1. Context
Breast cancer is the most common type of cancer in women (1-3). It accounts for 33% of all cancers and 19% of deaths due to cancer in women and is the second leading cause of death after lung cancer (3, 4). The diagnosis of breast cancer is considered to be a stressful event that causes a crisis in the lives of women (5, 6). The highest stress levels in women with breast cancer are related to occupational status, the decrease in self-efficacy, inability to adapt to the current situation, fears about death, and changes in body image and femininity (7, 8).
Coping strategies are effective ways to manage and overcome these stresses (6, 9, 10). The goal of coping is to modify maladaptive attempts and methods to manage stressful situations and adjust to a threat; more effective coping skills lead to less stress and fewer consequences from stress (11). Because coping strategies can predict breast cancer patients’ emotional well-being (12), women must access to effective interventions to improve their coping skills.
Effective interventions include cognitive-behavioral therapy (CBT) (11, 13, 14), spiritual-religious interventions (SRI) (13), mindfulness (15), self-management (16), and acupuncture (17). However, these interventions have different effects on coping skills. For example, the study by Behzadipour et al. (11) examined the effect of CBT on the coping skills of women with breast cancer and found that it increased the use of problem-focused coping skills, whereas decreased using emotion-focused coping skills. However, Ghahari et al. (13) investigated the effects of CBT and found that it did not significantly increase the coping skills of breast cancer women.
Since the results of these studies regarding coping strategies-oriented intervention in breast cancer, women have indicated a contradiction between previous studies; therefore, a systematic review is needed to overcome these inconsistencies between the initial studies. This study was done to review a series of relevant studies to make the readers able to use the results of multiple studies on the same topic simultaneously (3, 18). Also, a comprehensive overview of the available literature showed that there was only one systematic review on coping strategies-oriented interventions in breast cancer women as the couple-based psychological intervention, in which the women with breast cancer were studied (19). No exclusive and comprehensive investigation has been performed on all interventions on coping strategies.
2. Objectives
The aim of the present study was to review the coping strategies-oriented interventions in women with breast cancer.
3. Methods
3.1. Review Question
“What is known from existing literature about coping strategies-oriented interventions in breast cance?”
3.2. Inclusion Criteria
All studies considered for the systematic scoping review met the following inclusion criteria: clinical or quasi-experimental clinical trials using interventions and control groups, being published from 2009 - 2018, reported sample size, focusing on the coping strategies-oriented interventions in breast cancer women, the full text written in English or Persian, and the reported results of the interventions. Studies that did not meet these criteria and those their abstracts had been presented at congresses without the full text were excluded from the study.
3.3. Search Methods for Identification of Studies
A systematic scoping review of articles published from 2009 - 2018 was conducted using a comprehensive search of databases, such as PubMed, Scopus, Springer, Elsevier, Cochrane Library, Science Direct, Web of Science, Magiran, Scientific Information Database, and Google Scholar. Other sources were searched manually. References of the selected articles were used to find other relevant studies. The last search was done on December 27, 2018. The researchers used the following English keywords or equivalent Persian words in their search strategy: “Coping” OR “Coping strategy” OR “Coping skill” OR “Coping behavior” OR “Behavior adaptive” AND “Breast cancer” OR “Breast neoplasm” AND “Interventions” AND “Supportive intervention” AND “Counseling” AND “Psychological intervention” AND “Social intervention” AND “Support group” AND “Group counseling” AND “Cognitive-behavioral” AND “Mindfulness” AND “Education” AND “Supportive program” AND “Social support” AND “Religion intervention” AND “Spirituality intervention”.
3.4. Data Collection and Analysis
All relevant studies, reports, and documents were extracted using systematic and advanced searching. Duplicated articles were excluded. Irrelevant articles, which were identified by the title, abstract, or full text, were also excluded. Two independent researchers selected the final papers. In the case of a disagreement, the third researcher made the final decision. The quality of the included studies was assessed using the Jadad scale. This scale has direct and indirect sections to assess the risk of bias control (20). The direct section consisted of three items used to evaluate randomization, double-blinding, and dropout rate, while the indirect section assessed eight items (20, 21). Several studies included only the three direct items, whereas others applied both direct and indirect items (3, 22, 23).
In this study, the three direct items were evaluated using the Jadad scale with the application for all areas in medical science. The scoring system for the three direct items was as follows: The first item was related to the randomization of the samples using an appropriate method. The score ranged from 0 to 2: a score of 1 was given for randomization, and a score of 2 was given for mentioning the steps and using an appropriate randomization method. The second item referred to the double-blindness of the study; the score ranged from 0 to 2: A score of 1 was given if the term double-blind was mentioned in the study, while a score of 2 was assigned if the steps and using an appropriate double-blindness method was described. The third item referred to the number and causes of dropout; the score ranged from 0 to 1: A score of 1 was given if the number of dropouts and the reasons for the dropouts were reported in the study (20). The overall Jadad score was 5 points. A Jadad score of less than 3 indicates a study with poor quality, whereas a score of greater than 3 indicates a study with good quality (20, 21).
3.5. Extracting and Charting the Results
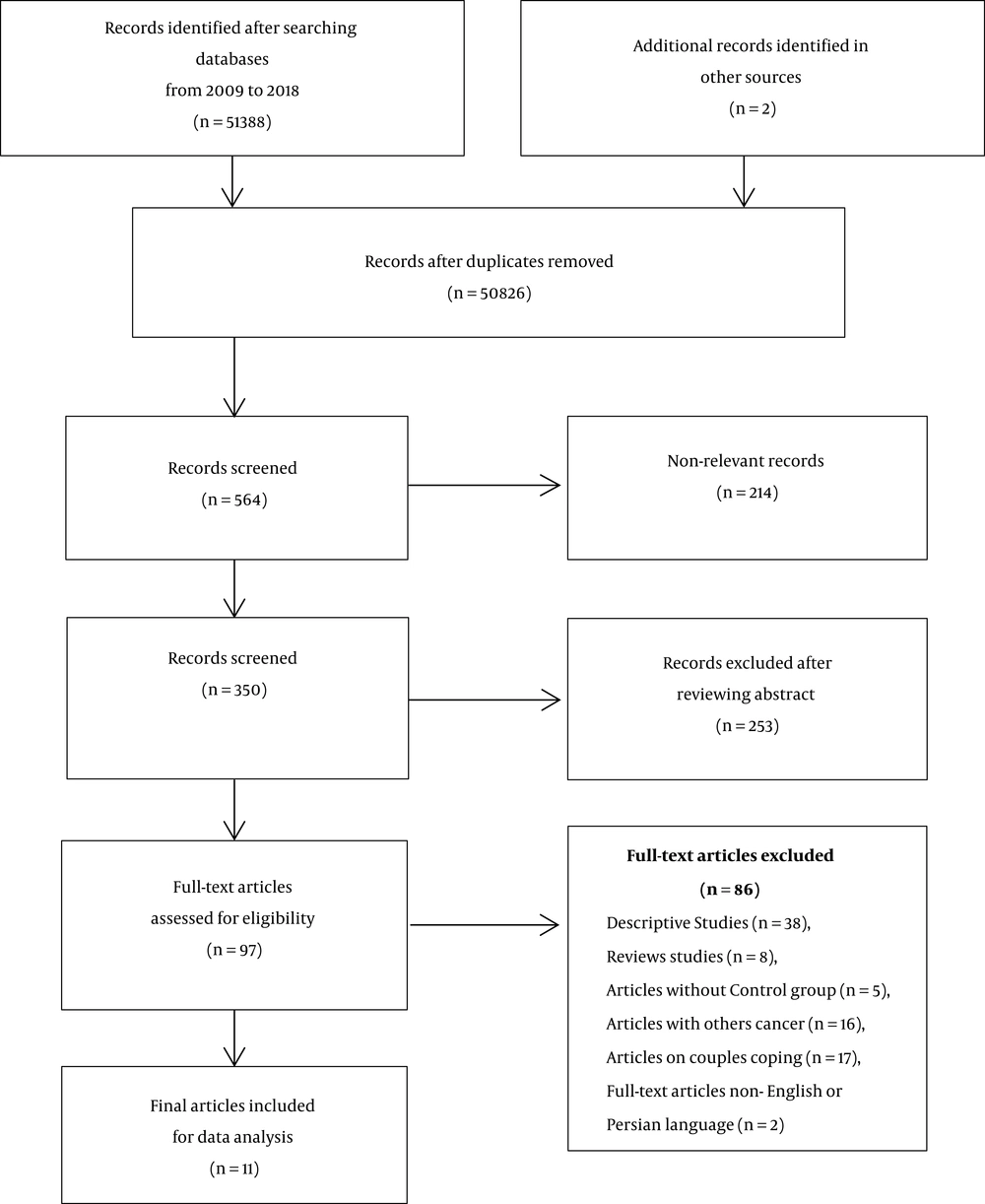
Data were extracted following the assessment and review of the abstract and the full text of the eligible articles. The data required for each research included the name of the author/year, study location, objective, samples’ age, sample size, used research tools, type and duration of follow-up, and results. Finally, the extracted data were classified and reported as the full text of the current systematic review. From the 51,390 articles that were obtained using the search strategies, 350 studies were retained after the duplicates and irrelevant studies were removed. After the abstracts of the articles were reviewed, 253 studies were excluded, while 86 studies were excluded after studying their full-text. Finally, 11 studies were selected for the current systemic scoping review (Figure 1).
4. Results
4.1. Description of Studies
The participants in all studies were women with breast cancer who were undergoing or had undergone different types of treatments. One study investigated patients undergoing chemotherapy (24), one study observed patients undergoing chemotherapy and radiotherapy (15), and one study investigated patients undergoing chemotherapy and hormone therapy (16). In one study, patients were undergoing mastectomy (17). One study had investigated interventions in newly diagnosed patients (25), patients who had completed their treatment course had been observed in one study (13), and patients with at least 1 year since the date of diagnosis had been investigated in one study (26). Patients’ age ranged from 18 - 75 years; however, the age range had not been mentioned in one study (Table 1) (14).
| Number | Authors/ Year/ Location | Study Type | Sample Size | Age, y | 1) Type of Intervention; 2) Duration; 3) Follow-Up | Results |
|---|---|---|---|---|---|---|
| 1 | Moghaddam Tabrizi and Alizadeh/2018/Iran (24) | Randomized clinical trial | 60 women (30 women in each group) | 20 - 60 | 1) Family-intervention based on FOCUS-group programs; 2) six 90-120-min sessions per week; 3) before and after the intervention | Family-intervention based on FOCUS-group programs improved coping strategies. |
| 2 | Ghahari et al./2017/Iran (13) | quasi-experimental trial | 45 women (15 women in each group) | ≥ 30 | 1) Cognitive-behavioral Therapy (CBT) and spiritual-religious intervention (SRI); 2) eight sessions of CBT and SRI, 1 session per week; 3) before and after the intervention | The CBT and SRI improved coping responses, but not significantly. |
| 3 | Quinlan-Woodward et al./2016/USA (17) | Randomized clinical trial-pilot | 30 women (15 women in each group) | ≥ 18 | 1) Acupuncture intervention; 2) a session of acupuncture for an average of 36 minutes; 3) Before, and one and two days after mastectomy | Acupuncture intervention increased the ability to cope with symptoms in the first and second days after mastectomy surgery. |
| 4 | Farajzadegan et al./2015/Iran (26) | Randomized clinical trial | 62 women (31 women in each group) | 18 - 60 | 1) Coping therapy intervention; 2) eight 1- hour sessions per week; 3) before and immediately after 8 weeks of intervention | Coping therapy significantly improved the problem-focused coping skills, but the effect of the emotion-focused coping strategy was not significant. |
| 5 | Shoaa Kazemi/2013/Iran (14) | Randomized clinical trial | 30 women (15 women in each group) | - | 1) Group psychotherapy (CBT); 2) Eight 1.5 - 2 h sessions; 3) before, immediately, and one month after the intervention | Group Psychotherapy (CBT) improved the problem-focused coping strategies and reduced the use of emotion-focused coping strategies and was also steady at 1-month follow-up. |
| 6 | Behzadipour et al./2013/Iran (11) | Quasi-experimental trial | 30 women (15 women in each group) | 30 - 50 | 1) CBT; 2) ten 2-hour sessions weekly; 3) before, immediately, and 2 months after the intervention | CBT improved coping skills in women with breast cancer so that the intervention increased the use of problem-focused coping strategies and reduced the use of emotion-focused coping strategies. |
| 7 | Kang and Oh/2012/South Korea (15) | Quasi-experimental trial | 50 women (25 women in each group) | 30 - 50 | 1) Mindfulness; 2) eight 3-hour sessions weekly; 3) before and after the intervention | Mindfulness significantly reduced the use of emotion-focused coping strategies and insignificantly improved the use of problem-focused coping strategies. |
| 8 | Loh and Quek/2011/Sweden (16) | Randomized clinical trial | 147 women (69 women in the intervention group and 78 women in the control group) | ≥ 18 | 1) Self-management; 2) four sessions of 2 hours per week; 3) before and after the intervention and follow-up (no mentioned follow-up period) | Self-management improved self-care, which has a significant relationship with coping behavior and cancer. |
| 9 | Hamilton et al./2011/Canada (27) | Quasi-experimental trial | 38 women (20 women in the intervention group and 18 women in the control group) | Mean age: 60.6 | 1) Positive self-talk (PST); 2) workshop and group session for 2 hours; 3) before, immediately, and one month after the first intervention session | PST increased coping strategies to cope with breast cancer, but it was not significant. |
| 10 | Cousson-Gelie et al./2011/France (28) | Randomized clinical trial | 65 women (G1 = 22 women, G2 = 14 women, G3 = 29 women) | 35 - 75 | 1) Group G1 received a specific psychoeducation and group G2 received a support group; 2) eight 2-hour sessions weekly; 3) one week before the intervention and immediately after the intervention | Psychoeducation did not significantly affect the different dimensions of coping skills. |
| 11 | Beatty et al./2010/Australia (25) | Randomized clinical trial | 49 women (25 women in the intervention group and 24 women in the control group) | ≥ 18 | 1) Self-help workbook; 2) the duration of the intervention is not mentioned; 3) a 3-6-month follow-ups | Self-help workbook significantly reduced coping strategies (cognitive avoidance and helplessness-hopelessness), but its effect was not significant after 3-6-month follow-ups. |
4.2. Risk of Bias in Included Studies
The abstracts of 253 studies and the full-text of 97 studies were reviewed. Also, 11 studies published from 2009 - 2018 that met the inclusion criteria of our systematic scoping review were investigated. According to the Jadad scale that was used to score the three direct items, only one study completely had described the randomization process (25), whereas two studies were non-randomized (15, 16). In addition, one study had a double-blind design (24). Only three studies did not fully describe the number and reasons for the dropout rate (11, 14, 16). Considering the Jadad score of the three direct items, only two of the evaluated studies were of good quality (24, 25). In general, the results of Table 2 indicate that most of the weaknesses of the studies were related to the lack of a description of the randomization process (Table 2).
| Row | Authors/Year | Jadad Scale Items (Directly) | Total Score | Quality of the Study | ||
|---|---|---|---|---|---|---|
| Was There a Description of the Withdrawals and Dropouts? | Was the Study Described as Double-Blinded? | Was the Study Described as a Randomized Study? | ||||
| 1 | Moghaddam Tabrizi and Alizadeh/2018 (24) | 1 | 2 | 1 | 4 | Good |
| 2 | Ghahari et al./2017 (13) | 1 | 1 | 1 | 3 | Good |
| 3 | Quinlan-Woodward et al./2016 (17) | 1 | 0 | 1 | 2 | Poor |
| 4 | Farajzadegan et al./2015 (26) | 1 | 0 | 1 | 2 | Poor |
| 5 | Shoaa Kazemi et al./2013 (14) | 0 | 0 | 1 | 1 | Poor |
| 6 | Behzadipoour et al./2013 (11) | 0 | 0 | 1 | 1 | Poor |
| 7 | Kang and Oh/2012 (15) | 1 | 0 | 0 | 1 | Poor |
| 8 | Loh and Quek/2011 (16) | 0 | 0 | 0 | 0 | Poor |
| 9 | Hamilton et al./2011 (27) | 1 | 0 | 1 | 2 | Poor |
| 10 | Cousson-Gelie et al./2011 (27) | 1 | 0 | 1 | 2 | Poor |
| 11 | Beatty et al./2010 (25) | 1 | 0 | 2 | 3 | Good |
The coping skills of the women were the measured outcomes in all included studies. Only one study had measured the coping skills using a self-report questionnaire (17). Two studies had used the Ways of Coping questionnaire (11, 15), and another two studies had used the Mental Adjustment to Cancer scale to measure coping skills (25, 28). Two studies had used the Coping Responses Inventory to measure coping strategies (13, 14). Also, other studies had employed the Cancer Coping questionnaire (24), Brief-COPE questionnaire (26), cancer behavior inventory (16), and rehabilitation survey of problem and coping to assess coping strategies (27). The coping strategies-oriented interventions were divided into four general categories, as follows: psychological, spiritual-religious, social, and complementary interventions.
4.3. Psychological Interventions
4.3.1. Cognitive-Behavioral Therapy (CBT)
CBT is a combination of cognitive and behavioral therapies, mainly focusing on the role of thoughts, beliefs, and misconceptions to achieve adaptive thoughts and behaviors. Four studies had examined the effect of CBT on the coping skills of women with breast cancer (11, 13, 14). In three studies, an 8-10-session intervention had been held once per week for 1.5 - 2 h (11, 13, 14), and one study involved a 2-hour workshop for women with breast cancer (27). All studies had used group interventions (11, 13, 14, 27). The results of two studies showed that CBT improved the problem-focused coping skills and reduced the use of emotion-focused coping skills, and the results were statistically significant (11, 14). The results of the two studies indicated that CBT and using positive self-talking (PST) improved the coping strategies, but the results were not statistically significant (13, 27).
4.3.2. Mindfulness
Mindfulness is the purposeful attention to current situations and is free of prejudice and judgment about the present reality (22, 29). Two studies had examined the effect of mindfulness on the coping strategies in women with breast cancer (15, 25). In one study, 8 3-hour sessions of mindfulness therapy had been provided once per week (15).
Another study had evaluated the effectiveness of a self-help workbook on improving the coping skills of women who had been recently diagnosed with breast cancer (25). The results of one study showed that mindfulness significantly had reduced the use of emotion-focused coping skills and insignificantly improved using problem-focused coping skills (15). According to the results of another study, the self-help workbook significantly reduced coping skills (cognitive avoidance and helplessness-hopelessness), but it was not significant after the follow-ups of 3 and 6 months (25).
4.3.3. Coping Therapy
Coping therapy is a part of the CBT and includes problem-focused coping skills, which concentrate on changing and correcting problems and emotion-focused coping skills based on managing emotions. One study had examined the effect of coping therapy on women with breast cancer who had maladaptive coping skills (26). In this study, eight 60-min sessions of coping therapy were provided once per week, and based on its results, coping therapy significantly improved the problem-focused coping skills, but the effect of emotion-focused coping skills was not significant (26).
4.3.4. Self-Management
Self-management is a method in which a patient plays an active role in developing coping skills. Self-management programs are a combination of strategies that increase self-efficacy and self-management behaviors leading to promoting well-being (30). The effect of self-management (through four 2-hour sessions once a week) on the coping behaviors of women with breast cancer had been examined in one study (16). The result of this study showed that self-management improved self-care, which has a significant relationship with coping behavior and cancer (16).
4.3.5. Psychoeducation
Psychoeducation is a psychological intervention that affects the coping skills of women with breast cancer. One study had assessed the effect of psychoeducation on the coping strategies in women with breast cancer (27). In a study, 22 women had received special psychoeducation interventions, and 14 women had been provided with a health-related support group of eight 2-hour group sessions twice per week. The result of this study showed that psychoeducation did not affect the different dimensions of coping skills (27).
4.4. Spiritual-Religious Interventions
Spiritual-religious interventions (SRI) and beliefs affected the coping skills, life expectancy, and meaning of life retrieval, and also reduced psychological complications, which ultimately improved the quality of life of the patients (31, 32). Only one study evaluated the effect of SRI on improving the coping responses in women with breast cancer (13). The result of this study reported that SRI (through eight sessions) did not significantly improve the coping responses in women with breast cancer (13).
4.5. Social Interventions
Social support, especially from family, friends, peers, and healthcare providers, had a positive effect on the coping skills of patients with breast cancer (5, 33, 34). One study had measured the effectiveness of social interventions (six 90-120-min sessions once per week using individual and group counseling) involving family members on the coping skills of patients with breast cancer who were undergoing chemotherapy (24). Its results showed that FOCUS program family-based intervention improved coping skills (24).
4.6. Complementary Interventions
Acupuncture is a non-pharmacological and complementary intervention that can be effective in reducing the pain and the side effects due to the treatments, as well as the individuals’ ability to cope with cancer. One study has studied the effect of acupuncture on the coping ability of 15 women undergoing a mastectomy. An acupuncturist performed the intervention through 36 min (17). Acupuncture intervention increased the ability to cope with symptoms in the first and second days after mastectomy surgery (17).
5. Discussion
In the current systematic scoping review, 11 studies were evaluated. This review focused on coping strategies-oriented interventions in breast cancer women. Based on the results of this study, some interventions were shown to be effective in improving the coping skills of women with breast cancer. Thus, it is recommended that appropriate interventions be developed and implemented by healthcare providers to promote coping skills and improve the health of women who have been diagnosed with breast cancer.
One of the findings of this study was the effectiveness of psychological interventions in the coping skills of women with breast cancer. The studies by Behzadipour et al. (11) and Shoaa Kazemi (14) had examined the effect of CBT on the coping skills of women with breast cancer and found that it increased the use of problem-focused coping skills and decreased using emotion-focused coping skills. However, Ghahari et al. (13) investigated the effects of CBT and found that it did not significantly increase the coping skills of women with breast cancer.
Mindfulness was another psychological intervention that affected the coping skills of women with breast cancer. Kang and Oh (15) reported that a mindfulness technique reduced the use of emotion-focused coping skills in patients with breast cancer; however, it was not significantly effective in increasing the use of problem-focused coping skills.
Farajzadegan et al. (26) examined the effect of coping therapy on women with breast cancer who used maladaptive coping strategies and reported that it significantly improved their problem-focused coping skills, but did not affect their emotion-focused coping skills.
Loh and Quek (16) reported that self-management programs improved self-care and had a significant relationship with the coping behaviors in women with breast cancer.
Psychoeducation is a psychological intervention that affects the coping skills of women with breast cancer. However, Cousson-Gelie et al. (28) revealed that psychosocial interventions had no significant effect on coping skills.
A review of the studies showed that most psychological interventions were effective in improving coping skills; however, some interventions were not. For example, Ghahari et al. (13) reported that CBT intervention had no significant effect on coping skills. The participants in the study were women who had been diagnosed with breast cancer in the past 2 years and had completed chemotherapy and radiotherapy. Thus, it seemed that the women had acquired the necessary coping skills during their treatment, which may explain the ineffectiveness of the intervention. In one study (13) using psychological interventions, such as CBT, the sample size was small, which affected the generalizability of the findings to the target population. It should be noted that in studies (13, 27) that had found that the interventions had no effect or no significant effect on the coping skills the factors affecting the intervention, such as economics, culture, social state, comorbidities, psychiatric disorders, and treatment type had not been considered.
Another finding of this study was the effect of SRI on the coping skills of breast cancer women. Ghahari et al. (13) reported that SRI did not significantly improve the coping responses in women with breast cancer; however, this result could be due to the very small sample size and the ignoring psychiatric disorders and economic, social, and cultural situations of the patients.
Another finding of the present study was the impact of social interventions on coping skills in breast cancer women. Moghaddam Tabrizi and Alizadeh (24) examined patients with breast cancer who were undergoing chemotherapy and showed that a FOCUS program family-based intervention, improved the coping skills of the patients.
This study also assessed the effect of complementary interventions on the coping skills of women with breast cancer. Quinlan-Woodward et al. (17) examined women who had a mastectomy and reported that acupuncture increased the woman’s ability to cope with the symptoms related to the treatment of the disease 2 days after mastectomy (17).
In summary, the obtained results indicated that most interventions improved the coping skills of women with breast cancer. However, four studies had reported that the interventions were ineffective. Economics, culture, social status, comorbidities, psychiatric disorders, treatment type, and sample size should be considered when evaluating the effect of an intervention.
The limitations of this study included the heterogeneity between the studies in terms of the variability of the instrument used, which did not allow for a meta-analysis. Another limitation of this study was the inaccessibility to the full-text of some articles and the exclusion of non-English or non-Persian studies. Despite these limitations, this review had some strengths, such as implications for the health care system:
5.1. Implication for Clinic
According to the importance of effective adaptation of coping strategies regarding breast cancer and using interventions, such as effective psychological interventions to improve coping strategies, it seems that using effective interventions by experienced health workers in breast cancer health centers and clinics is appropriate.
5.2. Implication for Research
This systematic scoping review investigated coping strategies-oriented interventions in breast cancer women. The findings of this study can be used to design, implement, and evaluate quality interventions. Therefore, it is recommended to conduct a meta-analysis to evaluate coping strategies-oriented interventions in breast cancer women.
5.3. Implication for Policymakers
The results of this study can be an effective step towards providing effective interventions, such as psychological interventions to breast cancer women, to assist health care providers and health policy makers because the family and community health is affected by the health of women in society.
6. Conclusions
Considering the importance of coping skills for the adaptation to life after cancer and better quality of life in these patients, it is suggested that healthcare providers should provide detailed plans and apply appropriate methods to promote the coping skills and improve the health of women with breast cancer. However, there remains a need for further culture-based specific research to adopt the best interventions and make changes in policy.