of being duplicates; the abstract of 260 probably related studies was examined and the full text of 75 papers was included in the final list. After applying the inclusion and exclusion criteria and qualitative evaluation, 40 qualified studies, published from 1990 to 2017, finally entered the meta-analysis. (Figure 1)
3.2. Characteristics of Studies Included in the Systematic Review
Forty studies containing 15,870 pregnant women were included in the meta-analysis. The mean age of participants in 13 studies (available data) was 25.90 ± 0.36 years. Study details included in the meta-analysis are shown in Table 1.
| Ref | First Author | Place | Year of Study | Sample Size | Age (Mean ± SD) | Trimester of Pregnancy | Questionnaire | Prevalence of Depression (%) |
|---|---|---|---|---|---|---|---|---|
| (15) | Bazarganipour F. | Aran va Bidgol | 2008 | 200 | 25.89 ± 5.5 | First | Beck | 41 |
| (16) | Garrusi B. | Kerman | 2012 | 255 | 29.1 ± 6.4 | All | Beck | 30 |
| (17) | Bondad R. | Mashhad | 2001 | 320 | 24.5 ± 0.9 | Third | Beck | 57.8 |
| (18) | laloee A. | Tehran | 2005 | 400 | 26.4 ± 4.9 | All | Beck | 21.3 |
| (19) | Najafi F. | Tehran | 2015 | 2721 | 28.4 ± 6.12 | Third | DSSA21a | 50.7 |
| (20) | Ghasemi A. | Tehran | 2002 | 1452 | 25.3 ± 6 | All | SCL-90Rb | 10.5 |
| (21) | Modabernia M. | Rasht | 2007 | 415 | Third | Beck | 25 | |
| (22) | Parsaie Rad E. | Ahvaz | 2009 | 70 | Third | Beck | 33.3 | |
| (23) | Nazari H. | Khorramabad | 2011 | 280 | 26.7 ± 6.0 | All | GHQc | 11.8 |
| (24) | Moshki M. | Gonabab | 2014 | 208 | 26.89 ± 4.5 | Third | Edinburghd | 30 |
| (25) | Shahmiri H. | Zanjan | 2004 | 300 | 26.2 ± 4.31 | All | Zung | 32 |
| (26) | Amanat S. | Isfahan | 2005 | 600 | All | Beck | 28.7 | |
| (27) | Ranjbar M | Bonab | 2015 | 125 | 24.4 ± 4.5 | All | EPDS | 56 |
| (28) | Mardanihamule M. | Shahin Shahr | 2009 | 315 | Third | GHQ | 16 | |
| (29) | Moeinimehr M. | Isfahan | 2010 | 966 | All | PHQe | 70.1 | |
| (30) | Karbakhsh M. | Tehran | 2001 | 170 | All | Beck | 30.6 | |
| (31) | Pazande F. | Tehran | 1999 | 260 | Third | Beck | 40 | |
| (31) | Pazande F. | Tehran | 1999 | 143 | Second | Beck | 45.5 | |
| (31) | Pazande F. | Tehran | 1999 | 173 | First | Beck | 54.3 | |
| (32) | Omidvar S. | Babol | 2006 | 191 | All | Beck | 28.8 | |
| (33) | Shabangiz A. | Isfahan | 2013 | 378 | Third | Beck | 65.2 | |
| (34) | Baghi V. | Saqez | 2012 | 140 | 27.4 ± 5.3 | Second and Third | EPDS | 32.9 |
| (35) | Salmalian H. | Babol | 2006 | 263 | 25.6 ± 4.8 | First and Second | Beck | 59.3 |
| (36) | Hosaynisazi F. | Tehran | 2003 | 180 | 26.14 ± 7.4 | Third | Beck | 49.4 |
| (37) | Iranfar S. | Kermanshah | 2003 | 163 | Third | Beck | 53.4 | |
| (38) | Ehsanpour S. | Isfahan | 2011 | 404 | Third | Beck | 26.7 | |
| (39) | Rezaee R. | Babol | 2012 | 47 | Second | DSSA21 | 31.9 | |
| (39) | Rezaee R. | Babol | 2012 | 47 | First | DSSA21 | 42.5 | |
| (39) | Rezaee R. | Babol | 2012 | 48 | Third | DSSA21 | 72.9 | |
| (40) | Kheirabadi G. R. | Isfahan | 2007 | 1898 | Third | Beck | 88.7 | |
| (41) | Mosalanezhad L. | Jahrom | 2006 | 214 | Third | Scl-90R | 42 | |
| (42) | Sotoudeh G. | Tehran | 2000 | 55 | All | Beck | 20.2 | |
| (43) | Hadavi M. | Rafsanjan | 2003 | 350 | Third | Beck | 43.4 | |
| (44) | Balouchi A. | Zabol | 2015 | 110 | All | GHQ | 45 | |
| (45) | Shahhosseini Z. | Sari | 2009 | 428 | Second | EPDS | 26.2 | |
| (46) | Hejrati P. | Hamedan | 2010 | 197 | Second | EPDS | 49.7 | |
| (47) | Jamali S. | Jahrom | 2016 | 264 | First | Beck | 61.7 | |
| (47) | Jamali S. | Jahrom | 2016 | 342 | Second | Beck | 71.6 | |
| (47) | Jamali S. | Jahrom | 2016 | 491 | Third | Beck | 75.5 | |
| (48) | Delavari M. | Tabriz | 2016 | 287 | Third | EPDS | 15.7 |
a Depression anxiety stress scales- 21
b Symptom checklist-90-revised
c General health questionnaire
d Edinburgh postnatal depression scale
e Patient health questionnaire
3.3. Total Prevalence of Depression
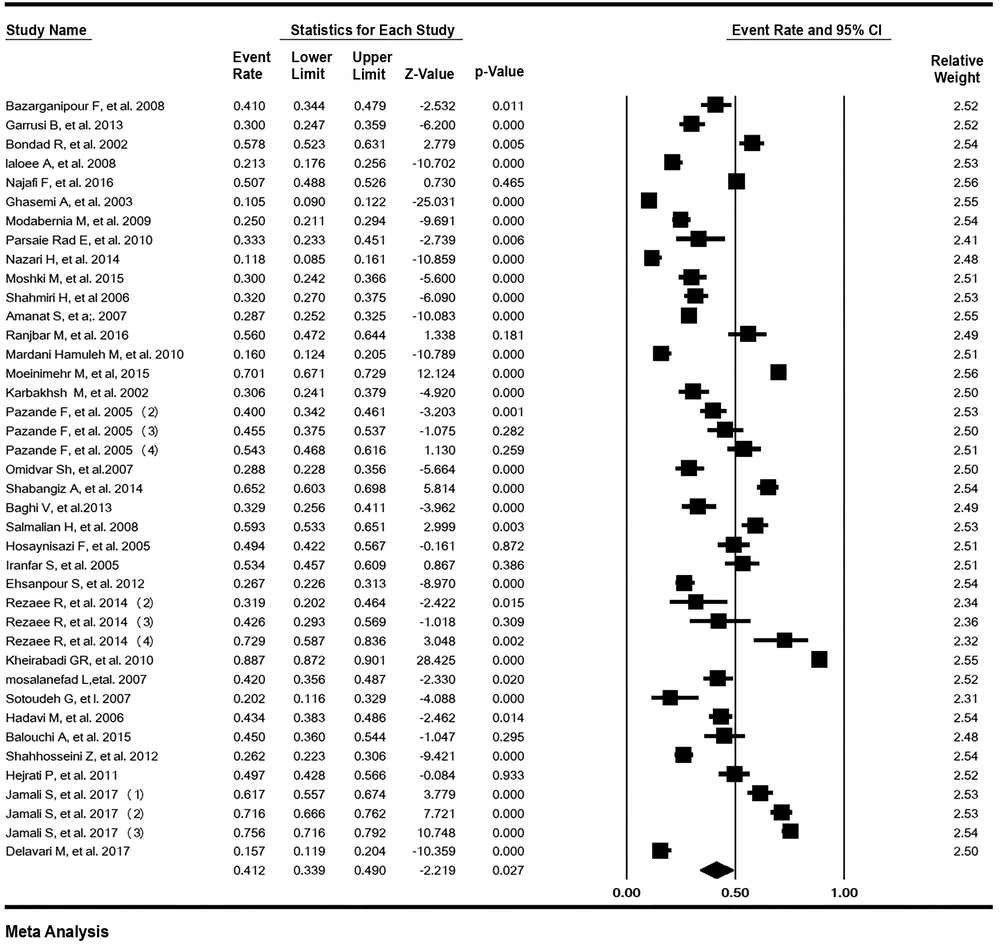
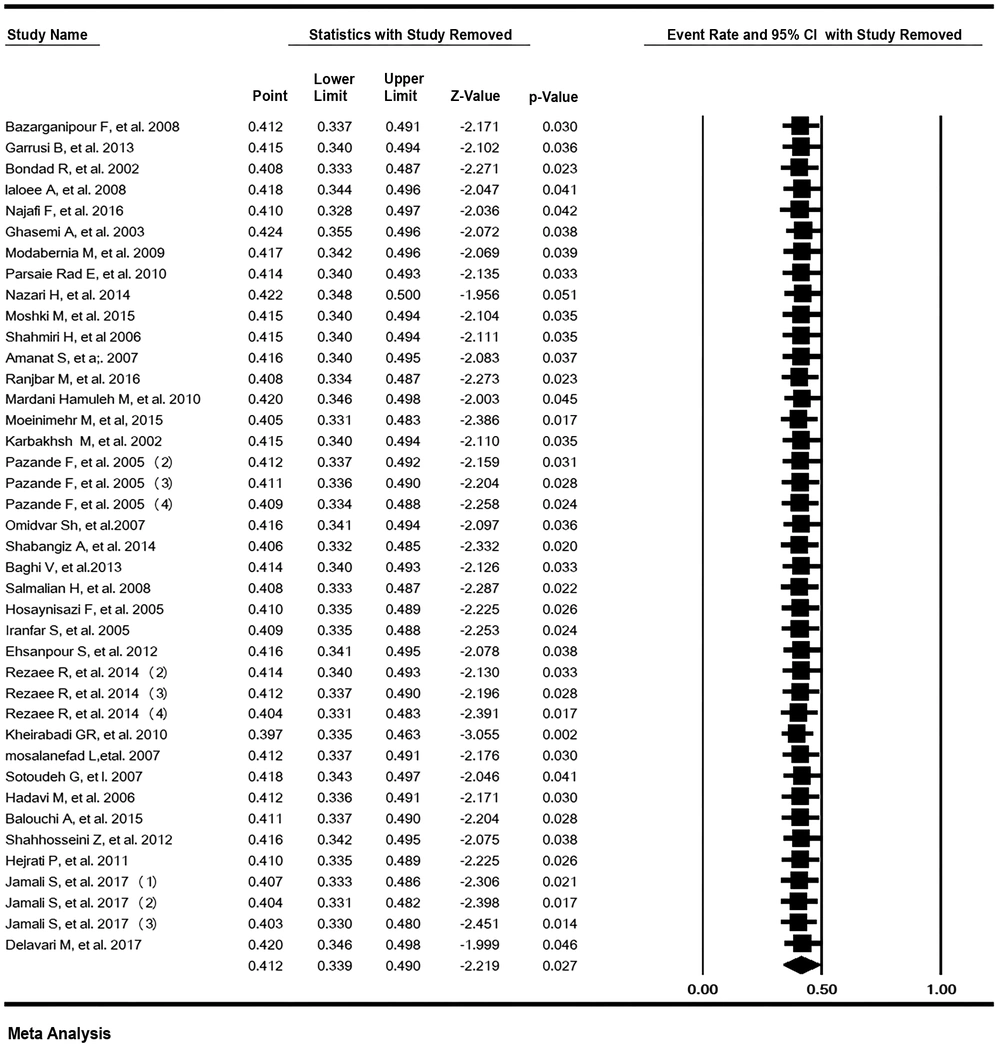
The heterogeneity of the studies was estimated to be high (I2 = 99.70%, P < 0.001). The prevalence of depression in pregnant Iranian women was estimated to be 41.22% (95% CI: 33.88 - 48.96). The lowest and highest prevalence was found in Ghasemi’s study (20) in Tehran in 2002 (10.5%) and Kheirabadi’s study (40) in Isfahan in 2007 (88.7%), respectively (Figure 2). The results of sensitivity analysis showed that the overall estimated point after omitting one study for the prevalence of depression was robust (Figure 3).
3.4. Subgroup Analysis Based on Geographical Region
The subgroup analysis of the prevalence of depression in pregnant women according to the geographical region is shown in Table 2. The lowest and highest prevalence of depression in pregnant women in Iran was related to the West of Iran (34.41% [95% CI: 17.38 - 56.67]) and the South of Iran (51.69% [95% CI: 37.32 - 65.78]), respectively, and the test result for subgroup analysis was not significant (P = 0.60).
3.5. Subgroup Analysis Based on Questionnaires
Most of the studies (57.5%) used Beck’s questionnaire to survey the prevalence of depression in pregnant Iranian women and the prevalence of depression according to this questionnaire was estimated to be 45.84% (95% CI: 35.47 - 56.60). The lowest prevalence of depression was in the General Health Questionnaire (GHQ) (21.53% [95% CI: 8.97 - 43.32]) and the highest prevalence of depression was in the Patient Health Questionnaire (PHQ) (70.10% [95% CI: 67.14 - 72.90]). The test result for subgroup analysis was significant (P < 0.001) (Table 2).
| Variable | Studies (N) | Sample (N) | Heterogeneity | 95% CI | Prevalence (%) | |
|---|---|---|---|---|---|---|
| I2 | P-Value | |||||
| Regions | ||||||
| Center | 17 | 10615 | 99.24 | < 0.001 | 27.67 - 53.11 | 39.69 |
| East | 3 | 638 | 94.74 | < 0.001 | 27.36 - 62.14 | 44.02 |
| North | 9 | 1851 | 95.77 | < 0.001 | 26.80 - 50.98 | 38.16 |
| South | 7 | 1986 | 97.31 | < 0.001 | 37.32 - 65.78 | 51.69 |
| West | 4 | 780 | 96.87 | < 0.001 | 17.38 - 56.67 | 34.41 |
| Test for subgroup differences | Q = 2.71, df (Q) = 4, P = 0.608 | |||||
| Questionnaires | ||||||
| Beck | 23 | 7985 | 98.60 | < 0.001 | 35.47 - 56.60 | 45.84 |
| SCL - 90R | 2 | 1666 | 99.20 | < 0.001 | 4.65 - 63.36 | 22.51 |
| DSSA21 | 4 | 2863 | 81.60 | 0.001 | 36.87 - 62.48 | 49.65 |
| GHQ | 3 | 705 | 96.20 | < 0.001 | 8.97 - 43.32 | 21.53 |
| EPDS | 6 | 1385 | 94.85 | < 0.001 | 23.03 - 46.32 | 33.68 |
| Zung | 1 | 300 | 0 | - | 26.97 - 37.49 | 32.00 |
| PHQ - 9 | 1 | 966 | 0 | - | 67.14 - 72.90 | 70.10 |
| Test for subgroup differences | Q = 165.08, df(Q)=6, P < 0.001 | |||||
| Trimester | ||||||
| First | 4 | 684 | 85.99 | < 0.001 | 39.91 - 61.08 | 50.52 |
| Second | 5 | 1157 | 97.33 | < 0.001 | 26.92 - 64.42 | 44.96 |
| Third | 17 | 8722 | 98.82 | < 0.001 | 36.64 - 60.20 | 48.33 |
| All | 12 | 5307 | 98.60 | < 0.001 | 20.83 - 43.61 | 30.83 |
| Test for subgroup differences | Q = 5.96, df (Q)=3, P = 0.113 | |||||
Abbreviations: CI, Confidence interval; N, Number.
3.6. Subgroup Analysis Based on the Trimester of Pregnancy
The subgroup analysis of the prevalence of depression in the first, second, and third trimester of pregnancy was estimated to be 50.52% (95% CI: 39.91 - 61.08), 44.96% (95% CI: 26.92 - 64.42), and 48.33% (95% CI: 36.64 - 60.20), respectively, and the test result for subgroup analysis was not significant (P = 0.11).
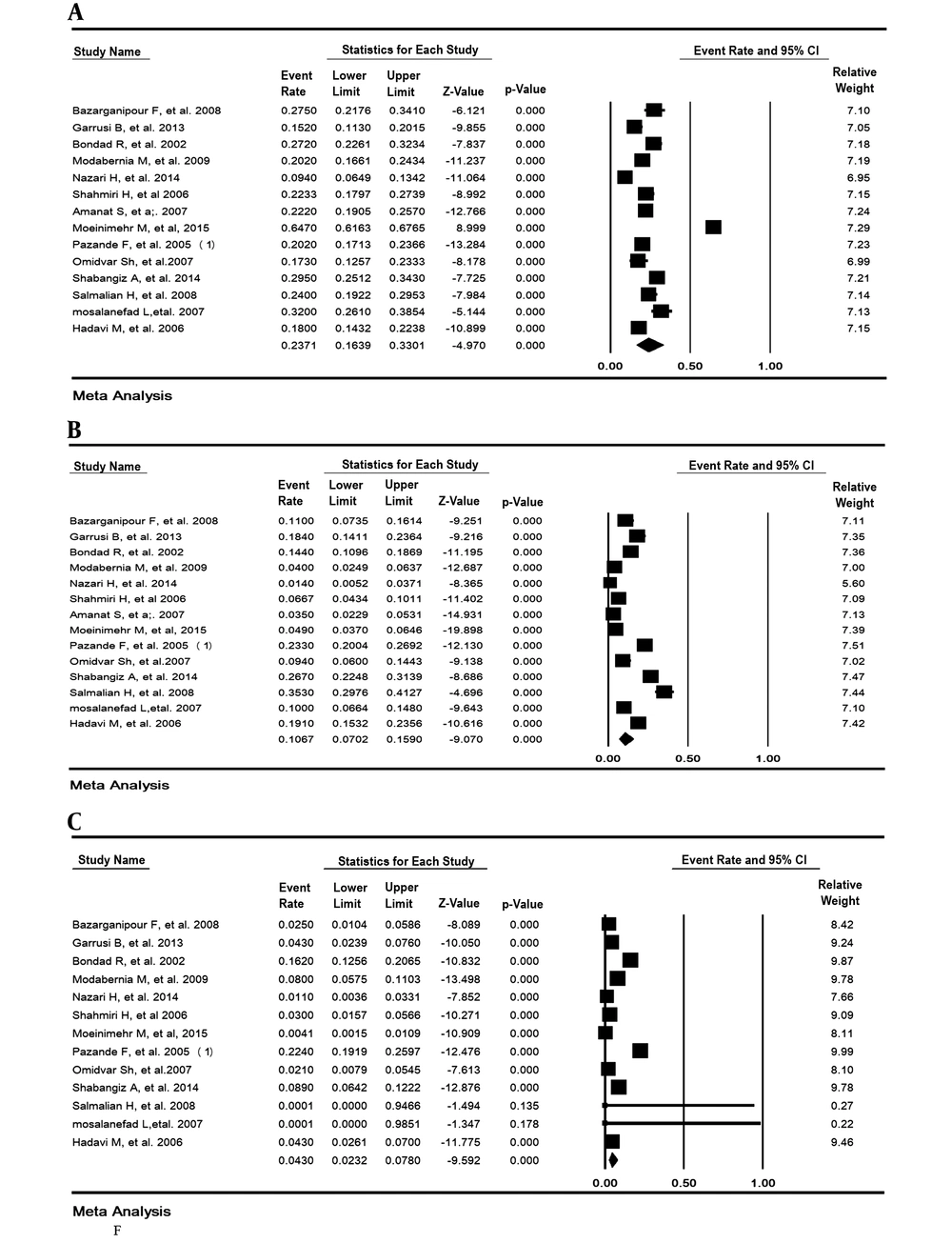
3.7. Prevalence of Depression Based on the Intensity
The prevalence of mild, moderate, and severe depression in pregnant women was estimated to be 23.71% (95% CI: 16.39 - 33.01), 10.67% (95% CI: 7.02 - 15.98), and 4.30% (95% CI: 2.33 - 7.80), respectively (Figure 4).
3.8. Meta-Regression
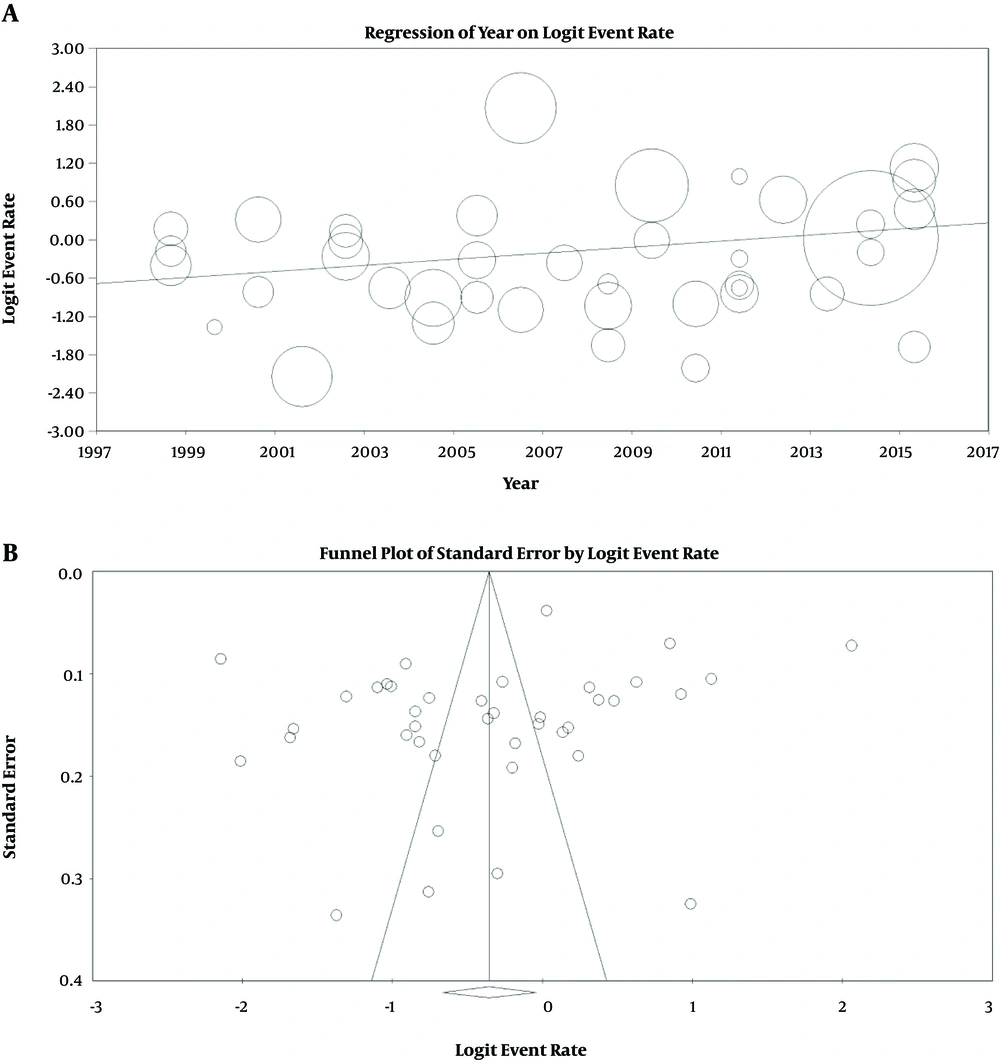
The prevalence of depression in pregnant women in Iran had a significantly increasing trend according to the year of study (P < 0.001) (Figure 5).
3.9. Publication Bias
The P-value for publication bias in Egger and Begg’s tests was estimated to be 0.08 and 0.33, respectively, which was not statically significant (Figure 5).
4. Discussion
The present study is the first systematic review and meta-analysis on the prevalence of depression during pregnancy in Iran. In this study, heterogeneity was 99.7%. There are three categories for heterogeneity: below 25% (low heterogeneity), 25 - 75% (moderate heterogeneity), and over 75% (high heterogeneity) (53, 54); therefore, the present study is in the high heterogeneity category and a random effects model was used in the meta-analysis. The overall and sub - grouped prevalence of depression in pregnant women were studied based on geographical regions, the used questionnaires and trimester of pregnancy. The overall prevalence of depression during pregnancy in Iran was 41.22%.
According to the systematic reviews and meta-analyses in other countries, the prevalence of depression has been reported to be 7.4% to 12% (5, 56, 57), indicating that the prevalence of depression during pregnancy among pregnant Iranian women is higher than in other countries. This difference may be due to the lack of social support and the difference in addressing psychological problems during pregnancy besides the development of these countries in health services or in medical material compared to developing countries such as Iran. Moreover, according to a review article of 15 studies by Veisani and Sayehmiri (58), the prevalence of postpartum depression in Iran was reported to be 28.7%, which is lower than the results of the present study. This indicates that the importance of depression in Iranian pregnant women during pregnancy is higher compared to postpartum depression. The American College of obstetricians and gynecologists suggests that screening for depression during pregnancy should also be considered potentially after the delivery (59). The weak points of the study of Veisani and Sayehmiri (58) compared to this study are the smaller sample size and non-random selection of samples in most studies that entered the meta-analysis process.
Several questionnaires including Beck, Symptom Checklist 90-Revised (SCL-90R), Depression anxiety stress scales- 21 (DSSA21), GHQ, PHQ and Edinburgh postnatal depression scale (EPDS) were used in these studies and the prevalence of depression in pregnant women in Iran was reported to be 10% - 89%. Possibly the most obvious cause of this difference is the diversity of diagnostic tools used in the studies. For example, in the study of Moshki et al. (24), who used EPSS questionnaire to assess depression, 30% depression was reported. Bondad et al. (17) estimated the prevalence of depression to be 58% with the Beck questionnaire. That is why a subgroup based on the diagnostic tool was also analyzed and it was found that most studies (57.5%) used Beck questionnaire and prevalence of depression during pregnancy in Iran, according to the Beck questionnaire was estimated to be 45.84%, and the overall estimate was not significant, while the test result for subgroup analysis according to questionnaires was significant.
The prevalence of depression in term of intensity during pregnancy was estimated to be 23.71%, 10.67%, and 4.30% for mild, moderate, and severe depression, respectively, while the highest prevalence of depression was in the mild range. This suggests that clinical and psychological programs and treatments can prevent the development of depression in pregnant women and thus prevent fetal and maternal complications of depression.
In the present study, the prevalence of depression in the first, second, and third trimester of pregnancy was 50.52%, 44.96%, and 48.33%, respectively. A review article by Bennett et al. (56) reported the prevalence of depression in the first, second, and third trimester of pregnancy to be 7.4%, 12.8%, and 12%, respectively, which is much lower than our results. Experiences of women in any trimester of pregnancy are based on their individual experiences. The first, second, and third trimesters are respectively the stage of pregnancy admission process with ambivalent feelings (pleasure and hate) about the fetus, embryo adoption stage with a primary focus on the fetus, narcissism and depression, and finally, the preparation stage of pregnancy associated with increasing dependence of pregnant women to people around them (60).
The most comprehensive study in terms of sample size and methodology is related to a study by Najafi and Kiani (19), in Tehran among 2,721 women in the third trimester of pregnancy, reporting the prevalence of depression during pregnancy as 50.7%. This finding is consistent with our estimates.
4.1. Study Limitation
1) National databases did not provide the possibility for a combined search.
2) Blood and hormonal risk factors were not considered in any of the studies.
3) There were no study to check job satisfaction, pregnancy satisfaction, etc which can effect depression among women in pregnancy.
Considering the prevalence of depression in this study and the importance of maternal and fetal complications before and after birth, identification and treatment of depression seem essential. Hence, it is recommended that medical policy-makers design and implement plans for improving the mental health in pregnant Iranian women.