1. Background
Medicines are one of the pillars of the health sector, and the provision of health services without them cannot be sustainable (1, 2). These inputs, along with the workforce and healthcare infrastructure, play an essential role in providing healthcare services and achieving universal health coverage (2, 3). Medicines play a significant role in the recovery of patients and are often considered an essential element in the treatment process (1, 4). Hence, appropriate access to medicines could promote health outcomes and address healthcare inequalities (3). Equal access to medicines, like other essential health services, is emphasized by the World Health Organization (WHO) as a powerful means of promoting health equity (1). Despite significant progress in providing various medicines for different clinical conditions, it seems that different countries and socio-economic groups may have heterogeneous access to these critical factors (5). This can lead to unethical inequalities in access to health services in the world.
Although high-income countries do not face the problem of access to medicine on average, people from different socio-economic classes in these countries do not necessarily have the same access to medicines (6-9). The situation seems even worse for low-income and middle-income countries (LMICs). These countries are more likely to face inequality in access to medicines (3, 10). Moreover, equal access to equal needs may also be challenging in the pharmaceutical sector; it is believed that patients with chronic conditions may not have adequate access to medicines (11, 12). These facts explain why the WHO pays special attention to drugs. These healthcare inputs have a unique role in providing healthcare services, and ensuring access to them is important for health systems.
The pharmaceutical sector absorbs remarkable resources to provide different medicines. According to the WHO report, 40% of treatment costs are spent on medicines (13). Additionally, over a quarter of total health expenditure in LMICs is related to pharmaceutical expenditure (14). However, this could not ensure access to medicines in these countries. Significant disparities in medicines use were reported from LMICs due to unaffordability and inappropriate use of medicines (15). The point is that the public sector may not have all the required medicines, and these medicines may have different prices in the private sector (16). In this situation, the risk of catastrophic health expenditure for vulnerable groups may increase without financial protection (17).
2. Objectives
The health system of Iran pays special attention to medicines and allocates substantial subsidies for their provision. The trend of pharmaceutical prices in Iran shows a clear increase in pharmaceutical expenditures in recent decades (18). After the health transformation plan (HTP), the government's share of health financing and pharmaceutical spending in Iran increased (19). However, it seems this policy did not necessarily guarantee access to medicines. Another problem is international sanctions, which have had a negative impact on access to medicine in Iran. Although some studies investigated socio-economic inequality in self-medication (20) and even the use of herbal medicines (21), there is no evidence of socio-economic inequalities in prescribed medicine use in Iran. In this study, unlike previous studies, the required data was obtained from the healthcare utilization survey, which better shows the health-seeking behavior than the income and expenditure survey. Access to medicine is one of the most important requirements for access to health services, and understanding the inequality in access to pharmaceutical services can guide policymakers to increase access to health services. Therefore, this study aimed to prepare such evidence and explain potential inequalities in the pharmaceutical sector of Iran.
3. Methods
This study is a secondary data analysis of cross-sectional data from a national survey. This survey was conducted in 2016 to provide evidence about the need for health services and the utilization of these services in Iran. Face-to-face interviews with household members were used in this nationwide survey. A sample of Iranian households (22470) living in urban and rural areas of Iran was chosen through three-stage cluster sampling. In the first stage, the regions (main sample units) were selected based on the probability proportional to the number of households in each region. Sampling units were based on the recent national census conducted by the Iranian Statistical Center in 2011. In the second step, systematic sampling was used to select one block from the selected regions. Furthermore, 10 households in each block were randomly selected. Interviews were conducted for all selected family members (N = 78 378). The participants aged 15 years or older who reported the need for health services (N = 13005) were included in our analysis.
Two questionnaires were used to gather data in this survey. Demographic and socio-economic characteristics, along with the need for health services, were collected in the first questionnaire. The second questionnaire was dedicated to evaluating the use of outpatient and inpatient services. This questionnaire also asked the participants about the use of prescribed and non-prescribed medicines we used as outcome variables.
3.1. Variables
The self-reported prescribed and non-prescribed medicine use were our outcome variables in this study. The following questions were used to define these variables. Participants' response to "have you used the prescribed medication in the last two weeks?" was used to define the prescribed medicine use. On the other hand, non-prescribed medicine use was obtained by answering various questions. First, the answer to "have you used any non-prescribed medicines from pharmacies during the last two weeks?" Was used to find people who had taken the drug without a prescription. This question was asked to those who had health-seeking behavior. Second, the answer to "have you had any self-medication during the last two weeks" was used to find people with a history of self-medication. This question was asked to those who had no health-seeking behavior. Since the use of these drugs in previous questions is generally not under the supervision of a doctor, the answers to these questions ultimately defined non-prescribed medicine use.
Considering previous evidence about the explanation of socio-economic inequality in healthcare, different independent variables were included in our analysis. Gender (male/female), age (15 - 29/30 - 59/60 and above), and the number of outpatient needs (one/two or above) were considered as need factors. Non-need factors include wide-range socio-economic variables such as marital status (married/widowed or divorced/single), education (illiterate/primary/secondary/diploma/higher), employment status (employed/unemployed/retired/student/housekeeper), area of residence (urban/rural), basic insurance (yes/no), private insurance (yes/no) and economic status (poorest/poor/middle/rich/richest). The survey used did not ask questions about household income or expenses but asked them about their assets. This allowed us to use principal component analysis to construct a proxy for economic status based on household assets.
3.2. Equity Analysis
To measure socio-economic inequality in the medication, the concentration index (CI) was used. This index is a well-established measure for assessing inequality in the health sector (22). For individual data, CI could be defined as follows:
Where h is the medicine use, r is the fractional rank of the independent variable, and µ is the mean of our outcome. The CI range between -1 and + 1 with zero indicating equality and negative values indicating the concentration of outcome among the lowest socio-economic groups and vice versa. Since our outcomes in the current analysis are binary variables, the Erreygers normalized concentration index (ECI) was used to measure inequality (23). The ECI can be obtained as follows:
Where μm is the weighted average of medicine use and b and a indicate its upper and lower bounds.
Concentration index can be decomposed to find the contribution of different factors. To do this, a linear incremental regression model of health criterion (hi) on its determinants is required (24). This model can be shown as follows:
Where, the “xk" variables are determinants of health variables, and ε is an error term. Given the linear regression model, the ECI can be written as (23):
Where, βk shows the marginal effect of independent factors obtained through logistic regression. Moreover,
4. Results
Most of the study subjects were women between 30 and 59. Nearly twenty percent of participants reported more than one outpatient need. Other descriptive characteristics of these variables are available in Table 1. The CI of prescribed and non-prescribed medicine use was represented in Iran Table 2. This index was positive and statistically significant for the prescribed medicine use, indicating a pro-rich distribution of this outcome in Iran. On the other hand, the CI for non-prescribed medicine use was negative and statistically significant, indicating the existence of pro-poor inequality.
| Variables | All Sample | Prevalence of Prescribed Medicine Use | Prevalence of Non-prescribed Medicine Use |
|---|---|---|---|
| Need Factors | |||
| Gender | |||
| Male | 5,210 (40.06) | 2464 (47.29) | 1,408 (27.02) |
| Female | 7,795 (59.94) | 3867 (49.61) | 2,008 (25.76) |
| Age | |||
| 15 - 29 | 2,895 (22.26) | 1416 (48.91) | 681 (23.52) |
| 30 - 59 | 7,068 (54.35) | 3417 (48.34) | 1,823 (25.79) |
| > 60 | 3,042 (23.39) | 1498 (49.24) | 912 (29.98) |
| Number of outpatient needs | |||
| One | 10,420 (80.12) | 5218 (50.08) | 2,253 (21.62) |
| Two or above | 2,585 (19.88) | 1113 (43.06) | 1,163 (44.99) |
| Non-need Factors | |||
| Marital status | |||
| Married | 9,720 (74.74) | 4789 (49.27) | 2,451 (25.22) |
| Widowed or divorced | 1,377 (10.59) | 658 (47.79) | 436 (31.66) |
| Single | 1,908 (14.67) | 884 (46.33) | 529 (27.73) |
| Education | |||
| Illiterate | 3,446 (26.5) | 1616 (46.89) | 1,072 (31.11) |
| Primary | 3,353 (25.78) | 1661 (49.54) | 843 (25.14) |
| Secondary | 2,104 (16.18) | 1043 (49.57) | 512 (24.33) |
| Diploma | 2,289 (17.6) | 1106 (48.32) | 566 (24.73) |
| Higher | 1,813 (13.94) | 905 (49.92) | 423 (23.33) |
| Employment status | |||
| Employed | 3,101 (23.84) | 1436 (46.31) | 837 (26.99) |
| Unemployed | 1,606 (12.35) | 745 (46.39) | 447 (27.83) |
| Retired | 1,438 (11.06) | 717 (49.86) | 404 (28.09) |
| Student | 810 (6.23) | 413 (50.99) | 216 (26.67) |
| Housekeeper | 6,050 (46.52) | 3020 (49.92) | 1,512 (24.99) |
| Area of residence | |||
| Urban | 8,698 (66.88) | 4401 (50.60) | 2,189 (25.17) |
| Rural | 4,307 (33.12) | 1930 (44.81) | 1,227 (28.49) |
| Basic insurance | |||
| No | 792 (6.09) | 318 (50.77) | 247 (31.19) |
| Yes | 12,213 (93.91) | 6013 (49.23) | 3,169 (25.95) |
| Private insurance | |||
| No | 10,550 (81.12) | 5013 (46.31) | 2,861 (27.12) |
| Yes | 2,455 (18.88) | 1318 (53.69) | 555 (22.61) |
| Economic status | |||
| Poorest | 2,630 (20.22) | 1165 (44.30) | 744 (28.29) |
| Poor | 2,583 (19.86) | 1216 (47.08) | 748 (28.96) |
| Middle | 2,591 (19.92) | 1313 (50.68) | 657 (25.36) |
| Rich | 2,600 (19.99) | 1275 (49.04) | 673 (25.88) |
| Richest | 2,601 (20) | 1362 (52.36) | 594 (22.84) |
a Values are expressed as No. (%).
| Medicine Use | ECI | SE | P-Value |
|---|---|---|---|
| Prescribed | 0.067 | 0.010 | 0.000 |
| Un- prescribed | -0.064 | 0.009 | 0.000 |
Abbreviation: ECI, Erreygers concentration index.
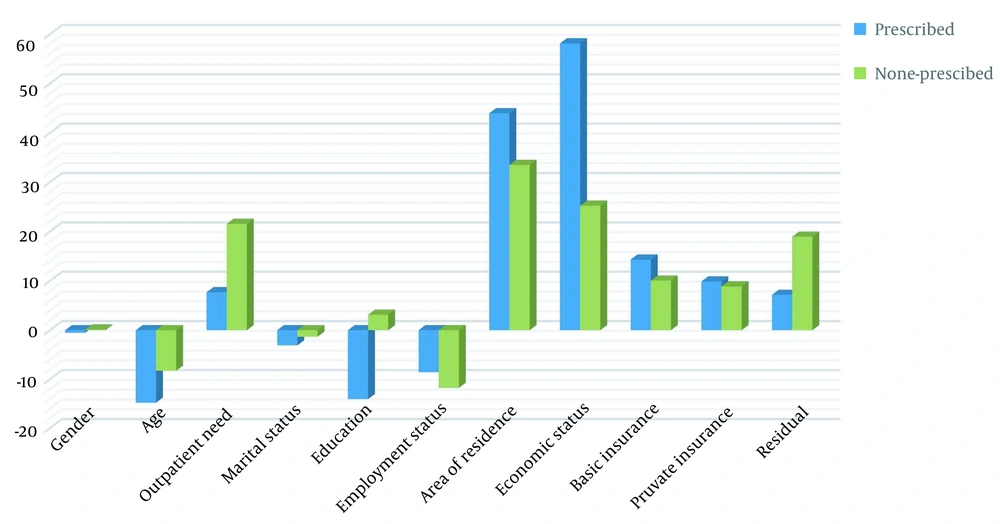
The decomposition of socio-economic inequality in the prescribed and non-prescribed medicine use. The second column of these tables shows the marginal determinants of the use of prescribed and non-prescribed medicine use. These tables also show each determinant factor's absolute contribution (cont.). The positive (negative) value of cont. indicated that the determinant factor increased (decreased) the socio-economic inequality in the prescribed medicine use. The economic status of participants was the main contributor to the pro‐rich inequality in prescribed medicine use. This factor explains about 60 percent of the observed inequality. Area of residence was another main contributor to socio-economic inequality in the prescribed medicine use. Private and basic health insurance and the number of outpatient needs were other positive contributors to the socio-economic inequality. Other factors had negative contributions to the observed inequality. After adjustment for the need factors, it is demonstrated that the degree of horizontal inequality was 0.072 indicating pro-rich inequity in the prescribed medicine use in Iran (Table 3). As Table 4 shows, the location of residence accounted for 33 percent of inequality in non-prescribed medicine use and was, therefore, the most critical factor contributing to inequality. The economic status was another key factor contributing to this inequality, which alone explained nearly 25% of it. The number of needs for health services and health insurance (basic and private) explained about 21 and 18 percent of the inequality, respectively. These factors significantly contributed to the socio-economic inequality in non-prescribed medicine use. The two estimated models had different residual component, but it was not very high in both cases. The residual component in the second model was higher, implying that unknown factors had a more significant impact on inequality. After subtracting the absolute contribution of the need factors from the concentration index, the horizontal inequity decreased but still showed the concentration of non-prescribed medicine use among the poor. The relative contribution of various factors explaining socio-economic inequality in the use of prescribed and non-prescribed drugs in Iran is shown in Figure 1.
| Variables | Marginal Effect | ECI | Cont. | Percent Cont. |
|---|---|---|---|---|
| Need Factors | ||||
| Gender | ||||
| Female | 0.004 | -0.034 | 0.000 | -0.515 |
| Age | ||||
| 30 - 59 | -0.025 | 0.149 | 0.003 | -12.310 |
| 60 and above | 0.010 | -0.185 | 0.000 | -2.503 |
| Number of outpatient need | ||||
| Two or above | -0.070 | -0.092 | 0.001 | 7.684 |
| Non-need Factors | ||||
| Marital status | ||||
| Widowed or divorced | -0.012 | -0.119 | 0.000 | 0.931 |
| Single | -0.063 | 0.073 | -0.001 | -4.022 |
| Education | ||||
| Primary | 0.010 | -0.132 | 0.000 | -2.054 |
| Secondary | 0.000 | 0.015 | 0.000 | -0.006 |
| Diploma | -0.029 | 0.168 | -0.001 | -5.200 |
| Higher | -0.027 | 0.299 | -0.001 | -6.835 |
| Employment status | ||||
| Unemployed | 0.038 | -0.065 | 0.000 | -1.815 |
| Retired | 0.014 | -0.014 | 0.000 | -0.129 |
| Student | 0.073 | 0.078 | 0.000 | 2.126 |
| Housekeeper | 0.037 | -0.085 | -0.001 | -8.773 |
| Area of residence | ||||
| Rural | -0.060 | -0.367 | 0.007 | 43.963 |
| Economic status | ||||
| Poor | 0.011 | -0.340 | -0.001 | -4.299 |
| Middle | 0.042 | -0.058 | 0.000 | -2.879 |
| Rich | 0.030 | 0.271 | 0.002 | 9.686 |
| Richest | 0.065 | 0.714 | 0.009 | 55.614 |
| Basic insurance | ||||
| Yes | 0.071 | 0.036 | 0.002 | 14.295 |
| Private insurance | ||||
| Yes | 0.033 | 0.261 | 0.002 | 9.873 |
| Total observed | 0.062 | 92.83 | ||
| Residual | 0.005 | 7.16 | ||
| Horizontal inequity | 0.072 | |||
Abbreviations: Cont., contribution; ECI, Erreygers concentration index.
| Variables | Marginal Effect | ECI | Cont. | Percent Cont. |
|---|---|---|---|---|
| Need Factors | ||||
| Gender | ||||
| Female | 0.001 | -0.034 | 0.000 | 0.137 |
| Age | ||||
| 30 - 59 | 0.036 | 0.149 | 0.012 | -18.373 |
| 60 and above | 0.037 | -0.185 | -0.006 | 10.096 |
| Number of outpatient need | ||||
| Two or above | 0.188 | -0.092 | -0.014 | 21.537 |
| Non-need Factors | ||||
| Marital status | ||||
| Widowed or divorced | 0.027 | -0.119 | -0.001 | 2.112 |
| Single | 0.051 | 0.073 | 0.002 | -3.443 |
| Education | ||||
| Primary | -0.026 | -0.132 | 0.004 | -5.583 |
| Secondary | -0.015 | 0.015 | 0.000 | 0.225 |
| Diploma | -0.016 | 0.168 | -0.002 | 3.051 |
| Higher | -0.021 | 0.299 | -0.003 | 5.435 |
| Employment status | ||||
| Unemployed | -0.019 | -0.065 | 0.001 | -0.949 |
| Retired | -0.024 | -0.014 | 0.000 | -0.242 |
| Student | 0.011 | 0.078 | 0.000 | -0.326 |
| Housekeeper | -0.042 | -0.085 | 0.007 | -10.266 |
| Area of residence | ||||
| Rural | 0.044 | -0.367 | -0.021 | 33.492 |
| Economic status | ||||
| Poor | 0.008 | -0.340 | -0.002 | 3.386 |
| Middle | -0.002 | -0.058 | 0.000 | -0.120 |
| Rich | -0.003 | 0.271 | -0.001 | 1.014 |
| Richest | -0.023 | 0.714 | -0.013 | 20.953 |
| Basic insurance | ||||
| Yes | -0.048 | 0.036 | -0.006 | 10.052 |
| Private insurance | ||||
| Yes | -0.029 | 0.261 | -0.006 | 8.869 |
| Total observed | -0.052 | 81.055 | ||
| Residual | -0.012 | 18.945 | ||
| Horizontal inequity | -0.055 | |||
Abbreviations: Cont., contribution; ECI, Erreygers concentration index.
5. Discussion
Socio-economic inequalities in medicines prescription can impose substantial burdens on the health systems. Current research investigates such inequalities in the pharmaceutical sector of Iran. In general, while non-prescribed medicines were concentrated among disadvantaged groups, a significant pro-rich was observed in the use of prescribed medicines in Iran. We explained these socio-economic inequalities through decomposition analysis.
The concentration index indicated a pro-rich distribution of prescribed medicine use in Iran. We also adjusted this pro-rich inequality relative to the need factors that lead to a pro-rich horizontal inequity in the prescribed medicine use. Our finding is inconsistent with previous studies (25, 26) that reported favorable access to medicines in the Iranian pharmaceutical market. It seems that these studies neglect the accessibility dimension of access that is predominantly related to the household's ability to pay. But the results of some studies indicate the existence of inequality in medicine use in Iran (27, 28), which is consistent with our results. Inequality in the Iranian pharmaceutical sector can be consistent with other studies showing inequality in health services (29, 30). Therefore, since healthcare services are concentrated among the better-off, a rich distribution of prescribed medicine use in Iran can be justified. Our results are consistent with previous studies that observed pro-rich inequality in pharmaceutical spending (31) in Brazil and also prescribed medicine use in Canada, Denmark, and Uruguay (8, 32, 33). Previous studies in China have shown pro-rich inequality in anti-diabetic (11) and anti-hypertensive (12) drug treatment. One international study also reported different socio-economic inequalities in terms of concentration index for secondary prevention of cardiovascular disease in some of LMICs and Sweden. While countries such as Saudi Arabia, China, Colombia, India, Pakistan, and Zimbabwe had pro-rich socio-economic inequality, pro-poor distributions were found for Sweden, Brazil, Chile, Poland, and the occupied Palestinian territory (34). This showed a significant variation in the access to medicines in the world.
The results showed that the economic status of the households explains about 60% of the observed pro-rich inequality in prescribed medicine use. Although there are no studies with the same methodology that surveyed adult participants, our results are in line with a former study that tried to explain socio-economic inequities in medicine use among Brazilian children (35). Another study in China found income to be the most important factor explaining socio-economic inequality in diabetes medication (11). Our result is consistent with a previous Iranian study that reported inequality in healthcare use (29). There are substantial debates about decreasing subsidies in the pharmaceutical market of Iran that may exuberate socio-economic inequality in medication and healthcare utilization. Location of residence was another main contributor to the observed inequality in the prescribed medicine use. Similar to our findings, other studies (35, 36) showed that people living in remote areas have poor access to essential medicines. Although Iran has a well-organized rural health system (37), a former study (29) showed that residence in rural areas could increase pro-rich inequality in healthcare utilization. Basic and private health insurance were other factors that played a positive role in inequality in the prescribed medicine use. According to Anderson's model of behavioral use of health care, health insurance can be considered as an enabling factor that facilitates access to health care services (38). Expanding the health insurance benefits package could increase access to needed drugs in Iran. However, blind health financing reforms may increase healthcare costs by increasing pharmaceutical expenses. Due to the positive impact of the national essential list on universal health coverage (1), Iran should promote this strategy and require various health insurance plans to include these drugs in their benefits packages.
The concentration index also revealed an inequality in favor of the poor in non-prescribed medicine use in Iran. This finding contrasts with a former Iranian study (20) that reported pro-rich socio-economic inequality in self-medication in Iran. In previous research, authors used household budget data provided by the Statistics Center of Iran. These data are monetary data and do not accurately show health-seeking behaviors. Since poor households may not have enough affordability to pay for non-prescribed medicines, the definition of self-medication in this study may be restrictive. Hence, it seems self-medication in Iran is distributed among lower socio-economic groups. This means that poor people in Iran generally use medicines they already have at home or probably seek to use over-the-counter medicines to meet their health needs. It should be noted that in this study, self-medication was used both for people who did not seek healthcare services and for those who used pharmacy drugs without a prescription. Of course, the frequency of the first case was higher in our study. Our finding is consistent with a previous local study (27) which showed that self-medication in a province of Iran is concentrated among the poor. There were no international studies on socio-economic inequality in non-prescribed medicine use. However, there are contradictory results observed regarding the socio-economic determinants of this kind of medicine use. Some studies (39) have shown that higher socio-economic groups are more likely to use non-prescribed medicines. In contrast, other studies (40, 41) have shown that this practice is more common among lower socio-economic groups. Decomposition analysis showed that residence was the main driver of pro-poor inequality in non-prescribed medicine use. As previously discussed, rural residents have poor access to health care, especially for complex healthcare needs. Economic status was another major contributor to the pro-poor inequality in non-prescribed medicine use, explaining about 25 percent of it. This is could be related to the higher use of non-prescribed medicine among disadvantaged groups, which has been confirmed in other studies (40, 41). The number of healthcare needs was another key determinant in the inequality in this type of medicine use. This indicates that people with poor health take medication to meet their health needs without consulting a doctor. Hence, healthcare authorities should facilitate the access of people in need of health services to the required medicines. In any case, it seems that self-medication in Iran is related to the accessibility of healthcare services. Therefore, the implementation of policies that increase access to health services by increasing insurance coverage can also greatly reduce the pro-poor inequality in non-prescribed medicine use. However, the impact of cultural and behavioral factors on self-medication should not be overlooked (42), which unfortunately were not considered in this study.
Although this research provided valuable evidence on socio-economic inequality in Iran's pharmaceutical sector, some limitations in the interpretation of the results should be considered. First, this study only explored overall medication and could not be used for socio-economic inequality for specific drugs. Socio-economic disparities for some drugs may be much greater. It is suggested that future studies perform inequality analysis for different drugs. Second, the self-reported nature of the data may lead to recall bias. Third, this is a cross-sectional analysis, and our findings necessarily fail to demonstrate a causal relationship between the independent variables and medicine use.
5.1. Conclusions
We observed significant pro-rich inequality in prescribed medicine use as well as pro-poor inequality in non-prescribed medicine use in Iran. Economic status and location of residence were key factors that contributed to the pro-rich inequality in the use of prescribed medicines. The order of these factors for socio-economic inequality in non-prescribed medicine use was reversed. Anyway, it seems that paying subsidies to disadvantaged households and facilitating the access of residents in rural areas can reduce socio-economic inequalities in the pharmaceutical market of Iran. In addition, it seems that the inclusion of the National Essential Medicines Strategy in healthcare financing can moderate the socio-economic inequalities in medicine use in Iran.