1. Background
Prescribed medications significantly improve an enormous range of health outcomes. On the other hand, it is well documented that prescribed drugs also may cause a considerable health burden. These adverse drug events (ADEs) have become a major cause of morbidity and mortality (1, 2). It has been estimated that about 6.5% of all emergency hospital admissions are drug-related, at least half of which are judged preventable (3, 4), and the additional annual costs of ADEs have been estimated to be USD 21 million per 100 000 adults (5). The risk of adverse effects and harm increases with increasing numbers of medications. Polypharmacy is defined as the concurrent use of multiple drugs to treat one or more conditions by a single patient (6-8). Previous evidence suggests that polypharmacy is a significant risk factor for ADEs (9, 10).
The main reasons for polypharmacy are aging and multimorbid patients (6, 11) and a proliferation in evidence-based guidelines (12). Polypharmacy patients are at increased risk for various negative outcomes such as inappropriate medication use, medication errors, poor compliance, poor disease control, and death (9, 13, 14). Additionally, polypharmacy has become a substantial healthcare expenditure burden. According to the literature, polypharmacy is associated with an annual estimated cost of $50 billion US, which is increasing over time (15).
These alarming reports make polypharmacy an area of grave concern and a potential target for reducing preventable adverse events. A complete understanding of the polypharmacy pattern is required to advance this agenda. For example, the increased prevalence of polypharmacy has been reported in most developed countries during the last decades (16, 17). Yet, few studies have documented the pattern of polypharmacy in low- and middle-income countries (LMICs), if not non-existent. However, the issue of polypharmacy seems to be more important in LMICs, where 80% of non-communicable disease (NCDs) deaths occur (18).
2. Objectives
In Iran, as an LMIC, we identified a unique opportunity to study polypharmacy patterns among a large outpatient population in East Azerbaijan province using the pharmaceutical dispensing records of the most prominent Iranian health insurer. This study has four primary aims: First, we aim to estimate the prevalence of polypharmacy among this population. Second, we examine the continuity of polypharmacy. Third, we estimate the predictor factors of being exposed to polypharmacy. And finally, this paper aims to identify the common therapeutic classes involved in polypharmacy. The results of this population-based study could assist in the effective planning and provision of quality healthcare services and improve patient safety.
3. Methods
3.1. Study Design, Data, and Population
We conducted a retrospective claims data-based cohort study. Medication and demographic data for this study were drawn from the claims database of the Iranian Health Insurance Organization (IHIO) for East Azerbaijan Province. This database includes each individual’s anonymized unique insurance number, age, gender, medical institution identification number, date of prescription, prescriber identification number, and generic name of prescribed drugs.
All individuals aged ≥ 20 years who received at least one prescription drug from March 1, 2020, to May 31, 2020 (the main three-month period of the study) were included in the study and followed for another three months of October 1, 2020, to December 31, 2020, to investigate chronic polypharmacy.
3.2. Chronic Health Conditions
Because individual-based epidemiological data for NCDs are unavailable within the country, the major chronic health conditions were derived via medication mapping using the recently developed pharmacy-based framework for identifying chronic conditions in Iran (19, 20). Codes for the identification of selected chronic conditions are presented in Appendix 1 (see Supplementary File).
3.3. Identification of Polypharmacy
First, we defined polypharmacy as the concurrent use of five or more different medications for three months. This cut-off point has been widely used and accepted as clinically relevant polypharmacy throughout the pharmacoepidemiologic literature (6-8). To measure the number of medications, they were classified using the anatomical therapeutic chemical (ATC) classification index of the World Health Organization (21). The unit of medication was applied as the 3rd ATC level administered. This pharmacological categorization is considered more appropriate than other subgroups (21, 22). Second, we estimated two standard polypharmacy measures (cumulative and continuous). We defined cumulative polypharmacy as the sum of all prescribed medications by one patient during the main three-month study period. We also calculated continuous polypharmacy. For this purpose, we identified constant exposure to polypharmacy by using a second three-month time window (follow-up period) with a three-month interval. In this regard, we defined continuous polypharmacy as the sum of all patients recognized as experiencing polypharmacy in both study periods (i.e., in the primary and follow-up periods).
3.4. Identification of Polypharmacy Composition
The ten most frequently prescribed medication classes (3rd level ATC code: Pharmacological subgroup) were calculated for patients with cumulative and continuous polypharmacy.
3.5. Statistical Analysis
All data management and statistical analyses were carried out using the STATA MP, V.16. Descriptive statistics were performed for all variables of interest. The prevalence of polypharmacy was presented as percentages with their associated 95% confidence intervals (CI). χ2 tests were applied to compare categorical variables between groups. The Student's t-test was used for the comparison of continuous variables. A multivariable logistic regression model was applied to estimate the odds ratios (OR) and their 95% CI to identify predictive factors of being exposed to polypharmacy. We constructed separate models for cumulative and continuous polypharmacy. The significance level was set at 0.05 for all analyses.
4. Results
4.1. Patients Characteristics
Three hundred seven thousand eight hundred twenty patients aged 20 years and older received at least one drug agent during the main study period. The mean age was 49.8 years (SD = 17.8), and 62.9% were female. Diabetes, cardiovascular disease (CVD), chronic obstructive pulmonary disease (COPD), and cancer were inferred (by the use of medication data) in 10.9%, 26.8%, 7.2%, and 0.7% of the study population, respectively (Table 1).
| All Patients | Prevalence of Cumulative Polypharmacy, No. (%) | Prevalence of Continuous Polypharmacy, No. (%) | |
|---|---|---|---|
| No. (%) | 307,820 (100) | 87,137 (28.3), CI: 28.1 - 28.4 | 31,884 (10.4) |
| Sex | |||
| Female | 193,615 (62.9) | 56,437 (29.1) | 20,627 (10.6) |
| Male | 114,205 (37.1) | 30,700 (26.9) | 11,257 (9.9) |
| Age (y) | |||
| Mean ± SD | 49.8 ± 17.8 | 55.9 | 61.2 |
| 20 - 29 | 44,903 (14.6) | 7,383 (16.4) | 1,083 (2.4) |
| 30 - 39 | 57,057 (18.5) | 10,356 (18.1) | 1,639 (2.9) |
| 40 - 49 | 56,045 (18.2) | 13,370 (23.9) | 4,115 (7.3) |
| 50 - 59 | 55,600 (18.1) | 17,626 (31.7) | 7,605 (13.7) |
| 60 - 69 | 45,458 (14.8) | 16,577 (36.5) | 7,216 (15.9) |
| 70 - 79 | 28,794 (9.3) | 12,568 (43.6) | 5,975 (20.8) |
| 80+ | 19,963 (6.5) | 9,257 (46.4) | 4,251 (21.3) |
| Comorbiditiesa | |||
| Diabetes | |||
| Yes | 33,667 (10.9) | 18,270 (54.3) | 10,875 (32.3) |
| No | 274,153 (89.1) | 68,867 (25.1) | |
| CVD (including hypertension) | |||
| Yes | 82,429 (26.8) | 45,066 (54.7) | 23,588 (28.6) |
| No | 225,391 (73.2) | 42,071 (18.7) | 8,296 (3.7) |
| Cancer | |||
| Yes | 2,025 (0.7) | 912 (45.0) | 392 (19.4) |
| No | 305,795 (99.3) | 86,225 (28.2) | 31,492 (10.3) |
| COPD | |||
| Yes | 22,366 (7.2) | 12,999 (58.1) | 6,818 (30.5) |
| No | 285,454 (92.8) | 74,138 (26.0) | 25,066 (8.8) |
Characteristics of Included Population and Prevalence of Polypharmacy Measures Among Them in Terms of Variables of Interest
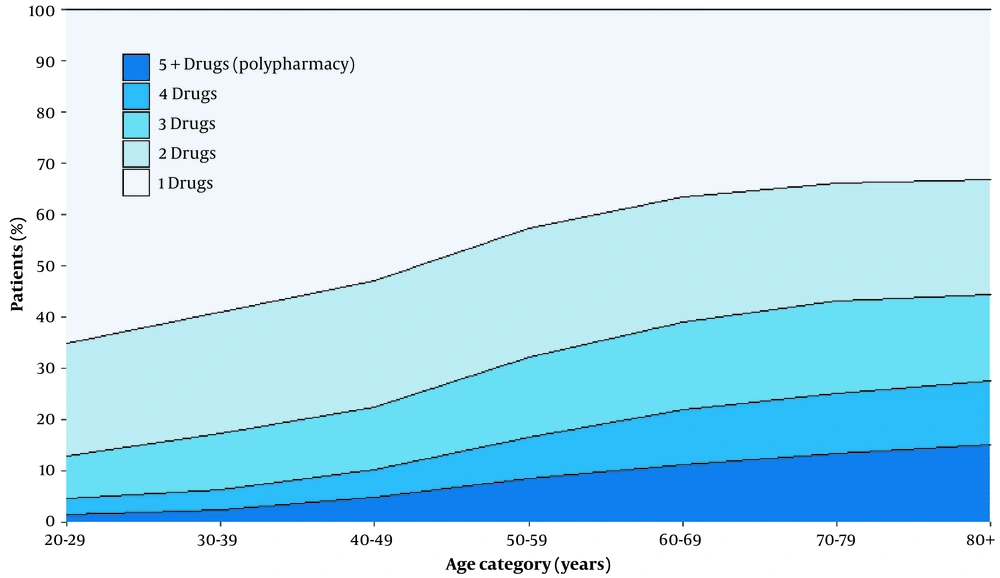
4.2. Medication Use
The mean number of drugs used by the study population in the main study period was 3.7 (± 2.6). The mean number of prescribed medications was 3.7 (± 2.6) and 3.6 (± 2.5) for females and males, respectively (P < 0.001). Overall, 18.0% of patients had a prescription for only one drug, 21.5% received two medications, 18.9% were prescribed three medications, 13.3% were utilizers of four medications, and 28.3% were exposed to more than four medications (i.e, polypharmacy). The distribution of the number of drugs used in different age groups during the main study period is presented in Figure 1. The number of medication use increased with age.
4.3. Polypharmacy
Of 307,820 adults (≥.20 years old), 87,137 (28.3%, 95% CI 28.1% - 28.4%) were exposed to polypharmacy in the main study period. The prevalence of cumulative and continuous polypharmacy is summarized in Table 2. Of these 87,137 polypharmacy patients, 31,884 individuals (36.6%) also remained exposed to polypharmacy in the follow-up period, resulting in an overall prevalence of continuous polypharmacy of 10.4%. Table 1 exhibits the prevalence of polypharmacy measures among the overall population and by variables of interest.
| Variables | Cumulative Polypharmacy | Continuous Polypharmacy | ||
|---|---|---|---|---|
| OR a | 95% CI | ORa | 95% CI | |
| Sex | ||||
| Male (base) | 1 | - | 1 | - |
| Female | 1.21*** | 1.19 - 1.23 | 1.19*** | 1.15 - 1.22 |
| Age (y) | ||||
| 20 - 29 (base) | 1 | - | 1 | - |
| 30 - 39 | 1.06*** | 1.02 - 1.09 | 1.04 | 0.96 - 1.13 |
| 40 - 49 | 1.20*** | 1.16 - 1.24 | 1.89*** | 1.76 - 2.02 |
| 50 - 59 | 1.23*** | 1.19 - 1.27 | 2.12*** | 1.98 - 2.27 |
| 60 - 69 | 1.14*** | 1.10 - 1.18 | 1.69*** | 1.57 - 1.81 |
| 70 - 79 | 1.34*** | 1.29 - 1.40 | 2.0*** | 1.86 - 2.16 |
| 80+ | 1.54*** | 1.48 - 1.60 | 2.13*** | 1.97 - 2.30 |
| Comorbidities | ||||
| Diabetes | 1.83*** | 1.78 - 1.88 | 2.52*** | 2.44 - 2.60 |
| CVD | 4.00*** | 3.91 - 4.08 | 6.42*** | 6.22 - 6.63 |
| COPD | 3.37*** | 3.27 - 3.47 | 3.63*** | 3.51 - 3.77 |
| Cancer | 2.21*** | 2.01 - 2.44 | 2.31*** | 2.04 - 2.62 |
Predictors of Polypharmacy
The prevalence of polypharmacy measures was higher among females compared to males. On average, patients with cumulative polypharmacy and patients with a continuous episode of polypharmacy were older. The prevalence rates of polypharmacy were very importantly higher among patients exposed to each selected chronic condition (Table 2).
4.4. Predictors of Polypharmacy
Table 2 exhibits the estimated ORs for the predictors of polypharmacy among the study population. Compared with male patients, female patients were more likely to experience polypharmacy (cumulative: OR 1.21, 95% CI 1.19 - 1.23, continuous: OR 1.23, 95%CI 1.20 - 1.25). The results of multivariate logistic regression models indicated that chronic conditions are significantly associated with higher odds of being a polymedicated patient. Cardiovascular disease was associated with the highest odds of being exposed to polypharmacy among selected chronic conditions. Individuals with CVD were four times more likely to be exposed to cumulative polypharmacy (OR 4.00, 95% CI 3.91 - 4.08) than those without CVD. This association was stronger when considering continuous polypharmacy (OR 6.42, 95% CI 6.22 - 6.63).
4.5. Common Medication Classes Involved in Polypharmacy
Table 3 describes the most prescribed classes of medication among patients with cumulative and continuous polypharmacy.
| 4 Digits ATC | Name of the Drug Class | Percent | Cum. |
|---|---|---|---|
| Cumulative Polypharmacya | |||
| A02B | Drugs for peptic ulcer and gastro-oesophageal reflux disease | 5.03 | 5.03 |
| C07A | Beta-blocking agents | 4.92 | 9.95 |
| N06A | Antidepressants | 4.32 | 14.27 |
| C10A | Lipid-modifying agents, plain | 4.09 | 18.36 |
| B01A | Antithrombotic agents | 3.96 | 22.32 |
| A10B | Blood glucose-lowering drugs, excl. insulins | 3.86 | 26.18 |
| C09C | Angiotensin ii receptor blockers, plain | 3.76 | 29.94 |
| N03A | Antiepileptics | 3.63 | 33.57 |
| J01D | Antibacterials for systemic use | 3.46 | 37.03 |
| D11A | Other dermatological preparations | 3.32 | 40.35 |
| Continuous Polypharmacyb | |||
| C07A | Beta blocking agents | 5.41 | 5.41 |
| C10A | Lipid-modifying agents, plain | 4.99 | 10.4 |
| A10B | Blood glucose-lowering drugs, excl. insulins | 4.99 | 15.39 |
| A02B | Drugs for peptic ulcer and gastro-oesophageal reflux disease | 4.9 | 20.28 |
| B01A | Antithrombotic agents | 4.62 | 24.9 |
| C09C | Angiotensin ii receptor blockers, plain | 4.61 | 29.51 |
| N06A | Antidepressant | 4.21 | 33.72 |
| N03A | Antiepileptics | 3.93 | 37.65 |
| D11A | Other dermatological preparations | 2.82 | 40.47 |
| R06A | Antihistamines for systemic use | 2.71 | 43.18 |
The Ten Most Commonly Prescribed Medication Classes (3rd ATC Level) Among Patients with Cumulative and Continuous Polypharmacy
These common medication classes constitute about 40% - 43% of all prescription medication utilization by patients with polypharmacy. Almost all of the common medication classes (9 of 10) involved in cumulative polypharmacy were also identified as common medication classes among patients with continuous polypharmacy.
5. Discussion
We investigated this project's four crucial aspects of polypharmacy: Intensity, continuity, predictors, and composition. Only a few studies, if not non-existence, have evaluated these comprehensive dimensions of polypharmacy patterns in a similar population. Such evidence regarding these dimensions might inform the interventions aimed at polypharmacy management.
Our study showed that the prevalence of polypharmacy among adults (≥ 20 years old) was 28.3%. Although it might not be reasonably accurate to directly compare polypharmacy prevalence data across previous studies because of possible differences among the implemented methods (sample age, exposure difference, the nature of data sources, and unit of analyses) (23), the prevalence reported in the current study is remarkably comparable with what has been reported previously. For example, it was reported that across Europe, 32.1% of older adults experience polypharmacy per day (16). In addition, it is encouraging to compare this study's detailed results with other authors' findings. For example, Turner et al. found that 57 % of cancer patients aged ≥ 70 years were exposed to polypharmacy (24). This measure is calculated as 54% in our study (data is not shown). However, our results are somewhat lower than those of some other studies that examined polypharmacy based on detailed ATC categorization or longer exposure windows.
We also investigated the chronicity of polypharmacy exposure and found that continuous polypharmacy's prevalence varies from cumulative polypharmacy's prevalence. About 37% of the individuals with polypharmacy during the main study period also remained exposed to polypharmacy in the follow-up period (overall prevalence of continuous polypharmacy: 10.4%). This finding seems to be consistent with limited earlier observations. A study from Germany reported that 26.7% of older primary care patients (aged 70+) used five and more chronically prescribed drugs (25). We reported the prevalence of continuous polypharmacy for this age group as 21%. This finding is cause for concern for clinicians and healthcare policymakers regarding patient safety. In addition, it highlights that it is necessary to consider the dynamic aspect of polypharmacy in epidemiological studies and clinical practice.
We found a significant association between gender and the presence of polypharmacy when considering both cumulative and continuous perspectives. Consistent with prior international studies (26, 27), females were more likely to be exposed to polypharmacy. Hofer-Dückelmann provided a detailed discussion about the higher prevalence of polypharmacy among women and outlined various possible reasons (28). Not surprisingly, we found that age was an independent variable associated with polypharmacy, which can be explained by the exponential increase in the prevalence of morbidities accompanying advancing age (29). This association is mainly concerned in Iran because the elderly population is rising (30). However, what was surprising is that we noted that most patients with polypharmacy were younger than 65 years (62% - 65%), indicating that polypharmacy is not just an issue for the elderly. Our multivariate regressions also revealed that chronic conditions (retrieved from medication data) are another factor associated with polypharmacy. The same association was identified during previously published studies (31). This association is especially highlighted for prescribing for CVDs. Indeed, cardiovascular medications are not only the most commonly prescribed drugs among patients with polypharmacy but are also a strong predictor of polypharmacy (32), consistent with the clinical guidelines requiring treatment with multiple drug classes. Patients with multiple chronic conditions are in high need of pharmaceutical care.
The results of this study showed that the use of drugs was centered on drugs for peptic ulcer and gastro-esophageal reflux disease, beta-blocking agents, antidepressants, blood glucose-lowering drugs, and antithrombotic agents. This result is similar to the limited published studies (33).
Our study has important strengths and limitations. To the best of our knowledge, this is the first population-based Iranian study to investigate polypharmacy patterns among a large outpatient population using a real-world medication database. In addition, because the database used in our study was based on data initially collected at the time and site of dispensation and was used for financial mechanisms, the data have a much lower likelihood of containing the error. Another strength of the present study is that we examined the chronicity of polypharmacy, while the research has focused only on the cumulative dimension of polypharmacy. There are several potential weaknesses as well. Firstly, our estimates of chronic conditions were based on medication data. Although using medication data as a surrogate for comorbidities is viable, this approach has its well-recognized limitations (34).
Moreover, because IHIO's database does not include over-the-counter (nonprescription) and non-reimbursable prescription medications, it is reasonable to conclude that calculated prevalence rates might be underestimated. Finally, we could not verify whether patients used prescribed medicines because of the reliance on medication claims data. However, it still affords significant insights into the prescription pattern. Due to unavailable clinical data, it was also impossible to determine whether or not exposure to polypharmacy is appropriate.
5.1. Conclusions
Our study demonstrated that a considerable portion of medication utilizers experience polypharmacy which has important implications because of the well-recognized associated adverse consequences of polypharmacy. Individual-level characteristics such as age, gender, and morbidities predicted the likelihood of polypharmacy. Thus, polypharmacy is likely to be more prevalent among the Iranian population, given the aging population and increasing prevalence of chronic conditions. However, it is important to emphasize that polypharmacy is not just an issue for the elderly. Further work is required to investigate to what extent provider and/or health system-level factors can further predict polypharmacy.