1. Background
The acetabular and proximal femoral bone abnormalities include developmental abnormalities, such as pistol-grip deformity, coxa profunda, femoral head-neck junction bone protrusion and acquired abnormalities, such as acetabular/labral ossification, acetabular cysts, acetabular osteophytes, herniation pits (HPs) of femoral neck, hip joint space narrowing (1-3). All of these bone abnormalities are very common in the clinical practice, and have a close relationship with femoroacetabular impingement (FAI) (4). The abnormal impact of the acetabular labral margin and the proximal femur often occurs at the end of the hip joint movement, which can be induced by certain specific positions of hip activities (5-7). “Drehmann’s” sign is an important sign and is positive if there is an unavoidable passive external rotation of the hip while performing hip flexion (6, 8). According to the “Drehmann’s” sign we designed a special hip functional position in full flexion abduction and external rotation with the patient in the supine position. In this special functional position, the abnormal contact between skeletal prominences of the acetabulum and the femur during hip joint motion could be induced, which caused the patient’s symptoms and limited the range of hip motion, furthermore we can observe the bone changes caused by this impact.
However, conventional radiography at special functional position leads to a more overlap of the femoral head-neck junction, and the bone abnormality is obscured. Therefore, hip digital tomosynthesis in special functional position (DT -SFP) has been designed for investigation of hip joint. DT is a newly digitalized sectional imaging technology developed in recent years and has greater advantages over conventional radiography in the imaging quality and diagnostic accuracy in showing some complex anatomical structures (9, 10). Thus, the application of DT for skeletal imaging has gradually attracted more and more attention in recent years (11-13). Based on this, we assume that the combination of DT and special functional position as DT-SFP will play a greater role in detecting acetabular and proximal femoral radiographic abnormalities.
2. Objectives
This prospective study aims to evaluate the diagnostic value of DT-SFP in detecting acetabular and proximal femoral radiographic abnormalities compared with conventional radiography.
3. Patients and Methods
3.1. Clinical Data
From May 2014 to January 2016, 94 patients (age range, 22 - 56 years; mean age, 34.4 years) were included in this prospective study. These patients included 43 men and 51 women. Patients presented with groin pain and/or deep hip pain with hip rotation, in the sitting position, during or after sports activities and while changing hip position. The institutional review board approved our study and written informed consent was obtained from all patients. All the patients included in our study had no history of hip trauma or diseases such as acetabular dysplasia, avascular necrosis of the femoral head, and ankylosing spondylitis. The clinical examination showed positive “Drehmann’s” sign.
3.2. Conventional Radiography
Standardized conventional anteroposterior pelvic radiographs were obtained while the patient was in supine position by using a commercial digital radiography system (Discovery XR650; GE Healthcare, Little Chalfont, Buckinghamshire, England). Both the legs were internally rotated by approximately 15° to adjust for femoral neck antetorsion (14).
3.3. DT-SFP
After conventional radiography, DT-SFP was performed using the same digital radiography system (Volume RAD; GE Healthcare).The patient was in the supine position with extreme flexion abduction and external rotation of the hip. The system produced sixty low-dose projection images in a period of about 10 s, using a tube voltage of 85 kV and a tube current of 160 mA. Matrix for 1024 × 1024 of the image, image reconstruction slice thickness was 1 mm.
3.4. Image Analysis
The set of images of the conventional radiography and DT-SFP were independently analyzed by two experienced musculoskeletal radiologists. Radiographic abnormalities for each hip were recorded and assessed. If the opinions conflicted, the abnormalities were judged again by the third senior experienced musculoskeletal radiologist. Readers were blinded to the clinical findings and readings were performed over a period of 2 weeks. Both the sets were randomly presented and a total of 10 acetabular and proximal femoral radiographic abnormalities were recorded which included 5 developmental abnormalities and 5 acquired abnormalities (Table 1) (4-6, 15).
| Radiographic Abnormalities | DT-SFP | Conventional Radiography | Pb |
|---|---|---|---|
| Developmental abnormalities | |||
| Coxa profunda | 41% (51/124) | 41% (51/124) | 1.000 |
| Cross-over sign | 0 | 11% (14/124) | - |
| Femoral head-neck junction bone protrusion | 33% (41/124) | 10% (12/124) | 0.000 |
| Posterior wall sign | 8% (10/124) | 8% (10/124) | 1.000 |
| Pistol-grip deformity | 0 | 22% (27/124) | - |
| Acquired abnormalities | |||
| Acetabular/labral ossification | 21% (26/124) | 9% (11/124) | 0.000 |
| Acetabular cysts | 17% (21/124) | 7% (9/124) | 0.000 |
| Acetabular osteophytes | 40% (49/124) | 31% (38/124) | 0.001 |
| Herniation pits of femoral neck | 35% (43/124) | 21% (26/124) | 0.000 |
| Hip joint space narrowing | 6% (8/124) | 6% (8/124) | 1.000 |
Abbreviation: DT-SFP, digital tomosynthesis at special functional position.
aValues are expressed as NO (%).
bP values were estimated by McNemar test.
3.5. Statistical Analysis
The detection rates of acetabular and proximal femoral radiographic abnormalities showed by DT-SFP and conventional radiography were statistically analyzed by McNemar’s chi square test. SPSS software (version 16.0; SPSS Inc., Chicago, IL, USA) was used for statistical analysis and P < 0.05 was considered to be significant. As the cross-over sign and pistol-grip deformity were only visible in the conventional radiographs, these two radiographic abnormalities were not included to be analyzed.
4. Results
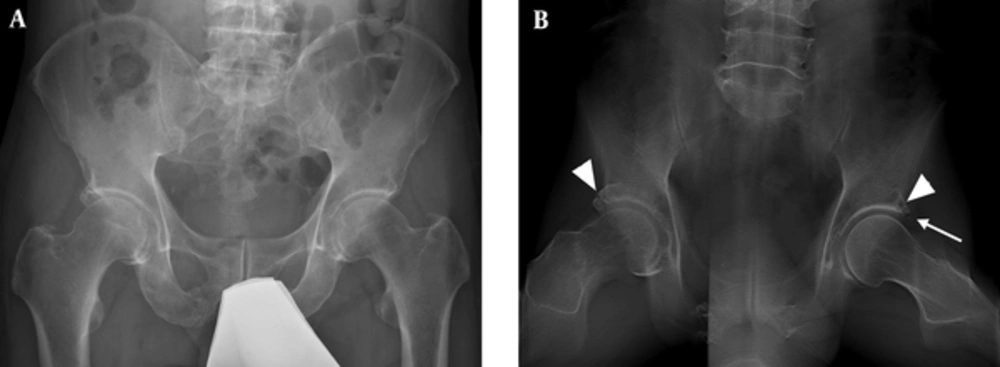
There were 124 symptomatic hips in a total of 94 patients. The statistical analysis for the detection rates of abnormalities in DT-SFP and conventional radiography are summarized in Table 1. Several acetabular and proximal femoral radiographic abnormalities were statistically different between DT-SFP and conventional radiography set of images including HPs (Figures 1 and 2), acetabular/labral ossification (Figure 3), femoral head-neck junction bone protrusion (Figure 3), acetabular cysts (Figure 4) and acetabular osteophytes. The detection rates of these radiographic abnormalities in DT-SFP were higher than in the conventional radiography (P < 0.05). The position of HPs and the sharp edge of the acetabulum correspond to each other as showed in DT-SFP images. The other osseous abnormalities of the acetabulum are located on the outer edge, and this is the area where the acetabulum and the proximal femur come in contact with each other in the special functional position. Differences in the detection of coxa profunda (Figure 1), hip joint space narrowing, posterior wall sign between DT-SFP and conventional radiography set were not statistically significant (P > 0.05). In addition, due to the position of the patient, cross-over sign and pistol-grip deformity were only visible in the conventional radiographs.
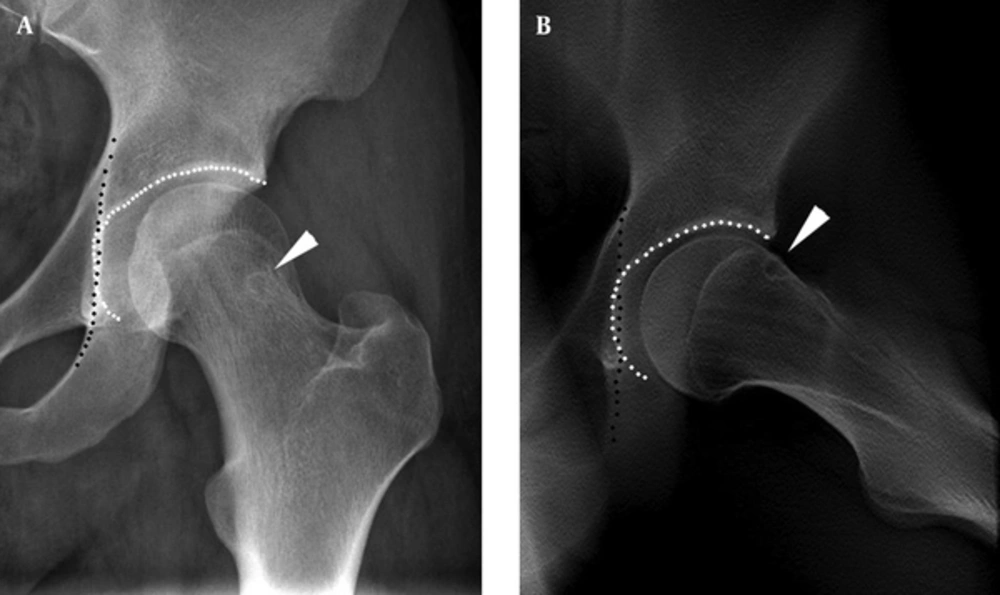
A 31 year old male with left groin pain for 2 years. A, Conventional radiograph shows a round lucency in the femoral neck (arrowhead), and acetabular fossa (white dotted line) touching the ilioischial line (black dotted line), which refers to coxa profunda; B, Digital tomosynthesis at special functional position (DT-SFP) image shows an oval lucency in the anterosuperior femoral neck (arrowhead), just corresponding to the outer edge of the acetabulum, and a coxa profunda (black and white dotted line).
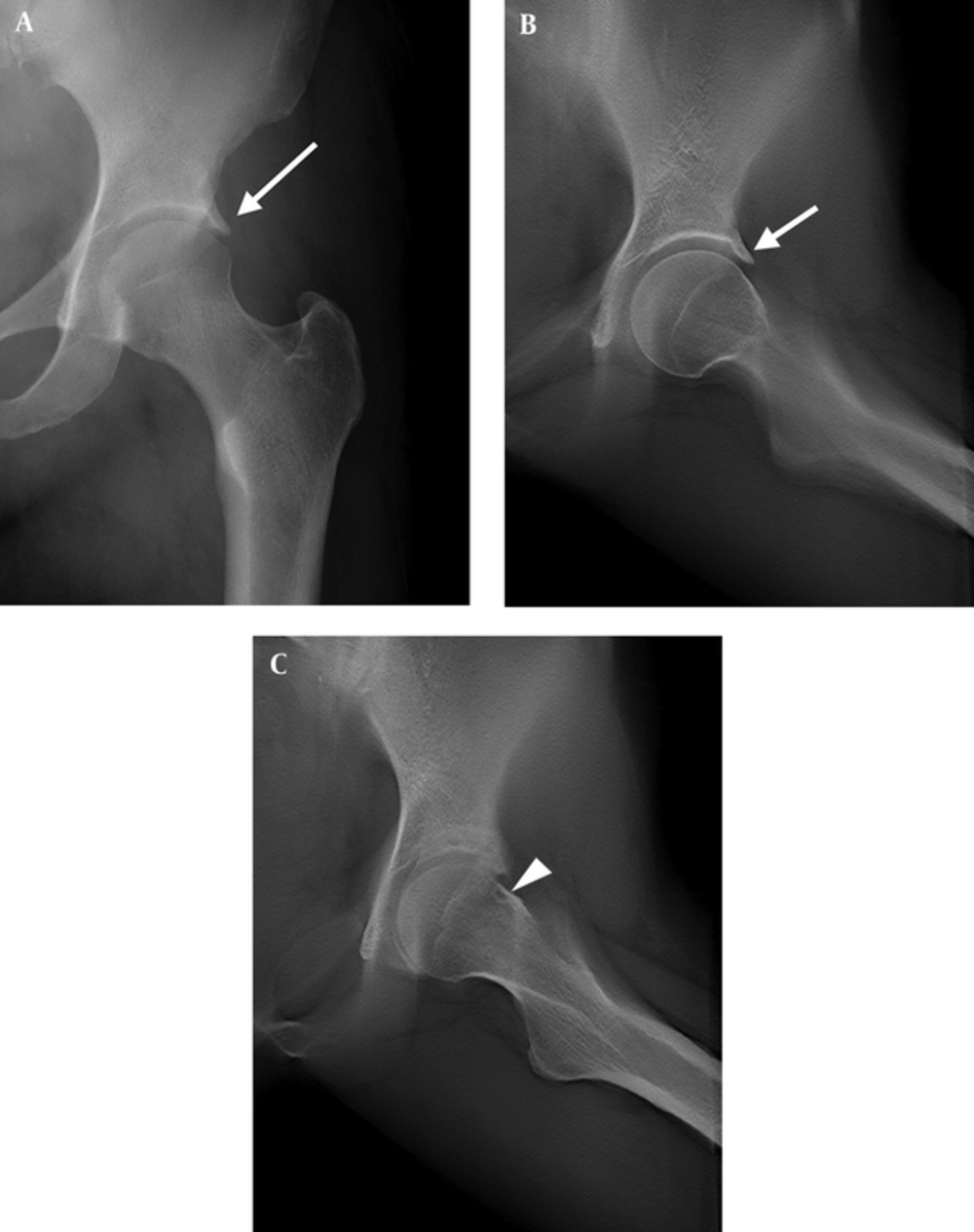
A 55-year-old female with left groin pain for 1.5 years after long distance walking. A, Conventional radiograph shows coxa profunda and acetabular osteophytes (long arrow) with a sharp edge, and pincer-like deformity; B and C, Digital tomosynthesis at special functional position (DT-SFP) images show sharp osteophytes in the rim of the acetabulum (short arrow) and coxa profunda. Herniation pit is not shown on the conventional radiograph it is clear on DT-SFP located in the junction of the femoral head and neck (arrow head).
A 37-year-old male with left hip pain for eight months. A, Conventional radiograph shows an aspherical femoral head; B, Digital tomosynthesis at special functional position (DT-SFP) shows bony protrusion at the femoral head-neck junction (arrowhead) and a small acetabular labrum ossification (arrow).
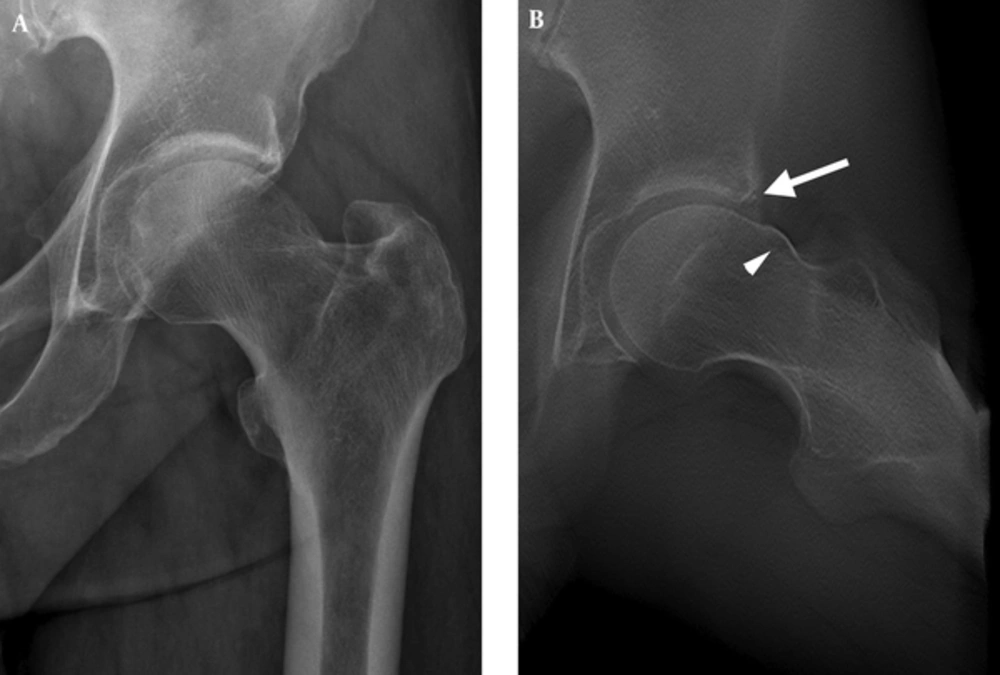
A 43-year-old male with bilateral groin pain for 5 years. A, Conventional radiograph does not show any obvious abnormality; B, Digital tomosynthesis at special functional position (DT-SFP) shows a prominent separated acetabular labrum ossification at the right acetabulum (arrowhead) and a cyst located at the junction of the head and neck in the area contacting with the acetabulum rim (arrowhead) and a very small ossification of labral basis (arrow).
5. Discussion
In this study, we noticed that the detection rates of 5 radiographic abnormalities such as HPs, acetabular/labral ossification, femoral head-neck junction bone protrusion, acetabular cysts, and acetabular osteophytes were higher by DT-SFP than by conventional radiography. Most of the signs with a higher detection rate using DT-SFP were acquired osseous abnormalities except for the femoral head-neck junction bone protrusion. The acquired osseous abnormalities are closely related with an abnormal contact during hip joint motion between the skeletal prominences of the acetabulum and the proximal femur (16-18). The recurrent impingement can lead to microtrauma of abnormal developmental osseous convexities, acetabular labral tear and cartilage damage, that progresses and results in degenerative disease of the hip joint if the underlying cause of impingement is not eliminated (19, 20). In the initial phase of this entity, patients do not have obvious radiographic signs, such as joint space narrowing, osteophyte formation, subchondral sclerosis, or cyst formation (16, 17, 20). Therefore observing the early stage of radiographic features is helpful for the correct diagnosis and evaluation before potential surgical treatment.
When patients with acetabular and proximal femoral radiographic abnormalities complain of groin pain radiating to the lateral thigh, labral tear and cartilage damage might exist and lead to corresponding osseous changes (16, 19, 20). The application of the tomography technology can show the lesion clearly by removing the overlap of the anatomical structures. DT refers to the technique of collecting a number of projection radiographs with very low dose at different angles in order to reconstruct sections of the target (9, 10). These reconstructed sectional images demonstrate much less of the overlying anatomical structures than the conventional radiographs, thus improving detection rate of tiny lesions (9-13, 21).
HPs refers to an oval or round lucency in the anterosuperior aspect of the femoral neck, just distal to the articular surface, and a cortical defect is always found in the side of the articular surface (22). Herniation of synovium or soft tissue into the bone through the cortical defect was previously thought to be the formation mechanism, leading to the alternate name “synovial herniation pit”. In our research the scene of the abnormal impact between acetabular and proximal femur was induced through the special functional position, full flexion abduction and external rotation. The imaging sequence of DT-SFP was from the near detector side to the far detector side and the bone abnormalities can be clearly observed layer by layer in the area of space. On DT-SFP the HPs corresponding to the acetabular/labral ossification, acetabular osteophytes, and acetabular cysts was confirmed. The HPs and the acetabulum abnormalities are just located in the area in which the acetabulum and the proximal femur contact with each other in the special functional position, which represent the abnormal impingement. This is a powerful objective supported by other authors on the theory of HPs at the femoral head neck junction (22).
Hence the results of our research show that conventional radiography is suitable for observation of anatomical abnormalities and obvious osteoarthritis of the hip, but is not suitable for diagnosis of early osteoarthritis. For coxa profunda, hip joint space narrowing and posterior wall sign, DT-SFP and conventional radiography almost show the same demonstrating ability. Therefore, the two imaging techniques have the same efficacy in the detection of these three radiographic abnormalities.
The application of DT-SFP is more convenient and flexible than CT and MRI, with open space, lower radiation dose and medical cost. DT-SFP is suitable for some special positions that could not be met by CT and MRI (except for open MRI) (23). In our research, we use lead barrier shield to protect the gonads during the DT-SFP scan, which can strengthen the radiation protection.
It should be noted that some types of developmental abnormalities such as cross-over sign and pistol-grip deformity cannot be shown on DT-SFP images due to the changing position of the projection. This suggests that conventional radiography is essential and irreplaceable in certain cases for diagnosis of acetabular and proximal femoral radiographic abnormalities. So a combination protocol of conventional radiography and DT-SFP for assessment of acetabular and proximal femoral osseous abnormalities should be taken.
In conclusion, DT-SFP provides a new method of X-ray examination for the assessment of acetabular and proximal femoral bone abnormalities. The diagnostic accuracy of acetabular and proximal femoral radiographic abnormalities is improved through removing overlapping anatomical structures out of the area of interest, and the abnormal impact between proximal femur and the acetabulum could be reproduced by DT-SFP.