Introduction
Development of diagnostic and therapeutic methods using laser and video techniques in the laryngeal region, as well as the location of laryngeal surgeries in the vicinity of the airway which make the patients being always threatened by risk of aspiration and adequacy of ventilation during the surgery, made sedation methods in managing anesthesia to b used for a long time (1). Considering the fact that the neural system in this area is highly sensitive and reactive and also important protective reflexes are active in the region, laryngeal surgeries are not performable with sedation alone and are associated with various autonomic and somatic reflexes (1). Combining local anesthesia and sedation which provides a painless condition without reflexes is definitely accompanied by maximum cooperation of the patients and a more practical situation to perform the surgeries (2). There are several methods of sedation (3-5); however, propofol results in rapid recovery (5) and no atmosphere pollution with anesthetic pollutants, the features which were considered from the beginning of its use in anesthesia. It has always been tried to reduce the adverse effects of propofol regimen by adding other drugs such as sedatives and narcotics (6-9) as much as possible. As the combinations of propofol-midazolam and propofol-fentanyl have never been compared in microlaryngeal surgeries, in this study we aimed to make a comparison between the two combinations regarding effectiveness, vital signs, hemodynamic, and providing a good condition for operation and recovery (10-12) by administering these combinations among the patients referred to Milad Hospital – Tehran during May 2007 and September 2008.
Experimental
In a sequential matched randomized double blind clinical trial, 40 patients with microlaryngeal surgery indications who were visited continually at the hospital were recruited and randomly allocated into two groups of 20 patients. After receiving informed written consent about the study protocol and sedation conditions and also informing the ear, nose and throat (ENT) surgeons of performing the operation under sedation, the patients were sent to the operating room. After performing the initial procedures and standard monitoring, the patients’ demographic data including age, sex, history of previous diseases, drug history, specific habits like smoking and alcohol and drug addiction was asked and documented in special forms. Only the patients without history of addiction, cardiovascular disease, hypertension, or drug dependency were included in the study. These patients were generally of ASA I-II groups and were candidates of microlaryngeal surgeries using suspension laryngoscopy. The operation was performed by Milad Hospital’s ENT surgery team. The surgeons and sign registrars were blinded to type of drug administered in addition to propofol for sedation. Propofol (Ferzinus Cabi Co.) was used for all the patients and they were randomly allocated into two groups of cases and controls. All the patients with a history of hypertension, diabetes, respiratory distress, hepatic and renal diseases were excluded. We also did not recruit patients with a history of drug allergy or drug addiction.
After catheter insertion, per each hour of fasting, 2 mL/Kg of normal saline was infused while no premedication for anesthesia was administered. The patients were fasting for the last 12 h before surgery and on the operation day, the surgery and sedation protocol were again fully described for the patient so that we could attract the trust and cooperation of the patients as much as possible. The equipments for anesthesia and intubation were checked after preparation, and resuscitation set was fully provided. For all the patients, from the time they entered the operating room, monitoring of heart rate, blood oxygen saturation and arterial blood pressure was performed through EKG and noninvasive methods and the values were recorded. Initial oxygenation was conducted via nasal cannula for at least 5 min to the level of 5 L/min while the surgeons were getting ready and a complete sedation was established. Anesthesia of the larynx was bilaterally conducted through superior laryngeal nerve block using 3 mL of 2% lidocaine solution. Success in creating the block was defined as a weak bass voice and reduced ability to cough effectively and voluntarily. In the next step, tans-tracheal block was done via cricothyroid membrane using 4 mL of the same concentration of lidocaine. Surface of the tongue was locally anesthetized up to the pharynx by means of 4 puff of 10% lidocaine spray. Performing these blocks, a complete attenuation of gag reflex and tolerance to laryngeal stimulation was largely obtained.
The first group, called midazolam group, first received 0.03 mg/Kg intravenous infusion of midazolam (Abureyhan co.), then 0.5 mg/Kg bolus dose of propofol followed by continuous infusion of 50 mcg/Kg/min of propofol. For the second group, called fentanyl group, at first 2 mcg/Kg fentanyl (Johnson & Johnson co.) was administered as a bolus, then after like the previous group 0.5 mg/Kg bolus dose of propofol followed by continuous infusion of 50 mcg/Kg/min of the drug was applied. After 6 min each patient was clinically assessed in terms of depth of sedation using Ramsay evaluation system (Table 1). The final goal was to achieve a sedation level of 3 or 4 according to Ramsay system. If a patient did not achieve the required level of sedation even after high doses of drugs, an extra dose of propofol was used as 0.1 mg/Kg bolus dose to obtain the desired level of Ramsay evaluation system.
| Sedation level | Characteristics |
|---|---|
| 1 | Patient is anxious and agitated or restless. |
| 2 | Patient is sleepy and partially co-operative; however is oriented to time and place. |
| 3 | Patient responds to commands. |
| 4 | Patient exhibits appropriate response to light glabellar tap and loud auditory stimulus |
| 5 | Patient exhibits no response to light glabellar tap or loud auditory stimulus |
After achieving the mentioned sedation level, vital signs including blood pressure, pulse rate and Spo2 level were recorded; the patients were evaluated again 1 min after insertion of laryngoscope. These vital signs and any adverse effect such as nausea/vomiting and chills was assessed and recorded in the patients up to full recovery. A full recovery was determined as the time the patient him/herself was able to open eyes and fully express his/her name. At this time the patient was asked to remember the intraoperative events and they were recorded in special forms. As the two groups were comparable regarding age and sex, the changes in blood pressure and heart rate as well as the time it took to achieve a full consciousness were analyzed by Mann-Whiteney u-test. Chi-square test was used for analysis of the need for additional dose of propofol, ability to recall, and occurrence of nausea/vomiting.
Results and Discussion
Twenty patients (16 men and 4 women) with mean age of 63 (range: 38-74) years were categorized in fentanyl-propofol group and another 20 subjects (17 women and 3 men) with mean age of 61 (range: 30-78) were recruited in midazolam-propofol group. In midazolam-propofol group, 6 patients needed an extra dose of propofol to achieve the desired level of sedation while in fentanyl-propofol group, 5 patients needed an additional dose. Mean preoperative systolic and diastolic blood pressure did not show statistically significant difference between the two groups (Table 2).
| Midazolam-propofol group (n = 20) | Fentanyl-propofol group (n = 20) | p-value | |
|---|---|---|---|
| Age (years) | 61 | 63 | NS* |
| Sex (male/female) | 17/3 | 16/4 | NS |
| Preoperative systolic blood pressure (mmHg) | 131.1 | 127.1 | NS |
| Preoperative oxygen saturation (%) | 95 | 96 | NS |
| Preoperative heart rate (per min) | 83 ± 8† | 85 ± 10 | NS |
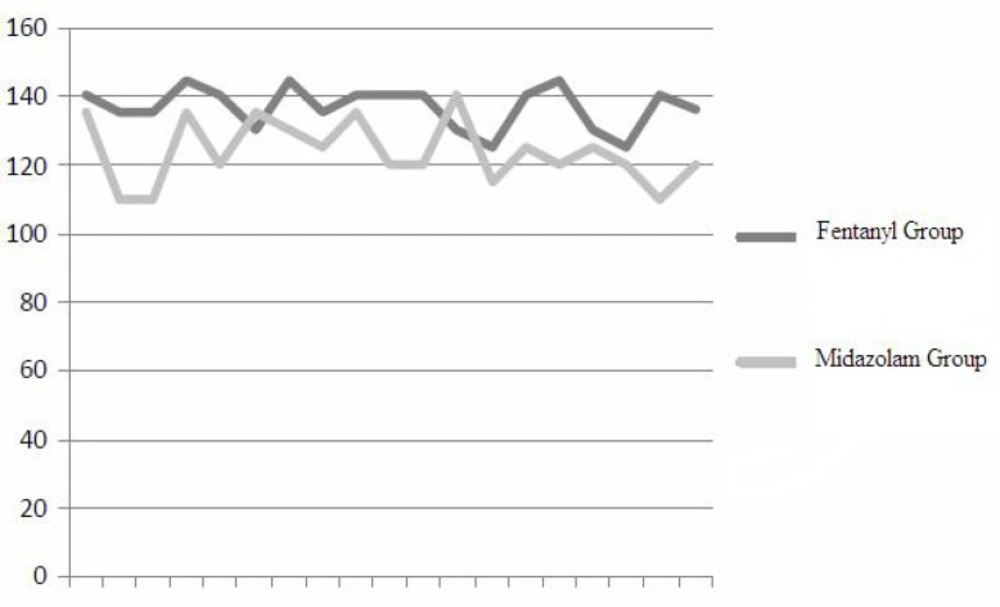
The changes in blood pressure during laryngoscopy did not show significant difference between the two groups; however, a significant increase in blood pressure during laryngoscopy was recorded in both groups. The decrease in systolic blood pressure 1 min after removal of the stimulation resulted by laryngoscopy was significantly more in midazolam group (36 ± 23 mmHg) compared with fentanyl group (25 ± 16 mmHg) (p < 0.01) (Figure 1, Table 3).
| Midazolam-propofol group (n = 20) | Fentanyl-propofol group | p-value | |
|---|---|---|---|
| Need for additional dose (yes/no) | 14/61 | 15/5 | NS* |
| Mean prelaryngoscopy systolic blood pressure | 121 | 117 | NS |
| Mean systolic blood pressure during laryngoscopy | 147.3 | 138.2 | NS |
| Mean systolic blood pressure 1 min after | 123.2 | 138.2 | 0.01 |
| removal of laryngoscopic stimulation | |||
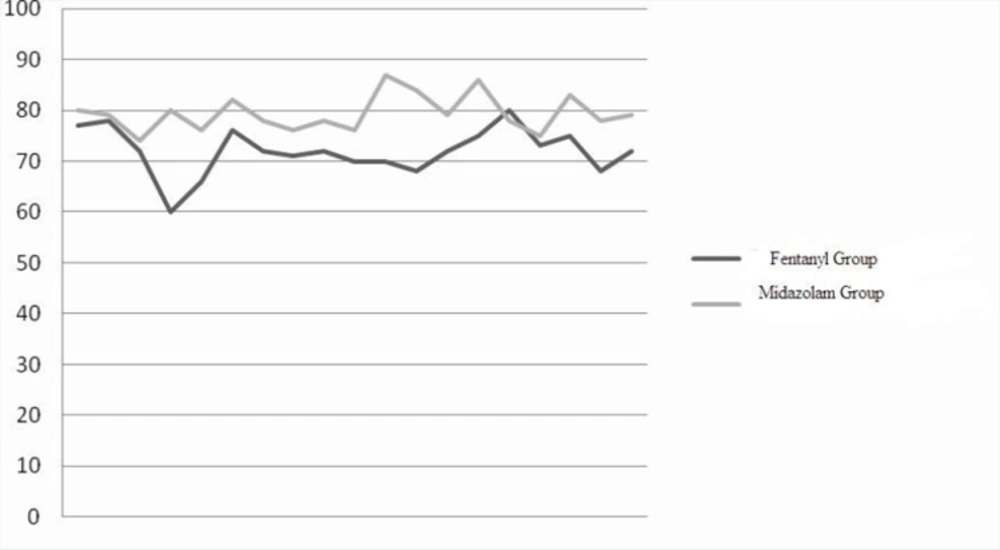
As is shown in Figure 2, the changes in mean heart rate during and after laryngoscopy, and during recovery was not significantly different between the two groups; however, the decrease in heart rate following fentanyl infusion was significantly more (70 ±14 in fentanyl group versus 80 ± 18 in midazolam group) (p < 0.02).
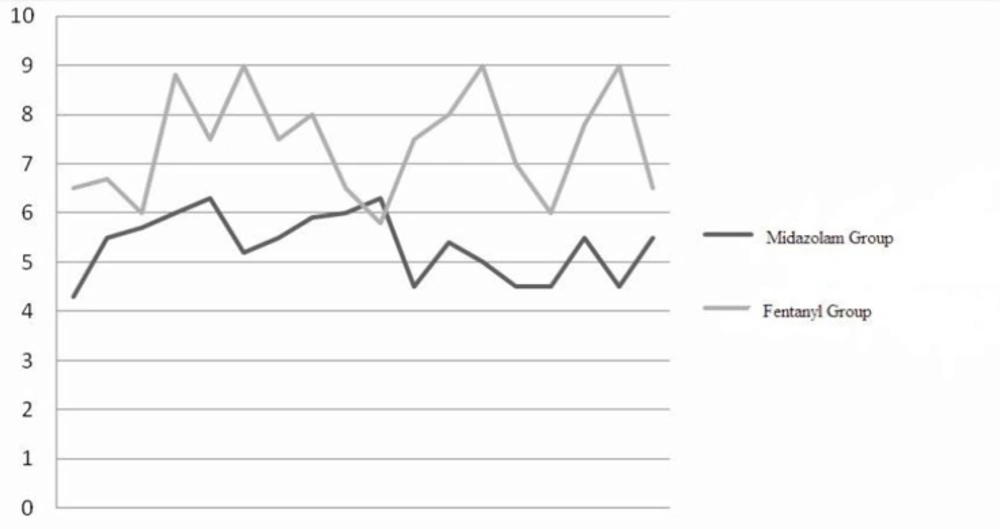
Mean prelaryngoscopy Spo2 was 93.4 ± 3.2 in fentanyl and 94.8 ± 2.4 in midazolam group which was not statistically different. Mean Spo2 during laryngoscopy was recorded as 92.4 ±1.1 in fentanyl and 94.6 ± 1.2 in midazolam group; the difference was statistically significant (p = 0.005). However, the mean Spo2 after laryngoscopy and during recovery time was not significant (Table 4). As expressed in Table 4, the mean time to voluntarily open eyes was 2.3 ± 2.3 min in midazolam and 3.7 ± 2.6 min in fentanyl group showing a significant difference (p = 0.05). The average time to achieve full consciousness in midazolam group was 5.7 ±1.7 min in midazolam group and 8.8 ± 1.1 min in fentanyl group which was also significantly different between the two groups (Figure 3).
Nausea/vomiting was observed in 2 (10%) patients in fentanyle group while postoperative chills was experienced by 3 patients in midazolam group (p > 0.05). Among the patients in midazolam group, 90% had no memory of the operation while 50% of patients in fentanyl group were able to recall the events during surgery (p < 0.001) (Table 4).
| Midazolam-propofol group (n = 20) | Fentanyl-propofol group (n = 20) | p-value | |
|---|---|---|---|
| Mean heart rate after induction | 82 ± 18 | 79 ± 14 | NS* |
| Mean Spo2 during laryngoscopy | 94.6 ± 1/2 | 92.4 ± 1/1 | < 0.005 |
| Time to achieve full consciousness (min) | 5.7 ± 1.7 | 8.8 ± 1.1 | < 0.001 |
| Nausea/vomiting (yes/no) | 29/0 | 18/2 | NS* |
| Intraoperative amnesia (yes/no) | 90/10 | 50/50 | < 0.001 |
This study demonstrated that the need to additional dose of propofol was almost similar in both groups. The changes in systolic blood pressure following surgical stimulation and before initiation of the surgery were not wide following administration of both regimens, suggesting that both approaches are effective in controlling and preventing the changes in blood pressure; the mean systolic blood pressure at the time of surgical stimulation was 147 mmHg in midazolam group and 138 mmHg in fentanyl group. The increase in blood pessure after surgical stimulation was similar and comparable in both groups; however, the patients in the two groups were different based on the time of achieving the blood pressure before stimulation; patients receiving midazolam achieved the pre-stimulation blood pressure more rapidly which could be mentioned as an advantage of midazolam-propofol regimen. A more rapid reduction in heart rate was observed in the propofol-fentanyl group justifiable by opiod nature of fentanyl; as a result, fentanyl is more beneficial when operating patients with heart failure or myocardial ischmia. However, as the changes in heart rate during laryngoscopy was similar in both regimens it might be necessary to add some other drugs such as β-blockers to control heart rate when these regimens are used. Compared to midazolam, after removal of laryngoscopic stimulation, fentanyl decreases heart rate upto the baseline more rapidly. Considering the changes in arterial blood oxygen saturation during laryngoscopy, Spo2 reduction was more significant in fentanyl group probably caused by respiratory depression due to opioid nature of fentanyl; however, patients in midazolam group also experienced the reduction in Spo2. Other advantages of midazolam are a more rapid recovery and a higher level of amnesia during surgery which makes it a good sedative drug in outpatient surgeries with sedation when added to propofol. These kinds of surgeries are associated with severe stimulations during operation leaving various psychologic and panic effects if the patient remembers them. Besides, a more rapid recovery results in a more suitable outpatient surgery and makes maintaining and cleaning of the patient’s airway more appropriate after sugery. There were some cases of nausea/vomitting in the fentanyl group which might be due to the opioid nature of the drug. Although propofol can control postoperative nausea/vomitting in most of the patients, these adverse effects may manifest when using opioids. In the present study, there were two cases of postoperative nausea/vomotting in patients undergoing laryngeal anesthesia and sedation which is potentially considered as an adverse effect (4).
Although fentanyl is expected to control blood pressure, the question is that why the changes in blood pressure following laryngoscopy and its reduction to pre-stimulation level was more rapid in midazolam group. Sedative and amnetic effects of midazolam enable it to suppress the stress during the operation; as a result, blood pressure reduction to the baseline is more repid after removal of stimulation (7). There are different methods such as those with or without intubation like jet ventilation or insufflations in order to induce general anesthesia in patients undergoing direct laryngoscopy; however, it seems that sedation with local anesthesia can provide an appropriate condition in surgeries with short duration, especially outpatient surgeries, preventing adverse effects such as aspiration of gastric contents or entrance of debri and blood resulted from the surgery into the airway (2). Consciousness in these patients, in addition to getting their cooperation to establish a good condition for operation, can provide a wider breadth of vision in the laryngeal area and is associated with the presence of the tube in the larynx, restriction on the use of laser, and operation room contamination to anesthetic gases. Propofol can be the first choice in managing these patients as it reduces environmental pollution, provides a faster recovery, and decreases adverse effects such as nausea/vomiting (4); however, using propofol alone is associated with several risks including respiratory depression and suppression of laryngeal reflexes. Several combinations have been used with propofol to reduce its adverse effects but there are few studies on use of these propofol combinations in laryngeal surgeries (8, 9). Propofol in combination with fentanyl and midazolam is used in various therapeutic regimens and has always shown good hemodynamic status in the studies. The patient is significantly less cooperative when propofol is used alone for sedation, and even more, patient irritability and airway spasm is seen when low doses of this drug is administered. Rapid return of laryngeal reflexes after laryngeal surgeries prevents blood and debris resulted from surgery to enter the trachea (12). Tagaitoy et al reported a more rapid return of protective reflexes in propofol-fentanyl regimen compared with propofol alone (5). In another study, consumption of propofol for induction of sedation was reduced upto 52% compared with when propofol alone was used (10). Another study considered better maintenance of hemodynamic in a group of patients using propofol-midazolam in comparison with a group using propofol only. In our study, in 70-75% of patients, the administered dose of propofol along with its co-administered drug seemed to be enough to achieve a desired level of sedation. The changes in blood pressure before and during laryngoscopy were in both groups in an acceptable range, however, in midazolam-propofol group blood pressure returned to the baseline pressure much faster (8).
The combination of fentanyl and propofol was more efficient in reducing heart rate before laryngoscopy; this is previously confirmed by other studies (1, 9, 12). Inducing parasympathomimetic effect due to fentanyl, this combination was successful in reducing heart rate after infusion and also after removal of stimulation. Midazolam provided better ventilation maintenance compared with fentanyl which showed the superiority of fentanyl in oxygenation. In cases with partial airway obstruction, ventilation suppression is a common and potentially dangerous status; hence, this is of advantages of using midazolam in combination with propofol in these patients. Some previous studies have considered propofol-fentanyl combination in preventing laryngeal spasm (5); however, the effect of fentanyl in suppressing ventilation can limit its use.
A more rapid awakening time, as well as no recall of unpleasant memories make midazolam beneficial in outpatients and those undergoing surgeries needing sedation.
In a study by Rama-Maceiras et al it was confirmed that the combination of propofol and opioids induces nausea/vomiting (11). In this study fentanyl-propofol regimen was associated with a more risk of nausea as well.
Although both methods provide a good sedative and anesthetic cover for microlaryngeal surgeries, however, shorter recovery duration, less postoperative amnetic effect and establishing a more adequate intraoperative oxygenation make midazolam-propofol combination generally superior. Providing a better condition, this pharmaceutic group is a better choice for these kinds of surgeries. In the future, important pharmaceutic compounds or even new anesthetic drugs may replace this proposed alternative and then they may resolve the possible objections of this regimen. In spite of limited number of patients in our study, conducting such a study in a group of patients with similar socioeconomic status, in the same hospital with the same equipments and the same drugs make our study valuable in managing anesthesia in these types of patients. More studies following emergence of appropriate treatment regimens applicable for all laryngeal surgeries which provide maximum health can be in prospective.