1. Introduction
Myoepithelial carcinoma, also known as malignant myoepithelioma, is a rare tumor, which was first described by Stromeyer et al. in 1975 (1). These tumors have been reported to arise from the salivary glands or other areas, such as cutaneous, subcutaneous, and deep soft tissues of the head and neck regions and upper and lower extremities (2, 3). Myoepithelial carcinomas typically occur in the salivary glands, and most commonly, in the parotid gland (4). Clinically, the majority of patients present with a palpable, usually painless mass (5). The standard treatment involves wide surgical resection with clear margins.
Due to the possibility of recurrence or metastasis following surgery, radiation therapy is recommended (4). Myoepithelial tumors of soft tissue show an equal distribution in males and females, with the highest incidence reported in young to middle-aged adults (5). According to the literature, myoepithelial carcinoma recurs in 40% of patients and metastasizes in 22% of cases (6). The common sites of metastasis include the lungs, liver, bone, and soft tissue (7).
Herein, we report a rare case of myoepithelial carcinoma in a 64-year-old woman with pain in the right ankle. To the best of our knowledge, this is the second report of ankle myoepithelioma in the English literature and the first one in the field of radiology. In this case report, the radiological features, including ultrasonography and magnetic resonance imaging (MRI) findings of the patient, as well as the pathological features of myoepithelial carcinoma of the ankle, were described.
2. Case Presentation
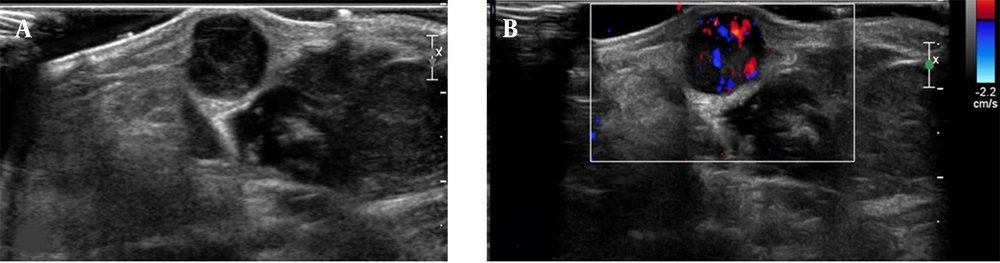
A 64-year-old woman with a history of painful palpable mass in her right ankle over the past three years visited our clinic. Physical examination revealed a bluish colored lump on the medial malleolus (Figure 1). The lesion was also firm and fixed. She complained of an itching sensation with mild pain. Besides, she had high blood pressure and hyperlipidemia and was on medication. She had no trauma or surgical history. The subsequent ultrasonography (Figure 2) indicated a 1 cm hypoechoic mass in the subcutaneous fat layer in the medial malleolar area. The mass exhibited a solid portion and vascularity on color Doppler images.
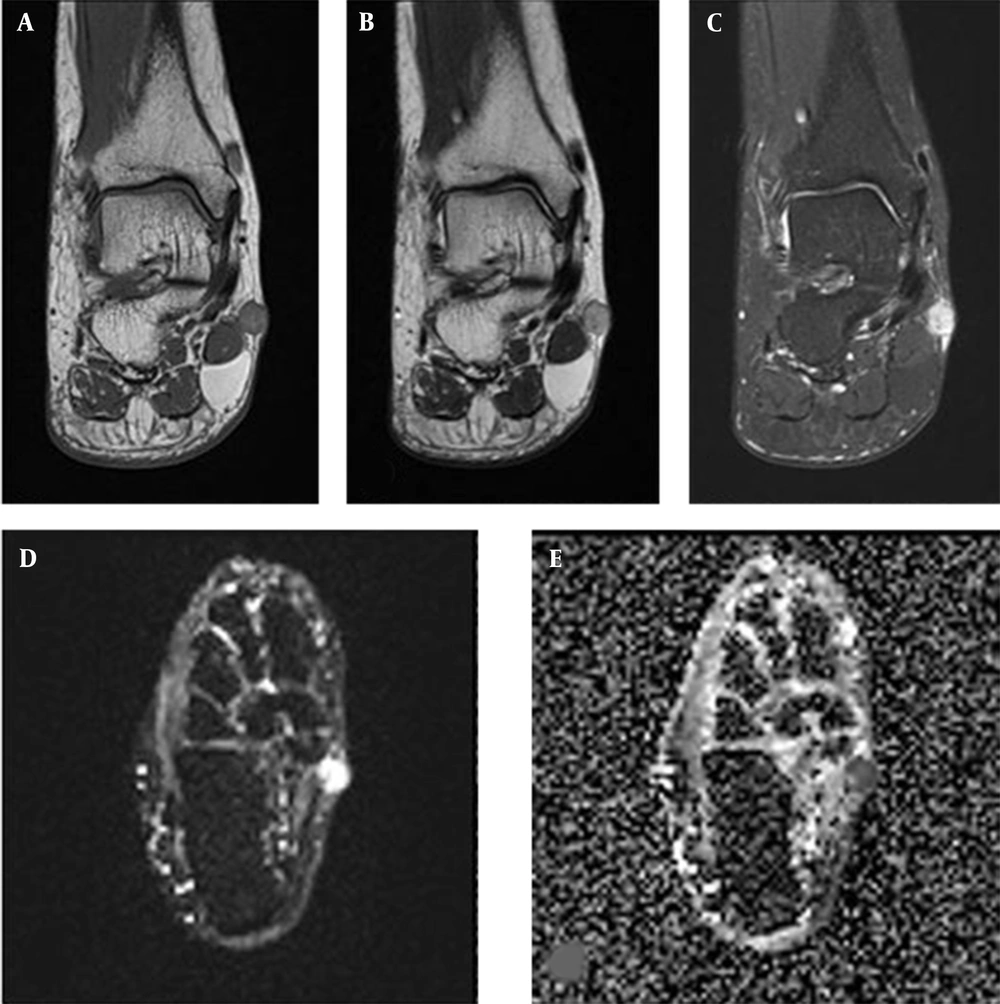
The ankle MRI (Figure 3) revealed a 1 cm, well-defined nodular lesion on the medial malleolus of the right ankle. The lesion showed hypersignal intensity on T2-weighted images and intermediate signal intensity on T1-weighted images. Following gadolinium injection, the lesion showed homogeneous enhancement on fat-suppressed post-contrast T1-weighted images. High b-value (b = 1000) diffusion-weighted imaging (DWI) showed restriction of the lesion with a low apparent diffusion coefficient (ADC). There were no adjacent soft tissue changes or skin involvement.
The MRI of the right ankle for further evaluation of the painful soft tissue mass. Coronal T1-weighted image (A), T2-weighted image (B), and contrast-enhanced fat-suppressed T1-weighted image (C), show a 1 cm, well-defined mass with iso-signal intensity on T1-weighted images and high signal intensity on T2-weighted images. After contrast injection, the lesion shows homogenous enhancement. The high b-value (b = 1000) diffusion-weighted image (D), shows restricted diffusion with a low apparent diffusion coefficient (ADC) (E).
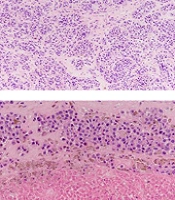
The patient underwent surgical excisional biopsy. The tumor was arranged in nests or large sheets with epithelioid cells in collagenous stroma. Tumor cells showed high-grade cytologic atypia and frequent mitoses. Based on immunohistochemistry, the tumor cells were strongly positive for S-100 protein (Figure 4). According to the histological findings, the tumor was diagnosed as myoepithelial carcinoma.
The histological features of the specimens. The tumor is arranged in nests or large sheets with epithelioid cells in collagenous stroma (A) (hematoxylin and eosin [H&E] staining, 100× magnification). The tumor cells are pleomorphic epithelioid or plasmacytoid cells with high-grade cytological atypia and frequent mitoses (B) (H&E staining, 400 × magnification). Also, tumor necrosis can be found (C) (H&E staining, 200 × magnification). Immunohistochemical staining for S-100 protein is strongly positive (D) (400 × magnification).
3. Discussion
Myoepithelial carcinoma is a rare tumor, which most frequently occurs in the parotid glands (4). The most common site of soft tissue myoepithelial carcinoma is the lower extremity, as reported in 38% of cases (8). The recurrence rate of soft tissue myoepithelial carcinoma is known to be as high as 37 - 42% following treatment (8, 9). Since soft tissue myoepithelial carcinoma commonly presents as distant metastasis and develops in the lungs, kidneys, brain, and skin, chest computed tomography (CT) and abdominal CT scan or positron emission tomography (PET)/CT can be useful for the initial staging workup (9-11).
The imaging characteristics of myoepithelial tumors in soft tissues are not well-known due to their rarity. Some studies have reported that soft tissue myoepithelial tumors are relatively well-defined lobulated masses with heterogeneous enhancement on contrast-enhanced CT scans. On MRI, tumors show low to intermediate or high signal intensity areas, representing hemorrhage on T1-weighted images and heterogeneous high intensity areas with low-signal-intensity internal septa on T2-weighted images (12, 13). Since there is an overlap between benign and malignant lesions without specific imaging findings, pathological confirmation is necessary for diagnosis.
In our case, the mass showed hypersignal intensity on the T2-weighted image and intermediate signal intensity on the T1-weighted image; these results appear to be similar to a previous report. On DWI, our patient showed diffusion restriction; although little is known, this finding is consistent with the results of a previous study (14). According to the literature, myoepithelial carcinoma of the tibia shows restricted diffusion, reflecting a large cellular microenvironment on DW-MRI with a low ADC. These findings suggest that DWI and ADC values can be used for differentiation of benign and malignant myoepithelial tumors (14).
Regarding treatment, surgical excision is the first option. Chemotherapy may be used for metastatic myoepithelial carcinoma (10). Radiation therapy can be used as the first-line treatment when surgery is contraindicated or as an adjuvant treatment when the risk of recurrence or metastasis is high (4). However, a study reported that radiation therapy is not effective for a recurrent or metastatic disease (15).
In conclusion, myoepithelial carcinoma of the ankle is an uncommon phenomenon, and there are few published reports describing the imaging features of myoepithelial carcinoma. We hope that our case can help radiologists diagnose myoepithelial carcinoma in practice.

![The histological features of the specimens. The tumor is arranged in nests or large sheets with epithelioid cells in collagenous stroma (A) (hematoxylin and eosin [H&E] staining, 100× magnification). The tumor cells are pleomorphic epithelioid or plasmacytoid cells with high-grade cytological atypia and frequent mitoses (B) (H&E staining, 400 × magnification). Also, tumor necrosis can be found (C) (H&E staining, 200 × magnification). Immunohistochemical staining for S-100 protein is strongly positive (D) (400 × magnification). The histological features of the specimens. The tumor is arranged in nests or large sheets with epithelioid cells in collagenous stroma (A) (hematoxylin and eosin [H&E] staining, 100× magnification). The tumor cells are pleomorphic epithelioid or plasmacytoid cells with high-grade cytological atypia and frequent mitoses (B) (H&E staining, 400 × magnification). Also, tumor necrosis can be found (C) (H&E staining, 200 × magnification). Immunohistochemical staining for S-100 protein is strongly positive (D) (400 × magnification).](https://services.brieflands.com/cdn/serve/3170b/b14906458e85ddf498463cb803cbca77008e6951/iranjradiol-133421-g004-F4-preview.webp)