Introduction
Medication errors (MEs) as one of the most common types of medical problems in healthcare institutions (1, 2), are a leading cause of patient harm (3) and a worldwide concern (4, 5).
ME is defined as “a failure in the treatment process that leads to, or has the potential to lead to, harm to the patient” (6). It has been estimated that between 10% and 18% of all reported hospital harms can be attributed to MEs with varied ranges of effects, from going unnoticed to causing death (1).
MEs may occur in any phase of medication process (4). In an update review of literature on Iranian MEs studies, prevalence of MEs in different stages were as follows: prescribing (29.8% to 47.8%), transcribing (10.0% to 51.8%), dispensing (11.3% 33.6%) and administration (14.3% to 70%) (7). Preventing MEs depends on awareness of the causes or contributing factors (3, 5); therefore, health care organizations are advised to monitor errors by establishing and promoting organization-wide reporting systems to find possible sources of ME (3).
Evidence from ME reporting systems suggests that many MEs are not reported, for different individual and contextual reasons, and therefore go undetected (3).
The resultant underreporting reduces the possibility of analyzing natures of MEs and developing quality improvement initiatives (8). As a developing country, Iran is no exception regarding underreporting of MEs (5) (4). Different studies have been published regarding the status and sources of MEs in Iran. But, there seems that evidence is lacking regarding the use of ME incidents in quality improvement in Iranian healthcare organizations (9).
Moreover, many preventive strategies have been used for reducing MEs and their complications. But, the effectiveness of many of these interventions is dependent on cultural context and circumstances. So, it is better to assess the effectiveness and suitability of ME prevention strategies in Iran’s context.
MEs can occur with any medicinal product (3); but, possibly due to scarcity of resources, many studies have been focused on commonly-used products or those drugs that have been frequently involved in ME reports. So, it is expected that studies on ME from Iran may have also been focused on commonly-used drugs and their possible consequences.
Limited number of studies on ME in developing countries makes it difficult to get a comprehensive picture on MEs (4, 5). Shortage of high-quality studies with well-designed methodologies also adds to the difficulties in providing reliable evaluation of MEs (5, 10).
In order to give details about sources, underreporting reasons, preventive measures, and also the most common drugs associated with MEs, we planned to review current available evidence.
Experimental
Databases
In order to review Persian and English language-literature on medication errors in Iran, we searched these English electronic databases to find articles related to sources, underreporting reasons, preventive measures, and also the most common drugs associated with MEs: Scopus, Web of Science, PubMed, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), and EBSCOHOST. We also searched these Persian electronic databases: Iran Medex, and Scientific Information Database (SID). We additionally searched references from relevant articles to identify additional studies. The time span was up to October 2012.
Search terms
We used these English terms and their corresponding Persian equivalents: administration error(s), administration mistake(s), dispensing error(s), dispensing mistake(s), documentation error(s), drug mistake(s), medication error(s), medication mistake(s), nurse(s), pharmacist(s), physician(s), prescribing error(s), prescribing mistake(s), transcribing error(s), transcribing mistake(s), wrong calculation(s), wrong dose(s), wrong drug(s), wrong medication(s), and wrong route(s) of administration. Each of the words were combined using “OR” and then combined using “AND” with (Iran OR Iranian OR I.R.Iran).
Inclusion/exclusion criteria
We considered all types of original studies on adults and children; i.e., clinical trials, cohort or case–control studies, and cross-sectional studies. We looked for studies which reported sources of MEs, reasons for not reporting MEs, preventive measures of MEs and most common drugs involved in MEs. Letters, case reports, conference papers, organizational reports, opinions or editorial papers were excluded. We also excluded articles focused on medical - not medication - errors and nursing practice errors. Moreover, we excluded articles on preventive measures which were solely focused on usability and acceptability of the measures themselves, not on the outcome of reducing MEs.
Selection and information extraction
Two authors independently selected and one of them reviewed the articles by following these stages: Inclusion and exclusion criteria were assessed both in reading the titles and abstracts of the search results. The data extraction tables comprised these sections which were examined in each article: sources, underreporting of, preventive measures for and drugs involved in MEs; unit of observation studied; sample size; study design and/or measurement tool(s); reported outcome(s); and main finding(s). Then we found all full-texts of the articles selected and the exclusion criteria were also applied to the full-texts.
We categorized the results from studies on sources of MEs using “framework of factors influencing clinical practice and contributing to adverse events” developed by Vincent C. in 2003 (11); we added an extra category entitled “medication” to what was suggested by Vincent.
We considered the results reported by more than 30% of studies in every category as the most frequent topic. We report the findings in different unit of observations based on their most frequent percentages.
Results
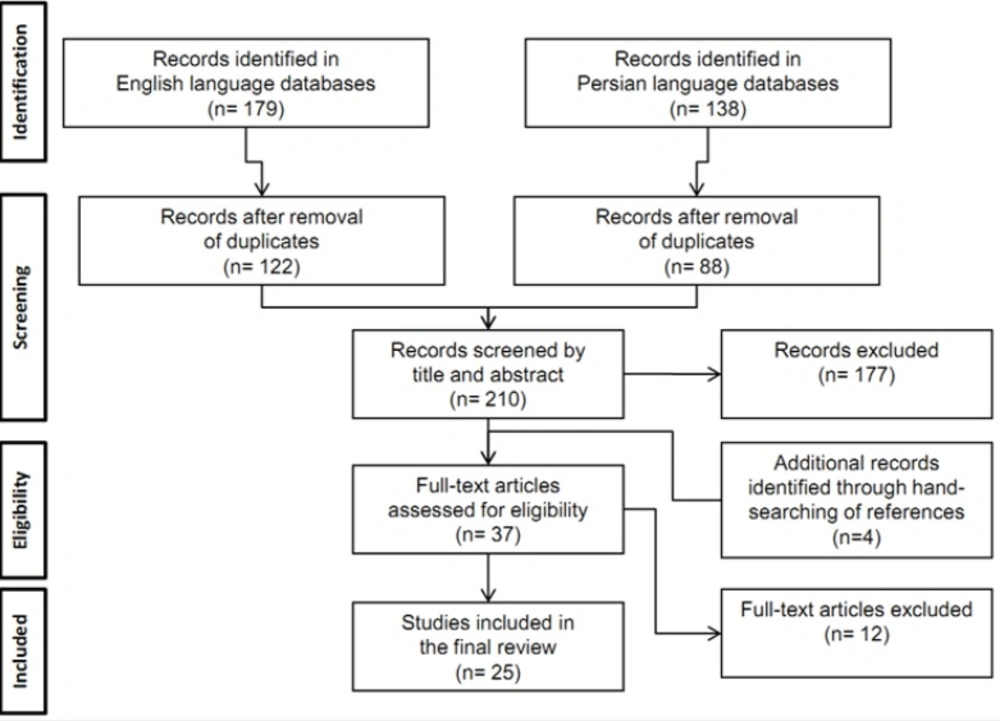
Initially, 122 and 88 studies were identified in English and Persian biomedical databases respectively, after removing the duplicates. Of the 210 studies, 177 were of no relevance to the current review according to their titles and abstracts. Twelve studies did not meet the inclusion criteria according to their full-text. After hand-searching of the reference lists of all primary studies, we added another 4 studies; this left us with 25 eligible studies for our final review. Figure 1 summarizes the complete process of selection.
Out of 25 studies, 12 of them reported sources of MEs, 11 assessed most frequent drugs involved in MEs, 5 focused on underreporting of and 5 on preventing measures of MEs.
The studies were published from 2007 onwards and all of them were conducted in hospital settings. Nursing staff and nursing students were the most frequent populations under observation. Except for 2 interventional studies, all other studies were cross-sectional.
Number of relevant studies
The 12 studies on sources of MEs investigated individuals (11), work environment (5), organization and management (4), team (4), tasks (2), and medications (2) as the possible causes of ME. Anti-infectives for systemic use (9) and cardiovascular system drugs (6) were the main drugs assessed in Iranian studies. Personal fears (5), reporting process (5) and administrative barriers (4), were the main areas of interest in studies focused on underreporting of MEs. Detailed characteristics of studies are summarized in Table 1.
| Categories of MEs | # of Studies | Publication Years | Units of Observation(# of studies) * | Study Design | Most Frequent Topics Covered |
|---|---|---|---|---|---|
| Sources of MEs | 12 | 2007-2012 | Cross-sectional | Individuals (10) | |
| Under-reporting of MEs | 5 | 2008-2012 | Nursing staff (4) | Cross-sectional | Fears (5) |
| Preventing measures of MEs | 5 | 2008-2011 | Nurses (1) | Cross-sectional; | **** |
| Drugs involved in MEs | 11 | 2007-2012 | Nurses (1) | Cross-sectional; | Anti-infectives for systemic use (9)*** |
Characteristics of studies on ME included in our final review with their most frequent topics covered
Sources of MEs
Only one out of 12 studies (8.3%) was in English. All study designs were cross-sectional. Most, not all studies, in this category reported the frequency of each source of ME as percentages; but few of them mentioned the importance of each source using a Likert scale with scoring from 1-5 in which score 5 corresponded to the highest degree of importance of the corresponding source of MEs.
Individual factors were regarded as accountable in 27.7% to 79.9% of MEs by nurses. The corresponding range was from 15.3% to 29.7% in nursing students.
All four studies which were performed on nursing students reported individual factors as the main and only source of MEs occurrence. Miscalculations of doses (100% of studies) with estimated prevalence between 13.5% and 20.0%, and inadequate knowledge of medications (75% of studies) with estimated prevalence between 11.4% and 18.9% were reported as the most frequent contributing factors.
In studies on nurses’ views shortage of workforce was accounted as one of the most reported sources (4 out of 5 studies; 80%) with regard to “organization and management”. It had one of the highest prevalence in all contributing factors (12.8% to 100.0%). Heavy workload had the estimated prevalence between 10.6% and 70.0% in different contexts and was reported in 80% of studies. Nurses also reported physical and mental health as the most frequent source of MEs at individual level which ranged from 48.7% to 79.9% in prevalence. Illegible handwritings (15.0% to 70.0%) and inadequate knowledge of medications (27.6% to 55.8%) was reported by nurses as the next most frequent individual factors.
In general, the most commonly-reported contributory factor to ME was individual factors (10 of 12 studies) in which the inadequate knowledge of medication (7 of 12 studies) was the most frequent reported one. The three most-commonly reported individuals contributing factors to MEs in all studies were personal problems (48.7% to 79.9% in different studies), inadequate knowledge of medication (11.4% to 55.8%), and dose miscalculations (13.5% to 20.0%).
We could not categorize two studies using Vincent’s framework; one of them assessed the association between nurses’ satisfaction from working conditions and frequency of their MEs (3) and the second, assessed sources of MEs from hospital officials’ viewpoint (6). The most frequent findings from studies on sources of ME are summarized in Table 2.
| Findings | Sources of Medication Errors | Study Design and/ or Measurement Tool | Sample Size | Unit of Observation | Author(s) / Year | |
|---|---|---|---|---|---|---|
| 12.76% | Organization and Management | Cross-sectional; | 64 | Nurses | (12)Cheraghi MA, et al. | 1 |
| Mean score SD | Organization and management | Cross-sectional; | 200 | Nurses | (13) Hosseinzadeh M, et al. | 2 |
| Mean score SD | Team | Cross-sectional; | 22 | Nurse instructors | (14)Baghcheghi N, et al. | 3 |
| 29.72% | Individuals | Cross-sectional; | 78 | Nursing students | (15) Mohammadnejad E, et al. | 4 |
| 62% | Organization and management | Cross-sectional; | 100 | Nurses | (16) Nikpeyma N, et al. | 5 |
| 100% | Organization and management | Cross-sectional; | 86 | Nurses | (17)Ghasemi F, et al. 2009 | 7 |
| 18.95% | Individuals | Cross-sectional; | 52 | Nursing student | (18) Baghcheghi N, et al. | 6 |
| 15.25% | Individuals | Cross-sectional; | 76 | Nursing student | (19)Koohestani HR, et al. | 8 |
| 20.00% | Individuals | Cross-sectional; | 60 | Nursing student | (20) Koohestani HR, et al. | 9 |
| 66.7% | Work Environment | Cross-sectional; | 40 | Nurses | (21) Souzani A, et al. | 10 |
| Studies which categorized sources of medication error un-comparable to classification by Vincent (11). | ||||||
| Mean | Work conditions | Cross-sectional; | 286 | Nurses | (10)Joolaee S, et al. | 11 |
| 7.29%a | Drug information | Cross-sectional; | 396 | Hospital officials | (22) Nasiripour AA, et al. | 12 |
Detailed characteristics of studies on sources of ME with their most frequent findings
Underreporting of MEs
Personal fears (Likert score range: 3.5 to 4.1), administrative barriers (3.6 to 3.8) and the reporting process (1.6 to 3.1) were the barriers for reporting MEs.
Ignoring to report as the most frequent barrier in MEs reporting (100% 0f studies) had the importance score between 1.4 and 3.5. Fear of “decreasing evaluation scores and introducing educational problems” had the highest importance (4.4 to 4.6) which was reported by nursing students. Nurses also declared focus on individual rather than system factors to MEs as the most important barrier (score 4.0).
Just one study reported the frequency of barriers; 23.3% for personal fears, and 14.5% for ignoring the report in the reporting process (23).
The most frequent findings from studies on reasons for underreporting of MEs are summarized in Table 3.
| Findings | Reporting of Medication Errors | Study Design and/ or Measurement Tool | Sample Size | Unit of Observation | Author(s) / Year | |
|---|---|---|---|---|---|---|
| Mean score | Fears | Cross-sectional; | 200 | Nurses | Hosseinzadeh M, et al. | 1 |
| Mean score | Fears | Cross-sectional; | 140 | Personnel | Tol A, et al. 2010(24) | 2 |
| 23.3% | Fear of | Cross-sectional; | 332 | Nurses; | Zahmatkeshan N, et al. | 3 |
| Mean score** | Fears | Cross-sectional; | 240 | Nursing students | 4 Koohestani HR, et al. | 4 |
| Mean score | Fears | Cross-sectional; | 76 | Nursing students | (26)Koohestani HR, et al. 2009 | 5 |
Detailed characteristics of studies on underreporting of ME with their most frequent findings.
Preventing MEs
We could not categorize the most frequent topics from studies on preventing MEs because of the diversity in reporting and the resultant inconsistencies in the findings. Details of findings from studies on preventing MEs are summarized in Table 4.
| Findings | Preventing Medication Errors | Study Design and/ or Measurement Tool | Sample Size | Unit of Observation | Author(s) / Year | |
|---|---|---|---|---|---|---|
| 91.2% | Before educational intervention | Non randomized clinical trial | 603 | IV administration by nurses | Sharifi N, et al. | 1 |
| 7.28a | Launching an electronic prescription system, proper medication labeling and packaging from pharmacy | Cross-sectional; | 396 | Hospital officials | Nasiripour AA, et al. 2011(28) | 2 |
| 40% | Increasing duration of theoretical education for pharmacology course | Cross-sectional; | 22 | Nurse instructors | Baghcheghi N, et al. | 3 |
| 52% | Prescription errors | Before-after interventional study | 248 | Patients | Kazemi A, et al. | 4 |
| 98.8% | Increasing number of staff proportional to patient load | Cross-sectional; | 86 | Nurses | Ghasemi F, et al. 2009 (17) | 5 |
Detailed characteristics of studies on preventing ME with their most frequent findings
Most common wards and most frequent drugs
The most common wards under assessment for ME were the intensive care units and internal medicine wards followed by critical care units and surgery wards.
Three studies did not report any frequencies of MEs with each drug or drug class. The reporting approach of the remaining 8 studies was very diverse; most of them mentioned specific drug names and frequency of corresponding MEs and the others just stated the overall drug classes.
Drugs with the highest prevalence involved in MEs ever were intravenous fluids in a pediatric ward (76.2%) and albumin in an internal medicine ward (62.0%). But generally, antibiotics were the most common drugs involved in MEs in different studies; the range of ME frequencies differed according to the wards and study populations of interest. Estimation of MEs in antibiotics administration by nurses varied widely from 11.0% for amikacin in an intensive care unit to 56.4% for ceftazidime in an internal medicine ward; the corresponding figure for nursing students was 4.6% for ceftazidime in an internal medicine ward. Cardiovascular drugs (including heparin) usually followed antibiotics; overall, the range of MEs in cardiovascular drugs by nurses varied from 15.6% to 21.0%.
Table 5 summarizes detailed characteristics and findings of studies on most frequent drugs involved in MEs.
| Findings | Drugs | Type of Ward | Unit of Observation | Author(s) / Year | |
|---|---|---|---|---|---|
| NA | Ceftriaxone | Endocrinology & nephrology | Nursing students | Ebrahimi Rigi Tanha Z, et al. | 1 |
| 23.5% | Antimicrobials | Intensive Care Units (ICU) | IV administration by nurses | Vazin A, et al. | 2 |
| 62.0% | Albumin | Internal | IV administration by nurses | Sharifi N, et al. | 3 |
| 38.4% | Immunosuppressive | Nephrology | Patients | Vessal G. | 4 |
| 76.2% | Intravenous fluids | Pediatric | Pediatrics’ medical charts | Mohsenzade A, et al. | 5 |
| NA | Aspirin | Emergency | Nursing students | Mohammadnejad E, et al. | 6 |
| 27% | Antibiotics | ICU | Nurses | Nikpeyma N, et al. | 7 |
| 11.0% | Amikacin | ICU | IV administration by nurses | Fahimi F, et al. | 8 |
| 6.5% | Heparin | Internal | Nursing student | Baghcheghi N, et al. | 9 |
| NA | Heparin | CCU | Nursing student | Koohestani HR, et al. | 10 |
| 30% | Three NitroGlycerin | ICU | Infusion pump doses | Fahimi F, et al. | 11 |
Detailed characteristics of studies on most frequent drugs with ME and their findings
Discussion
This review intended to detect and evaluate the studies on source of MEs, reasons for MEs under-reporting, preventive measures of MEs and the most common drugs related to MEs in Iran. It demonstrates the existing gaps and evidence insufficiency in the current published literature which were investigated and the need for improvement in different aspects of study designs for future.
Sources of ME
Individual factors were the most frequently claimed source of ME occurrence reported in Iranian studies. This could be because MEs which are attributed to human failure are somewhat easier to recognize (3). But, in reality, they contribute to small percentage of MEs because system failures are the main cause in the vast majority of MEs (3, 4). Nursing students reported individuals as the main and only source of MEs occurrence with inadequate knowledge of medications, and miscalculations of doses as the most frequent factors. But based on nurses’ views, shortage of workforce, heavy workload, and physical and mental health problems were the main and most reported reasons. Illegible handwritings and inadequate knowledge of medications were recognized as the next most frequent sources of MEs. These differences between nursing students and nurses could be due to their personal skills and also institutional settings and responsibilities.
In different studies, dose miscalculation (8, 36-39) and inadequate knowledge of medication (1-3, 5, 8, 36, 37, 39, 40) were considered responsible for the most incidents of ME. These have been reported frequently in the literature as one of the most common contributing factors (2).
Nevertheless, it has been reported that nurses are at particular risk for making errors in calculating dosages because their mathematical skills are not well developed (8, 39, 41). Moreover, nurses routinely perform medication administrations; but, studies have revealed that they do not always have sufficient knowledge about the medication itself (1). Based on the systematic review by Alsulami et al., poor knowledge of prescribed or administered medications was the most common reported contributory factor for MEs in Middle Eastern countries (5).
As we stated in our results, shortage of workforce (8, 13, 39, 40, 42), heavy workload (2, 3, 39, 40, 42), poor physical or mental health (1, 40), are also common factors contributing to MEs in different studies and literature reviews. Shortage of workforce or increased workload can often lead to shifting highly-skilled staff from their standard actions (1). Staffing shortage also may cause an increase in administrative activities of nurses, which augments the chance of MEs (8, 39).
Illegibility of physician orders (3, 8, 39, 40) is a frequent causative factor to MEs and sometimes is accounted as the main factor (36). Nurses frequently administer medications in an unsafe manner due to poor standard of written prescriptions (39). Physicians have the least readable handwritings (8, 39) which place nurses at risk of making errors in administering medications (39).
These factors have not been assessed as frequent sources of ME in our included studies: inexperience (3, 5, 39, 40, 43), distraction (3, 8, 39, 40, 43) and interruption (1, 8, 36, 39) of nurses, and also medication characteristics such as similar names (3, 40) and large number of new drugs (3).
Reasons for MEs underreporting
Personal fears were the highest important reasons as the barrier for reporting in all of our studies. In the review by Aronson et al., personal fears have been stated as major perceived barriers (37).
Ignoring to report was the most frequent reason for underreporting (100% of the studies) in our review. It has been mentioned in other studies too with somehow similar phrases such as “error is not considered serious enough to report”, or “perception of non importance” (8, 43).
Several authors have stated that fear of being reprimanded and punishment is the most frequent barrier (2-4, 6, 8, 9, 38, 43); in our study, this became as the second most frequent barrier. There are many studies which emphasize on non-punitive (2, 6), blame free (3, 8, 38) and supportive (8) work environment for ME reporting; otherwise, health care’s providers will not report coverable errors (2). This emphasis has lead to the need for an anonymous reporting system which is usually lacking in developing countries including Iran.
MEs prevention strategies
Many preventive measures have been suggested in different overseas and Iranian studies like providing access to pharmacological text books (36, 38), defining protocols (44), formulary interchanges (42), launching electronic prescription systems (2, 6, 36, 37), medication labeling and packaging (2, 9, 37, 45), patient education about their treatment (4), physician education about appropriate guidelines for prescribing(46), providing information about new drugs (3, 36, 39) and compensating staff shortages (4). Some other approaches have also been declared to prevent MEs outside Iran such as avoidance of unsafe abbreviation (3, 37), national drug chart to reduce MEs related to documentation(3), national prescription forms (6), education of nurses in mathematics or calculation(3, 36), establishing formal ME reporting system (36, 38), supportive and non-punitive environment (3, 4), double checking (3), standardizing drug names(37), and checking five “right”s; right medication, patient, dose, route and time (3).
In the systematic review based on studies from Middle Eastern countries, two types of interventional study have been reported; intervention by clinical pharmacists and the use of computerized physician order entry systems with or without clinical decision support (5). Pharmacist participation in drug rounds is an effective intervention, which leads to significant reduction in MEs (2, 5, 38, 47).
CPOE and/or CDSS are among the possible promising technologies such as bar codes (45) and personal digital assistants (3) that are expected to have positive effects on ME reduction (2, 3, 5, 6, 36-38, 45, 48). But, only one interventional study in our review had assessed the impact of CPOE and/or CDSS establishment on reducing MEs. Although many advantages and disadvantages of CPOE/CDSS technologies have been reported by other authors (3, 6, 37, 38, 48) (2, 3, 45), there seems a need for further studies to assess the feasibility and possibility of implementation in Iranian context.
There is a huge lack of educational and interventional studies for preventing MEs. Considering the inability in generalization of this context based on its variation in different culture and countries, there is a need for these types of studies to evaluate different interventions in the Iranian context.
Most frequent drugs involved in MEs
We found much diversity in how studies reported most frequent drugs involved in MEs (3, 5, 38, 40, 48). The highest rate of MEs for administering intravenous fluids in a pediatric ward (76.2%) was much higher than study by Lewis et al. who reported the prevalence as 9% (48).In general, antibiotics were the most reported drugs involved in MEs in our studies; a finding which is in accordance with other reviews (3, 5, 38, 40, 48). The reported error rate for antibiotics by other studies was between 32% and 56% (40, 48); our studies reported a range between 11% and 56.4%. Cardiovascular drugs frequently followed antibiotics; other studies (5, 38, 40, 48) reported the same with the estimated prevalence of 16% to 17% (40, 48).
It is better to give the priority for further research to those drugs that carry more risk and are associated with more severe and frequent MEs.
Conclusion
Based on our results and discussion, we may suggest further study topics to bridge the gap in research on ME. These topics are:
Design, implementation, and evaluation of a systematic ME reporting system;
Assessing systems-related factors to ME alongside individual factors;
Assessing other stakeholders of MEs including health care professionals such as physicians, pharmacists, undergraduate students, etc.;
Evaluating the effectiveness of preventive measures for MEs in trials; and
Evaluating the effectiveness of interventional approaches which increase ME reporting by organizations and health care professionals.