1. Background
Noncommunicable diseases (NCDs) are becoming increasingly prevalent among Iranian people and other populations worldwide (1-3). Simultaneously, the prevalence of multimorbidity (MM), described as presenting two or more chronic conditions (4), is also increasing (5). As multimorbid individuals generally deal with complicated medical demands and experience adverse clinical outcomes (6, 7), such as increased death rate, disability, reduced life quality, and adverse drug reactions or events (8, 9), MM has been one of the most critical issues for healthcare systems. Moreover, the patients have to cope with the growing number of drugs they need to use for their treatment.
In addition to financial impacts, polypharmacy has some medically negative impacts, including a higher risk of using potentially inappropriate medications (PIMs) (10), drug-drug interactions (DDIs) (3), under-using appropriate drugs, poor patient compliance, dropped functioning (11), and reduced physical performance (12). Another negative impact associated with polypharmacy is adverse drug events (ADEs) (13), resulting in hospitalizations. Adverse drug events can be predicted based on defined pharmacological information of prescribed medications, such as interactions, and thus are preventable in 59 - 70% of cases (14). Moreover, hospital readmissions with short intervals (15) and an increased death rate are other negative consequences of polypharmacy (14). Accordingly, all the mentioned factors make polypharmacy a challenging issue for public health and affected people.
There is no common consensus on the cut-off point for interpreting polypharmacy. As a result, the prevalence of polypharmacy has a broad range due to the lack of a universal definition. According to a study by Forslund et al., 24.1% of the Swedish population had polypharmacy (using more than five prescription medicines) (10). According to Pappa et al.’s study on a Greek population, 45.6% of those meeting the polypharmacy criteria were under 65-years-old (13). It has been indicated that polypharmacy is associated with different factors, including older age (11), education (9), gender (12), socioeconomic status (9), poor self-rated health (SRH) (14), chronic diseases (CDs) or MM (11), obesity (15), and smoking (15), among other factors. These factors have been well investigated among older adults.
To the best of our knowledge, studies examining the prevalence of polypharmacy in general populations (aged 35 - 70 years) are rare, with most studies focusing on the elderly. On the other hand, because CDs occur 10 - 15 years earlier in individuals living in developing countries (16), polypharmacy in young people is becoming a serious public health issue. Accordingly, it is critical to investigate the epidemiology of polypharmacy and its related factors in middle-aged people as a prerequisite for developing approaches to rationalize polypharmacy and prevent possible adverse impacts in general practice. Therefore, we decided to investigate the prevalence of polypharmacy and its predicting risk factors in the Azar cohort population.
2. Methods
This cross-sectional population-based cohort study utilized Azar cohort information to investigate polypharmacy in the Azar cohort population (N = 15,001). The Azar cohort is considered a prospective cohort study performed in the city of Shabestar, East Azarbaijan province, Iran. This research is part of a large-scale Persian cohort study (Prospective Epidemiological Research Studies in Iran) (17). The pilot and enrollment phases were launched in 2014, and the study was concluded in 2017. All eligible individuals aged 35 - 70 years in the Shabestar region were invited to participate in the study. Those included had been the inhabitants of Shabester for at least nine months. The participants with severe psychiatric or physical illnesses and pregnant women were excluded from the study. The Azar cohort study is described further in the cohort profile article (18). The Tabriz University of Medical Sciences Ethics Committee approved this work (tbzmed.rec.1393.205). All subjects provided written informed consent.
2.1. Participants' Demographic Characteristics
An available and well-designed questionnaire was used to obtain the participants' demographic information, such as age, sex, marital status, and educational background. Personal behaviors like smoking were assessed using the questionnaire. The smoking status was reported as either continuous smoker or non-smoker. The wealth score index (WSI), determined via multiple correspondence analysis (MCA), was used to assess the socioeconomic position of the participants. Each participant's WSI was calculated using their possession of a range of durable assets (for example, dishwasher, car, and TV), house condition (e.g., the number of rooms, type of ownership), and education level.
Attendees in the research were divided into five WSI quintiles, ranging from the lowest to the highest (first to fifth quintiles, respectively). The participants’ daily activity was measured in the study through a questionnaire completed by the subjects. A criterion known as metabolic equivalent of task (MET) was used for this purpose. Each MET represents the amount of energy consumed by each individual concerning their weight. For example, one MET is the amount of oxygen consumed per kilogram of body weight per minute by each resting individual, which is 3.5 mL of oxygen, and four METs are equal to 16 milliliters of oxygen used per kilogram of body weight per minute. Using MET, we measured the activity levels of each participant.
2.2. Polypharmacy Definition
There is no general agreement on defining polypharmacy, although the most often used definition is a daily intake of five or more medicines for a minimum of 90 days or more (12). This study collected the number of drugs consumed and declared by each subject during the interview, including prescribed drugs, over-the-counter (OTC) drugs, and dietary or herbal products. We divided medicines into 22 categories.
2.3. Definition of Multimorbidity
Multimorbidity (MM) is characterized by the presence of two or more chronic diseases (CDs) simultaneously, such as cardiovascular diseases (CVD), hypertension, diabetes mellitus, depression, cerebrovascular diseases, asthma, obesity, fatty liver disease, rheumatologic diseases, and different cancers (e.g., gastrointestinal, prostate, skin, bladder, lung, breast, head and neck, etc.). Participants were deemed to have these disorders in the questionnaires if they answered “yes” to the related question, "Has any doctor ever informed you that you have …?" Obesity was also classified as having a body mass index of 30 kg/m2 or greater. In addition to the chronic diseases listed above that were used in the MM classification, chronic headache and thyroid disease were described independently as CDs in this study.
2.4. Anthropometric and Blood Pressure Measurements
All individuals' weights and heights were assessed, and then the data were applied to calculate the body mass index (BMI) using the standard formula: weight (kg)/height (m2). The detailed anthropometric measurements can be found elsewhere (17). Based on the BMI, the subjects were classified into four different categories: (1) underweight (BMI < 18.5 kg/m2), (2) normal weight (BMI: 18.5 - 24.9 kg/m2), (3) overweight (BMI: 25.0 - 29.9 kg/m2), and (4) obese (BMI ≥ 30 kg/m2). The underweight participants were excluded (91 participants).
To measure blood pressure, a skilled nurse used a mercury sphygmomanometer (Rudolf Richter; DE-72417; Germany) to check blood pressure two consecutive times with an interval of two minutes, twice for each arm, in a sitting position after 10 minutes of rest. The systolic and diastolic blood pressures were calculated by taking the averages of these two measurements.
2.5. Statistical Analysis
Descriptive statistics, including frequency, percentages, mean, and standard deviation (SD), were reported for all variables of concern. The subjects were classified based on the number of drugs they used. The chi-square and Kruskal-Wallis tests were used appropriately to examine the general characteristics across the features of the determined categories. Furthermore, ordinal logistic regression was conducted to analyze the polypharmacy predicting risk factors (Model 1: Unadjusted, Model 2: Adjusted for age, gender, education level, and socioeconomic status, [WSI]). The odds ratios (ORs) and the related confidence intervals (CIs) of 95% were evaluated. The statistical significance level was set at P < 0.05. Finally, SPSS software was used to analyze the data (SPSS Inc., Chicago, IL, version 20).
3. Results
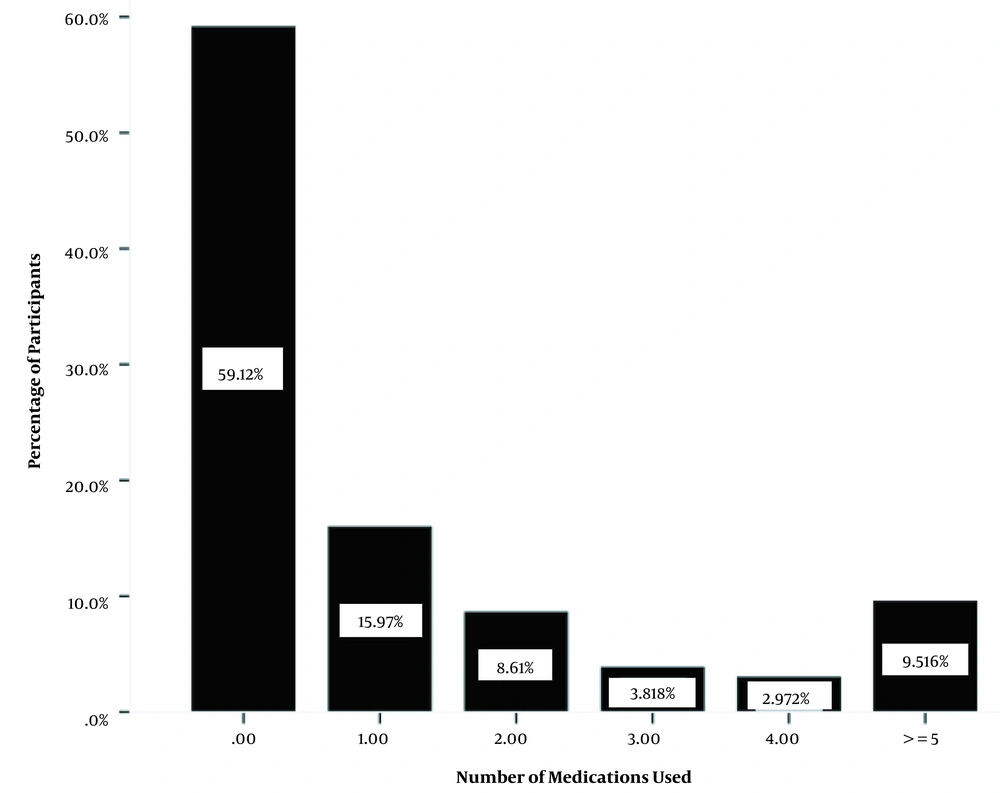
Based on Figure 1, 9.51% of the population received five or more claimed prescribed medications. Table 1 displays the overall characteristics and MM of all 14,910 individuals stratified by polypharmacy status. The polypharmacy group (≥ 5 medicines) had a greater proportion of female, less educated, non-smoking, and married participants. Furthermore, the number of medications rose with age and BMI. On the other hand, when the level of physical activity increased, the number of medicines dropped. Hypertension, obesity, depression, diabetes mellitus, cardiovascular diseases, thyroid disorders, chronic headache, COPD rheumatologic diseases, fatty liver, stroke, and different types of cancers were the top 12 conditions associated significantly with polypharmacy. The participants with hypertension consumed more medicines than the ones without this condition.
| Number of Medicines | P Value | ||||||
|---|---|---|---|---|---|---|---|
| 0 (n = 8812) | 1 (n = 2379) | 2 (n = 1283) | 3 (n = 572) | 4 (n = 446) | 5 (n = 1418) | ||
| Gender | < 0.001* | ||||||
| Male | 4628 (52.5) | 803 (33.8) | 319 (24.9) | 103 (18) | 200 (44.8) | 592 (41.7) | |
| Female | 4184 (47.5) A | 1576 (66.2) A | 964 (75.1) A | 469 (82) A | 246 (55.2) B | 826 (58.3) A | |
| Age (y) | < 0.001** | ||||||
| 35 - 49 | 5465 (62) C | 1185 (49.8) C | 576 (44.9) C | 225 (39.3) C | 132 (29.6) C | 216 (15.2) C | |
| 50 - 59 | 2358 (26.8) C | 750 (31.5) C | 451 (35.2) C | 202 (35.3) C | 163 (36.5) C | 583 (41.1) C | |
| 60 - 70 | 989 (11.2) C | 444 (18.7) C | 256 (20) C | 145 (25.3) C | 151 (33.9) C | 619 (43.7) C | |
| Residential regions | 0.2* | ||||||
| Urban residents | 6166 (70) | 1658 (69.7) | 883 (68.8) | 376 (65.7) | 296 (66.4) | 989 (69.7) | |
| Rural residents | 2646 (30) | 721 (30.3) | 400 (31.2) | 196 (34.3) | 150 (33.6) | 429 (30.3) | |
| Marital status | < 0.001* | ||||||
| Not married | 510 (5.8) | 170 (7.1) | 117 (9.1) | 69 (12.1) | 42 (9.4) | 176 (12.4) | |
| Married | 8301 (94.2) D | 2208 (92.9) D | 1166 (90.9) E | 503 (87.9) E | 403 (90.6) F | 1241 (87.6) E | |
| Education level | < 0.001** | ||||||
| Illiterate | 1123 (12.7) G | 420 (17.7) G | 269 (21) G | 141 (24.7) H | 110 (24.7) G | 422 (29.8) I | |
| Primary school | 3542 (40.2) | 918 (38.6) | 504 (39.3) | 223 (39.1) | 167 (37.4) | 465 (32.8) I | |
| Diploma | 3322 (37.7) G | 830 (34.9) G | 393 (30.7) G | 172 (30.1) H | 138 (30.9) G | 425 (30) I | |
| University | 824 (9.4) | 208 (8.8) | 115 (9) | 35 (6.1) H | 31 (7) | 104 (7.3) I | |
| BMI (kg/m2) | < 0.001** | ||||||
| 18.5 - 24.9 normal weight | 2129 (24.2) J | 402 (16.9) J | 218 (17) J | 89 (15.6) J | 76 (17) K | 202 (14.2) J | |
| 25 - 29.9 over weight | 3720 (42.2) J | 1010 (42.5) J | 479 (37.3) J | 224 (39.2) J | 185 (41.5) | 530 (27.4) J | |
| ≥ 30 obese | 2963 (33.6) J | 967 (40.6) J | 586 (45.7) J | 259 (45.3) J | 185 (41.5) K | 686 (48.4) J | |
| Physical activity level (METs) | < 0.001** | ||||||
| Low | 2541 (28.8) L | 808 (34) L | 492 (38.3) L | 253 (44.2) L | 194 (43.5) | 713 (50.3) M | |
| Moderate | 2736 (31) L | 939 (39.5) L | 513 (40) L | 204 (355.7) L | 131 (29.4) L | 432 (30.5) | |
| High | 3535 (40.1) L | 632 (26.6) L | 278 (21.7) L | 115 (20.1) L | 121 (27.1) L | 273 (19.3) M | |
| Quintiles of wealth index | < 0.001** | ||||||
| 1 (poorest) | 1999 (22.7) | 522 (21.9) | 297 (23.1) | 171 (29.9) N | 93 (20.9) | 369 (26) P | |
| 2 | 1397 (15.9) | 421 (17.7) | 216 (16.8) | 88 (15.4) | 95 (21.3) | 295 (20.8) P | |
| 3 | 1808 (20.5) | 457 (19.2) | 263 (20.5) | 111 (19.4) | 88 (19.7) | 307 (21.7) | |
| 4 | 1950 (22.1) | 499 (21) | 258 (20.1) | 119 (20.8) | 88 (19.7) | 197 (13.9) P | |
| 5 (richest) | 1658 (18.8) | 480 (20.2) | 249 (19.4) | 83 (14.5) N | 82 (18.4) | 250 (17.6) | |
| Current smoking status | < 0.001* | ||||||
| Smoker | 1278 (14.5) | 202 (8.5) | 84 (6.5) | 27 (4.7) | 65 (14.6) | 142 (10) | |
| Non-smoker | 7534 (85.5) Q | 2177 (91.5) Q | 1199 (93.5) Q | 545 (95.3) Q | 381 (85.4) | 1276 (90) Q | |
| Multimorbidity | < 0.001* | ||||||
| 0 | 4751 (53.9) R | 590 (24.8) R | 229 (17.8) R | 85 (14.9) R | 97 (21.7) S | 49 (3.5) R | |
| 1 | 2994 (34) R | 940 (39.5) R | 388 (30.2) R | 147 (25.7) R | 142 (31.8) | 289 (20.4) R | |
| 2 | 846 (9.6) R | 604 (25.4) R | 357 (27.8) R | 190 (33.2) R | 100 (22.4) S | 442 (31.2) R | |
| 3 | 182 (2.1) R | 202 (8.5) R | 224 (17.5) R | 91 (15.9) R | 72 (16.1) S | 380 (26.8) R | |
| ≥ 4 | 39 (0.4) R | 43 (1.8) R | 85 (6.6) R | 59 (10.3) R | 35 (7.8) S | 258 (18.2) R | |
| Common chronic diseases | |||||||
| Hypertension | 514 (5.8) | 685 (29.2) | 474 (36.9) | 239 (41.8) | 154 (34.5) | 957 (67.5) | < 0.001 T |
| Diabetes | 261 (3) | 389 (16.4) | 337 (26.3) | 142 (24.8) | 84 (18.8) | 529 (37.3) | < 0.001 T |
| CVD | 96 (1.1) | 60 (2.5) | 45 (3.5) | 35 (6.1) | 46 (10.3) | 452 (31.9) | < 0.001 T |
| Obesity | 2960 (33.6) | 967 (40.6) | 568 (45.7) | 259 (45.3) | 184 (41.3) | 685 (48.3) | < 0.001 T |
| Stroke | 17 (0.2) | 9 (0.4) | 18 (1.4) W | 9 (1.6) W | 6 (1.3) W | 57 (4) W | < 0.001* |
| Fatty liver | 282 (3.2) | 127 (5.3) | 113 (8.8) | 58 (10.1) | 33 (7.4) | 121 (8.5) | < 0.001 T |
| Rheumatoid | 188 (2.1) | 76 (3.2) | 54 (4.2) | 39 (6.8) | 28 (6.3) | 126 (8.9) | < 0.001 T |
| Cancers | 26 (0.3) | 16 (0.7) Y | 13 (1) Y | 5 (0.9) | 13 (2.9) Y | 11 (0.8) Y | < 0.001 * |
| Depression | 862 (9.8) | 506 (21.3) | 430 (33.5) | 220 (38.5) | 130 (29.1) | 401 (28.3) | < 0.001 T |
| COPD | 192 (2.2) | 90 (3.8) | 68 (5.3) | 46 (8) | 37 (8.3) | 101 (7.1) | < 0.001 T |
| Thyroid disorder | 428 (4.9) | 313 (13.2) | 228 (17.8) | 104 (18.2) | 51 (11.4) | 180 (12.7) | < 0.001 T |
| Chronic headache | 866 (9.8) | 361 (15.2) | 233 (18.2) | 135 (23.6) | 70 (15.7) | 217 (15.3) | < 0.001 T |
Abbreviation: METs, metabolic equivalent of task.
* P: chi-square test (total P value for comparison); ** P: Kruskal-Wallis H (total P value for comparison).
B, P = 0.01 compared to the male group; C, comparisons significant (P < 0.001) among all age groups; D, P = 0.04 compared to not married; E, P < 0.001 compared to not married; F, P = 0.01 compared to not married; G, comparisons significant (P < 0.001) between illiterate and diploma groups; H, comparisons significant (P < 0.001) among illiterate, diploma, and college groups; I, comparisons significant (P < 0.001) among all education levels; J, comparisons significant (P < 0.001) among all BMI classes; K, comparisons significant (P < 0.001) between underweight and obese groups; L, comparisons significant (P < 0.001) among all physical activity levels; M, comparisons significant (P < 0.001) between low and high physical activity levels; N, comparisons significant (P = 0.005) between the first and fifth quintiles of WSI; P, comparisons significant (P < 0.001) among the first, second, and fourth quintiles of WSI; Q, P < 0.0001 compared to the smoker group; R, comparisons significant (P < 0.001) among all multimorbidity classification with each other; S, comparison significant (P < 0.001) among 0,2,3, and 4 multimorbidity classification; T, comparisons significant (P < 0.01) among all polypharmacy classes; W, comparisons significant (P < 0.01) among all polypharmacy classes, except for the second class; Y, comparisons significant (P < 0.05) among all polypharmacy classes, except for the no medicine group.
As shown in Table 2, the most often prescribed drugs in the research population were those prescribed to treat disorders related to the cardiovascular system (19.9%), central nervous system (CNS) (16.7%), endocrine system (13.3%), analgesics and NSAIDs (11.5%), and drugs used to treat musculoskeletal and joint diseases (11.4%). Furthermore, 3.8% of individuals consumed calcium and vitamin D supplements. We also discovered that the patterns of medicines and most diseases varied substantially across genders (P < 0.05).
| Medicine Group | Male | Female | P Value b | Total |
|---|---|---|---|---|
| Cardiovascular drugs | 1008 (15.2) | 1954 (23.6) | < 0.001 | 2962 (19.9) |
| CNS drugs | 976 (14.7) | 1513 (18.3) | < 0.001 | 2489 (16.7) |
| Drugs used in endocrine disorders and contraceptives | 631 (9.5) | 1355 (16.4) | < 0.001 | 1986 (13.3) |
| Analgesics and NSAIDs | 796 (12) | 923 (11.2) | 0.07 | 1719 (11.5) |
| Drugs used in musculoskeletal and joint diseases | 781 (11.8) | 926 (11.2) | 0.3 | 1707 (11.4) |
| Calcium | 44 (0.7) | 523 (6.3) | < 0.001 | 567 (3.8) |
| Iron supplement | 20 (0.3) | 523 (6.3) | < 0.001 | 543 (3.6) |
| Zinc supplement | 102 (1.5) | 322 (3.9) | < 0.001 | 424 (2.8) |
| Hypertension | 986 (14.8) | 2047 (24.7) | < 0.001 | 3033 (20.3) |
| Diabetes | 688 (10.3) | 1054 (12.8) | < 0.001 | 1742 (11.7) |
| CVD | 391 (5.9) | 343 (4.2) | < 0.001 | 734 (4.9) |
| Obesity | 1741 (26.2) | 3900 (47.2) | < 0.001 | 5641 (37.6) |
| Stroke | 54 (0.8) | 62 (0.8) | 0.36 | 116 (0.8) |
| Fatty liver | 266 (4) | 468 (5.6) | < 0.001 | 734 (4.9) |
| Rheumatoid | 123 (1.9) | 388 (4.7) | < 0.001 | 511 (3.4) |
| Cancers | 24 (0.4) | 60 (0.7) | 0.003 | 84 (0.6) |
| Depression | 530 (8) | 2019 (24.4) | < 0.001 | 2549 (17.1) |
| COPD | 188 (2.8) | 346 (4.2) | < 0.001 | 534 (3.6) |
| Thyroid disorder | 134 (2) | 1170 (14.2) | < 0.001 | 1304 (8.7) |
| Chronic headache | 478 (7.2) | 1404 (17) | < 0.001 | 1882 (12.6) |
aValues are expressed as No. (%).
bP chi-square test
Cardiovascular medications, CNS drugs, endocrine disorder medicines, and contraceptives were more prevalent than other drug categories in females. The CDs of men and women are compared in Table 2. Except for CVD, females showed a greater prevalence of CDs than males. Obesity was also more common among women.
Table 3 shows the results of ordinal logistic regression analysis of variables associated with polypharmacy in the Azar cohort group. The subjects aged 60 - 70 years had substantially greater odds of polypharmacy [OR = 4.53; 95% CI: 4.16 - 4.94] than those aged 35 - 49 years.
| Unadjusted OR (95%CI) | P Value | Adjusted a OR (95%CI) | P Value | |
|---|---|---|---|---|
| Age (y) | ||||
| 35 - 49 | Reference | - | ||
| 50 - 59 | 2.31 (2.15 - 2.49) | < 0.001 | - | |
| 60 - 70 | 4.53 (4.16 - 4.94) | < 0.001 | - | |
| Gender | - | |||
| Male | Reference | - | ||
| Female | 2.04 (1.91 - 2.18) | < 0.001 | - | |
| Residential regions | ||||
| Urban residents | 0.94 (0.88 - 1.01) | 0.12 | 1.00 (0.93 - 1.08) | 0.81 |
| Rural residents | Reference | |||
| Marital status | ||||
| Not married | 1.78 (1.59 - 2.00) | < 0.001 | 1.06 (0.94 - 1.20) | 0.32 |
| Married | Reference | |||
| Education level | ||||
| Illiterate | 2.14 (1.88 - 2.44) | < 0.001 | - | |
| Primary school | 1.08 (0.95 - 1.21) | 0.20 | - | |
| Diploma | 0.99 (0.88 - 1.12) | 0.90 | - | |
| University | Reference | - | ||
| Quintiles of wealth index | ||||
| 1 (poorest) | 1.10 (0.99 - 1.21) | 0.05 | - | |
| 2 | 1.2 (1.08 - 1.32) | 0.001 | - | |
| 3 | 1.02 (0.92 - 1.12) | 0.68 | - | |
| 4 | 0.85 (0.77 - 0.94) | 0.003 | - | |
| 5 (richest) | Reference | |||
| Physical activity level (METs) | ||||
| Low | 2.52 (2.32 - 2.73) | < 0.001 | 1.90 (1.74 - 2.07) | < 0.001 |
| Moderate | 1.92 (1.77 - 2.08) | < 0.001 | 1.47 (1.34 - 1.60) | < 0.001 |
| High | Reference | |||
| Current smoking status | ||||
| No smoker | 1.74 (1.57 - 1.94) | < 0.001 | 1.02 (0.90 - 1.15) | 0.4 |
| smoker | Reference | |||
| Multimorbidity | ||||
| 0 | Reference | |||
| 1 | 2.90 (2.66 - 3.17) | < 0.001 | 2.73 (2.49 - 2.98) | < 0.001 |
| 2 | 9.15 (8.3 - 10.10) | < 0.001) | 7.56 (6.83 - 8.37) | < 0.001 |
| 3 | 22.88 (20.15 - 25.99) | < 0.001 | 17.34 (15.21 - 19.76) | < 0.001 |
| ≥ 4 | 49.36 (41.32 - 58.95) | < 0.001 | 33.87 (29.85 - 43.10) | < 0.001 |
| BMI classification (kg/m2) | ||||
| 18.5 - 24.9 normal weight | Reference | |||
| 25 - 29.9 over weight | 1.38 (1.26 - 1.51) | < 0.001 | 1.31 (1.20 - 1.44) | < 0.001 |
| ≥ 30 obese | 1.94 (1.77 - 2.12) | < 0.001 | 1.65 (1.50 - 1.82) | < 0.001 |
Abbreviation: METs, Metabolic equivalent of task.
aAdjusted for age, gender, education level, and socioeconomic status.
Different factors can influence the risk of polypharmacy. For example, our results revealed that being a female [OR = 2.04; 95% CI: 1.91 - 2.18], illiterate [OR = 2.14; 95% CI: 1.88 - 2.44], and not married [OR = 1.78; 95%CI: 1.59 - 2.00] increased the chance of polypharmacy significantly (Table 3). The participants in the lowest physical activity tertile [OR = 2.52; 95 % CI: 2.32 - 2.73] had a greater risk of polypharmacy than those who had the highest level of physical activity (Table 3). This correlation remained substantial after controlling for age, sex, education level, and WSI. Obese participants revealed a trend towards more prescribed medications.
Moreover, this group revealed a 1.94 increase [95% CI: 1.77 - 2.12] in polypharmacy risk compared to the participants with normal weight. As the co-occurrence of chronic diseases increased, the risk of polypharmacy increased. Our results indicated that the risk of polypharmacy was 49.36 times higher in patients with four or more CDs than in those without CDs. However, the reported relationship was reduced after adjusting for age, sex, education level, and WSI [OR = 33.87; 95% CI: 29.85 - 43.10].
4. Discussion
In the present research, we investigated the occurrence of polypharmacy and associated risk factors in the Azar cohort population. This report also focused on gender differences. In this cohort study, we identified 9.51% of participants who had polypharmacy. According to a study, 9% of African-American individuals had polypharmacy (consuming more than five medicines) (19). Another study found that polypharmacy was prevalent in 26% of American individuals older than 21 years (20). Furthermore, Seixas and Freitas revealed that 13.5% of the Brazilian population aged 50 or older were exposed to polypharmacy (21). More recently, an investigation in Qatar on 5,639 older individuals indicated that 75% of them were subject to polypharmacy (22).
Among older people, the prevalence of polypharmacy ranges from 5% to 78% (23). The difference in results might be due to variations in polypharmacy classifications, age, inpatients, or outpatients. Most of the trials were conducted on older people; however, some research assessed polypharmacy in participants younger than 60.
Females’ gender was a risk factor for polypharmacy, with substantial variations in the incidence of the most often prescribed medications detected between males and females. This conclusion aligns with that of earlier research that found females at a higher risk of polypharmacy (19, 24, 25). Females report more CDs than males (26). Women are also more likely to seek medical assistance for their diseases (27). Females are typically more conscious of their symptoms (28) and communicate with doctors more effectively (29). In line with previous studies, chronic diseases were higher in females in this study. In this respect, the prevalence of hypertension, depression, and thyroid disorders was greater in females than in males.
Age, as previously stated, is also another risk factor for polypharmacy (19, 20) because the coexistence of chronic illnesses rises with age. Although people in the age range of 60 - 70 years had the greatest rates of polypharmacy, younger individuals aged 50 - 59 years were also substantially more prone to experience polypharmacy than those in the age range of 35 - 49 years. Similar to our findings, Oktora et al. discovered that polypharmacy increased more than two times from 1999 to 2014, and this rise was not confined to older people (30).
It has been reported that the prevalence of MM is increasing in young adults in low- and middle-income countries (16). Ebrahimoghli et al. reported that the absolute number of MM was higher in those younger than 65 years. Moreover, they suggested that MM should be monitored in all age groups, and the evaluation of MM merely in the elderly population can lead to neglecting a large number of MM in the young population (31). Based on these data, it is implied that the age of chronic disease in the Iranian people would be several years lower than that in adjacent countries, showing that screening for polypharmacy may be required for the middle-aged Iranian population.
We discovered that a low education level and socioeconomic status (WSI) were risk factors for polypharmacy. A similar correlation has been shown previously, although mostly in elderly patients (32-34). One reason is that individuals with lower education have greater multimorbidity prevalence (35, 36), which might be attributable to poor socioeconomic situations or a lack of interest in preventative measures. According to this study, having a poor socioeconomic position (WSI) increases the likelihood of polypharmacy. Vyas et al. showed that a poor level of socioeconomic status is inversely related to polypharmacy, which is consistent with our findings (20).
For both genders, a dose-response association was detected for physical activity level (MET), with declining levels of physical activity associated with an increased risk of polypharmacy. Baldoni et al. (24) and Volaklis et al. (37) showed similar results. The involvement of low levels of physical activity in polypharmacy may be explained by the fact that low physical activity increases the likelihood of different chronic conditions, such as obesity, hypertension, Diabetes Mellitus (DM), and tumors, which can raise the demand for medication use (38, 39).
In the present research, we discovered that the coexistence of chronic diseases is a powerful indicator of polypharmacy in this population. These findings are in agreement with those of Assari et al., who discovered that more chronic diseases are linked with polypharmacy (taking > 5 medicines) and hyper polypharmacy (taking > 10 medicines) (40). Besides, the Australian research by Taylor et al. (11) and Vyas et al. (20) discovered that MM is connected to polypharmacy.
Overweight and obesity raise the rate of polypharmacy in a trend-like manner. Similar results were reported by Pappa et al. in Greece (13), Bardel et al. in Sweden (41), and Carmona-Torres in Spain (42). This is because overweight/obesity is regarded as a risk factor for numerous NCDs, which may need more drugs for therapy (42, 43). Cardiovascular medicines were the most frequently prescribed drugs in our population-based analysis, which is consistent with prior research (15, 44, 45). Antihypertensives are placed at the top, closely followed by statins. The possible cause is hypertension, which is associated with the greatest risk of CVD among Iranians (46). Hypertension contributes largely to CVD, ranging from 17.3% to more than 20% in Iranian people over the age of 18 (47) and 26.9% in the population between 40 and 75 years old (48).
Because of the high incidence of neurologic and psychiatric diseases in this study, nervous system medications were the second most often prescribed drug category (17.1%). Depression is the primary cause of health-related disability worldwide, based on a World Health Organization report (49). Depression and mental health disorders are quite frequent in Iran, and their incidence is rising. In line with our results, a comprehensive study by Montazeri et al. revealed the prevalence of depression ranging from 6% to 73% in various populations (50). Endocrine disorder medicines were the third most commonly prescribed drugs in this research.
Blood glucose-lowering and anti-thyroid drugs were the most commonly prescribed sub-classes in this pharmaceutical class. This is consistent with the chronic disease trend observed in the Azar cohort group. In 2014, the average incidence of diabetes in the Eastern Mediterranean Region (EMRO) age groups was 13.7%, the highest incidence among WHO regions (51). Diabetes was prevalent in 11.9% of individuals aged 25 - 70 years in Iran (2011), a 35% rise from 2005. It is projected that almost 9.2 million Iranians might develop diabetes by 2030 (52).
Analgesics, NSAIDs, and medicines used to treat musculoskeletal and joint diseases were placed fourth and fifth, possibly due to the high prevalence of chronic headache and rheumatoid diseases. This discovery with analgesics and NSAIDs poses challenges, as these medications are not meant to be administered long term.
4.1. Strengths and Limitations
The advantages of this study are its large sample size and subject age range of 35 to 70 years. The majority of prior research examined polypharmacy in older people or elderly inpatients, and it has received less attention in the general population aged < 60 years. In addition, our analysis contained a thorough list of independent factors that may be related to polypharmacy.
This study was designed cross-sectionally. As a result, we cannot draw any causal relationships. A longitudinal study is required in the future. Furthermore, our findings were based on self-reports of the number of drugs used and chronic diseases. There is a need to analyze medicines rather than rely on self-reported data from patients. Nonetheless, most large-sample epidemiological research uses self-reported data on medicines and chronic diseases.
4.2. Conclusions
Low socioeconomic status, obesity, increasing age, low physical activity, chronic health conditions, and MM were associated with the prevalence of polypharmacy in the Azar cohort aged 35 to 70 years. Furthermore, our study emphasized the importance of routine monitoring to evaluate polypharmacy among those aged 35 to 59 and the elderly. Future research is required to explore the underlying cause of these relationships. Physicians should carefully assess drug suitability, especially in multimorbid and obese patients, to prevent excessive polypharmacy and its potential negative impacts.